Mucosal® tissue thickening around bone-level implants
A clinical case report by Algirdas Puišys, Lithuania
A 54-year old patient with a missing tooth 3.6 came to our clinic and asked for a restoration of an implant-borne crown. He demonstrated good oral and systemic health; no significant health problems that might influence the treatment were marked. Intraorally, the tooth gap in region 3.6 was noted. The alveolar ridge was slightly flattened and a width of the fixed, keratinized mucosa of approximately 7 mm was observed (Figs. 1, 2).
Treatment procedure
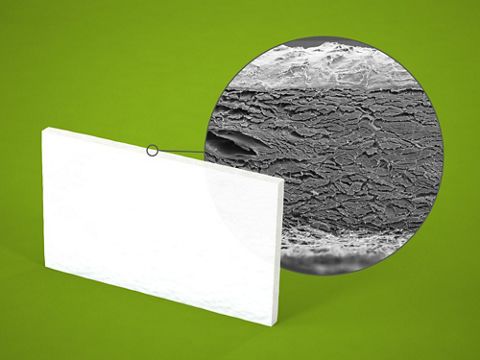
The treatment plan included the placement of a Straumann® Bone Level Implant and, if necessary, a simultaneous thickening of the peri-implant mucosa. Mucosal thickness has been shown to be an important factor in the etiology of early crestal bone loss around dental implants. A clinical study demonstrated that a mucosal thickness of 2 mm or less increased the risk of crestal bone loss within the first year after implantation . Consequently, in cases of thin biotypes, we perform a thickening of the soft tissue by application of the acellular porcine collagen matrix botiss mucoderm®. The matrix is applied instead of an autogenous transplant to spare the patient the harvesting from the palate.
Surgical procedure
After local anesthesia, a crestal incision in region 3.6 and a sulcular incision from 3.5 to 3.7 were performed and a full-thickness flap was raised. A vertical thickness of the mucosal tissue of 2 mm was measured with a periodontal probe (Fig. 3), indicating the augmentation of the peri-implant mucosa. The bone was prepared and a Straumann® Bone Level Implant (Regular Neck , ∅ 4.8 10 mm, SLActive®) was placed (Figs. 4, 5). After implant placement, the crestal bone around the implant was contoured using a straight hand piece with round bur, and the healing cap was screwed down. The botiss mucoderm® collagen matrix was rehydrated in sterile saline for about 10 minutes to ensure a sufficient flexibility of the graft, and then perforated. After that, the matrix was pulled over the healing cap and placed in direct contact with the bone (Fig. 6). Finally, the margins of the flap were adapted and sutured with Assucryl 4/0, leaving the healing abutment open (Fig. 7).
Prosthetic procedure
The sutures were removed one week after the surgery (Fig. 8). At the same time, a perpendicular dental radiograph was taken, showing the implant in correct prosthetic position (Fig. 9). After four months, a wider standard healing abutment was screwed in to create optimal soft tissue conditions for the forthcoming prosthetic restoration (Fig. 10). The healing abutment was removed two weeks later. The mucosal appearance indicated stable and healthy soft tissue around the implant, satisfying biological width and a smooth emergence profile (Fig. 11). An impression was taken. One month later, the ceramic crown was integrated and cemented (Figs. 12 – 14).
Final result
The final prosthetic restoration shows an optimal emergence profile supporting good hygiene. The patient is very satisfied with the esthetic result and the increased width of the peri-implant mucosa will be helpful to maintain the stability of the crestal bone.
Findings
From a prospective controlled clinical study, the following observation was reported: in cases with a tissue thickness at the crest of 2 mm or less, all implants – irrespective of their position to the bone level – developed a crestal bone loss within one year. In cases of a low vertical soft tissue thickness of 2 mm or less, the placement of an acellular collagen matrix derived from porcine dermis (botiss mucoderm®) resulted in increase of peri-implant soft tissue volume and therefore helped to maintain crestal bone stability. In comparison with thin biotypes, significantly less bone loss is being observed around bone-level implants placed in naturally thick mucosal tissues. Therefore, the augmentation of thin soft tissues with a xenogenic collagen matrix (like botiss mucoderm®) during implant placement may be a way to reduce crestal bone loss.