“Biologics are becoming more and more routine in everyday practice”
An interview with Richard J. Miron.
Following his recent review in the Journal of Clinical Periodontology on twenty years of Enamel matrix derivative, Dr. Richard J. Miron shares with us in an interview some insights on the past, present and the future of Emdogain® and of biologics in dentistry.
You have recently written a review1 on “Twenty years of enamel matrix derivative: the past, the present and the future”. Can you tell us a little bit about yourself and how you came to publish a review on this topic?
Early in 2007 I began working at the University of Western Ontario (Douglas Hamilton’s lab in London, Canada) on a project funded by the ITI. The purpose of the project was to investigate the role of enamel matrix protein adsorption onto various titanium implant surfaces including smooth, SLA and SLActive surfaces. Unlike many clinicians, my first handling of, and exposure to, Enamel matrix derivative (EMD) was in this in vitro study, contrary to the large majority using the commercially available Emdogain gel for patient treatment. Following this, I was offered a great opportunity by the government of Canada to pursue a PhD at a university of my choosing. Naturally I sought to consider some of the best academic researchers working in the field of implant surface dentistry with EMD. Anton Sculean had been one of the key clinical investigators in the field and had recently become the chairman of the periodontal department at the University of Bern in Switzerland. I therefore decided to move to Switzerland to be part of his team in 2009. Over the years we’ve published over 20 scientific articles together with Dieter Bosshardt and continue to work closely on this topic. Since March 2016, I returned to North America and have been working in the Department of Periodontology at Nova Southeastern University in Fort Lauderdale, Florida. One of the main research interests in my lab remains EMD.
In 2015 at EuroPerio, a group of experts gathered to discuss what has now been 20 years of research with Emdogain. As part of the ceremony and discussions, I was fortunate to have been asked to write a summary review article on the topic, gathering the last 20 years of research on EMD with our group in Bern. Naturally we were instructed to seek and incorporate all the leaders who have contributed to the field of EMPs1 over the past 20 years. We were fortunate to be able to publish the work in the Journal of Clinical Periodontology a few months ago, and the publication has been extremely well received by our collaborators and colleagues internationally.
What is the role of Emdogain® in the field of periodontal regeneration?
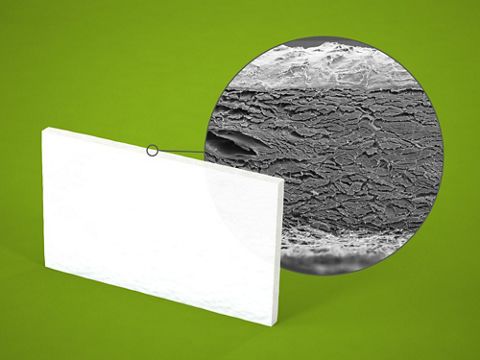
To answer this question, it is first important to understand how EMPs are naturally deposited onto the root surface at an early stage during embryogenesis. Over 20 years ago, a team of researchers in Sweden, including Lars Hammarström, Sven Lindskog and Leif Blomloff, found that EMPs could be utilized as a biological agent capable of periodontal regeneration by studying root formation. However, these reports originated from previous studies conducted some 15 years earlier by Lindskog et al. and Slavkin et al., which reported that certain EMPs (which until then were considered enamel-specific proteins) were deposited onto the surface of developing tooth roots prior to cementum formation and hypothesized their possible role in cementogenesis. The role of Emdogain is therefore to mimic the root surface’s natural formation. EMPs (mainly comprised of amelogenin proteins) are necessary for the formation of a functional periodontal ligament attached via Sharpey’s fibers to alveolar bundle bone and to newly formed cementum during embryogenesis. The use of Emdogain was formulated to mimic this natural process in cases where attachment loss has been observed clinically. Therefore, and owing to its excellent documentation, Emdogain may be utilized as one of the only regenerative modalities demonstrating true periodontal regeneration by initiating a regenerative process supported by histological findings in humans. Today, a number of clinical indications have been performed with Emdogain including, but not limited to, intrabony defect regeneration with/without bone grafts, recession coverage, class II furcation defect regeneration, and soft tissue wound healing.
"Data exists for the use of Emdogain alone for the management of severely compromised situations where initially questionable teeth have been maintained in stable situations for over 20 years following therapy with Emdogain."
How does regenerative periodontal therapy with Emdogain® compare with alternative treatments?
The healing of different types of periodontal defects treated with Emdogain or guided tissue regeneration (GTR) has been the focus of much research in the early 2000s. It was reported in a multitude of studies that application of Emdogain resulted in substantially larger amounts of new cementum, periodontal ligament and bone formation when compared to controls (i.e. flap surgery alone). Moreover, the main findings from these studies revealed that the amount and quality of the newly formed periodontal tissues were comparable between Emdogain and GTR, thus eliminating the need for GTR membranes in such cases. Today, when a clinician is faced with a choice of regenerating contained intrabony defects with either Emdogain or GTR, not only is the procedure simpler and more timely with Emdogain, but the results have also revealed fewer difficulties with Emdogain, mainly due to complications resulting from barrier membrane exposure reported while utilizing GTR.
In regenerative periodontal therapy: when should one use Emdogain® and when should one mix Emdogain® with a bone graft?
Although numerous clinical studies have provided evidence of substantial clinical and radiographic improvements following application of Emdogain alone, concerns have been raised regarding the viscous nature of Emdogain, which may not be sufficient to prevent a flap collapse and maintain space for periodontal regeneration. In order to overcome this potential limitation and improve clinical results, various combinations of Emdogain with barrier membranes and/or grafting materials have been tested. Recent systematic reviews and meta-analyses found that the combination of bone grafting material + Emdogain led to statistically significant better outcomes. Therefore, when I expect Emdogain gel alone will not be sufficient to prevent flap collapse, I utilize a combination approach with a bone grafting material.
"Emdogain was shown to enhance soft tissue wound healing by acting at a cellular and molecular level, for instance by significantly decreasing a variety of inflammatory markers."
Can you tell us more about the soft tissue wound healing indication of Emdogain®?
Emdogain was shown to enhance soft tissue wound healing by acting at a cellular and molecular level, for instance by significantly decreasing a variety of inflammatory markers including interleukin-1b and RANKL, increasing prostaglandin E2 and OPG expression, increasing proliferation and migration of T lymphocytes, inducing monocyte differentiation, increasing bacterial and tissue debris clearance, as well as increasing fibroplasia and angiogenesis by inducing endothelial cell proliferation, migration and capillary-like sprout formation. Furthermore, clinical studies have reported improvements in pain levels and increases in angiogenesis, all supporting its use in wound healing. It remains interesting to point out that EMPs have been studied under the trademark name Xelma for the treatment of complicated foot ulcer regeneration in diabetic patients further demonstrating its role in wound healing.
"To this day EMD remains a ‘gold-standard’ for regeneration of periodontal defects, and investigators from around the world have confirmed these findings."
Twenty years after its launch on the market, Emdogain® is still going strong. Why do you think that is?
In the early years, it was quite new to the dental field to utilize growth factors either from recombinant sources or derived from animal products, and this initiation was perceived with caution. Due to the substantial number of clinical studies and excellent documentation of its long-term safety, Emdogain has now been studied extensively in regenerative dentistry. Of the other growth factors currently available for dental use, recombinant human BMP2 cannot be utilized for periodontal regeneration due to the risk of ankylosis. The use of rhPDGF has had some success for intrabony defect regeneration however there is limited supply of clinical studies validating its use and the cost associated with its use is much higher without documented improvements in clinical parameters. Therefore, to this day EMD remains a ‘gold-standard’ for regeneration of periodontal defects, and investigators from around the world have confirmed these findings.
"It is a very exciting time to be an investigator in the field of regenerative dentistry, and I’m looking forward to gaining more insight into this topic for years to come!"
Where do you see the future of EMD?
Biologics are becoming more and more routine in everyday practice, and I expect this trend to continue in the future as more and more clinicians become aware of the published literature as well as the ease of use/handling of these regenerative materials. It is important to note now that long-term data exists for the use of Emdogain alone for the management of severely compromised situations where initially questionable teeth have been maintained in stable situations for over 20 years following therapy with Emdogain. As clinicians, it should always be our primary objective to maintain natural teeth in the dentition especially when long term data exists that support certain therapies. I am looking forward to the availability of Osteogain for clinical use. This liquid formulation of EMD has been shown to make the coating of bone graft with EMD easier and leads to better protein adsorption not only on the surface of bone grafting materials but also within the interior of bone grafts. I would expect that the additional advantage of having an osteopromotive agent would further enhance the speed and quality of new bone formation but this remains to be investigated. It also interests me to discover how Osteogain will perform in pure bone regeneration procedures when compared to other growth factors that are commercially available in dentistry such as bone morphogenetic proteins and platelet-derived growth factor. Needless to say, it is a very exciting time to be an investigator in the field of regenerative dentistry, and I’m looking forward to gaining more insight into this topic for years to come!