Straumann® Tissue Level hydrophilic implants in the esthetic zone – a 10-years follow-up
A clinical case report by Shakeel Shahdad, UK
Successful restoration of a single tooth edentulous space in the anterior maxilla is not only dependent upon long term osseointegration, but achieving and maintaining optimal esthetic outcome is profoundly desirable. It is well established that bone volume reduction occurs after tooth extraction and as a result bone augmentation, either simultaneously or as a two-staged procedure, may be necessary for implant-supported restorations.
There continues to be a debate whether Tissue Level (TL) implants are indicated in esthetic zone with
This case report presents a 10-year outcome of a maxillary anterior tooth with a circumferential bone defect around the implant which was successfully replaced with Straumann® SLActive Tissue Level implant.
Initial situation
A 20-year-old male patient presented with an infection associated with #11. A previous history of sports injury resulting in root canal treatment and post-crown ten years earlier was reported.
Clinical examination revealed root fracture and chronic radicular abscess within middle 3rd of the root between #11 and #12. The coronal portion of #11 had extruded resulting in a favourable coronally positioned gingival zenith (Fig. 1). Probing pocket depth of 7mm was noted on the palatal aspect. A midline diastema was present. The radiograph confirmed the root fracture with a radiolucent halo around the root and the prognosis was deemed to be hopeless.
Treatment planning:
The patient expressed a preference for replacement of the tooth with a dental implant. Type 2 implant placement protocol was chosen and simultaneous guided bone regeneration with bovine deprotienized bone and porcine collagen membrane was consented for. A provisional removable acrylic denture was planned as an interim prosthesis.
Surgical procedure:
After extraction of the crown and the fractured apical root fragment (Fig. 2), exploration of the socket confirmed lack of labial (facial) bone with a crater type bone defect at the crestal aspect. A bovine hemostatic collagen plug was placed and the socket was allowed to heal.
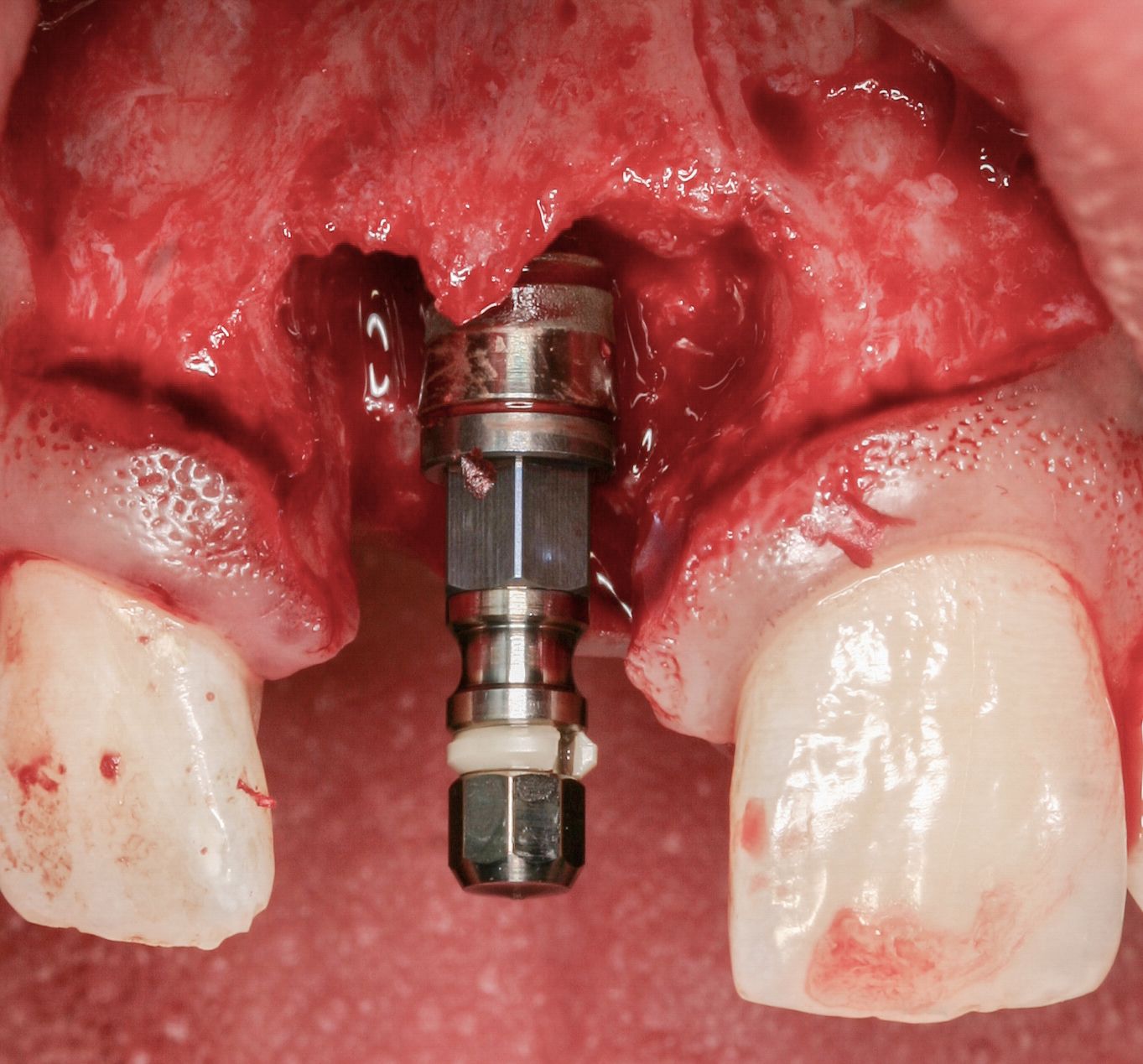
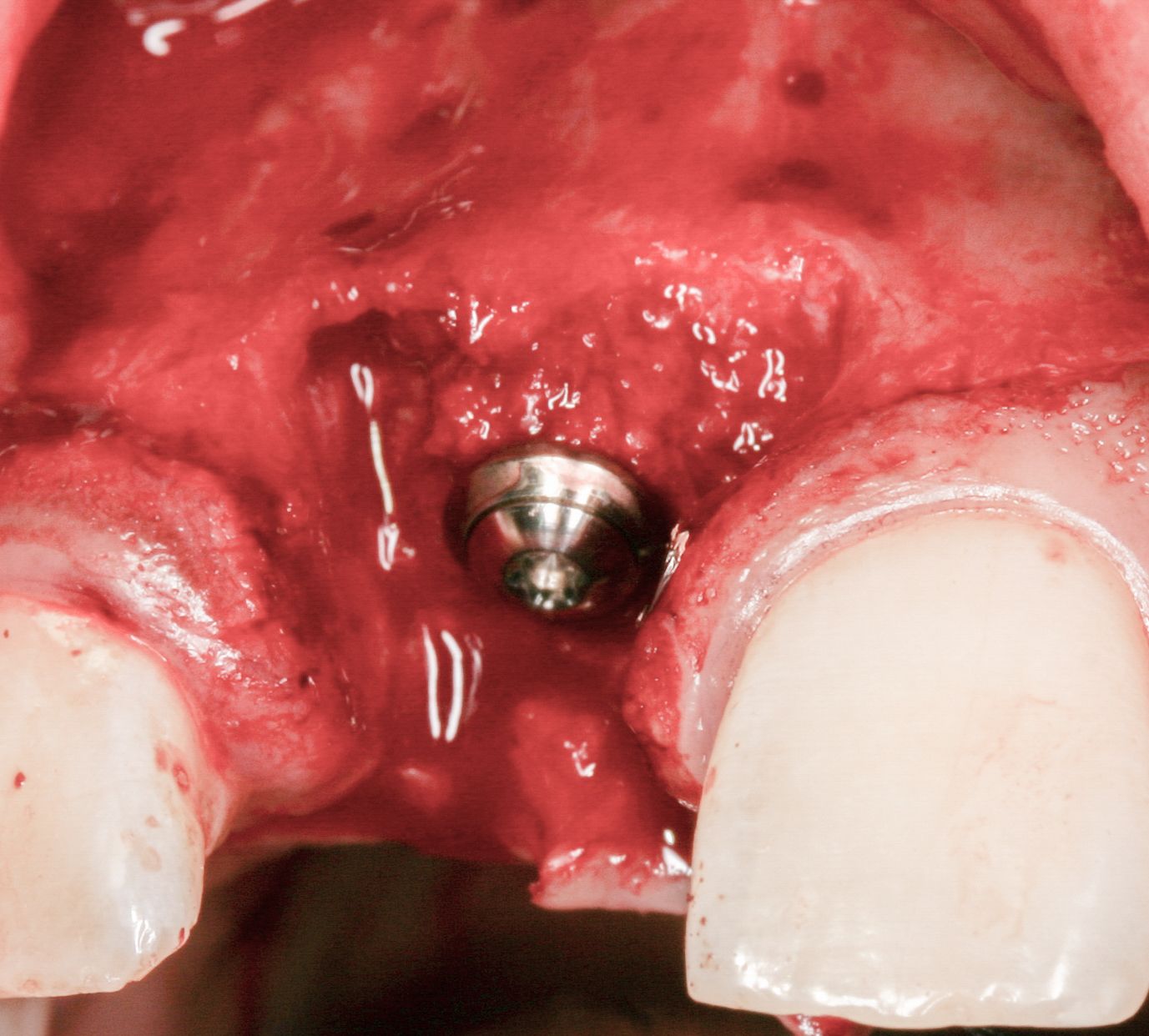
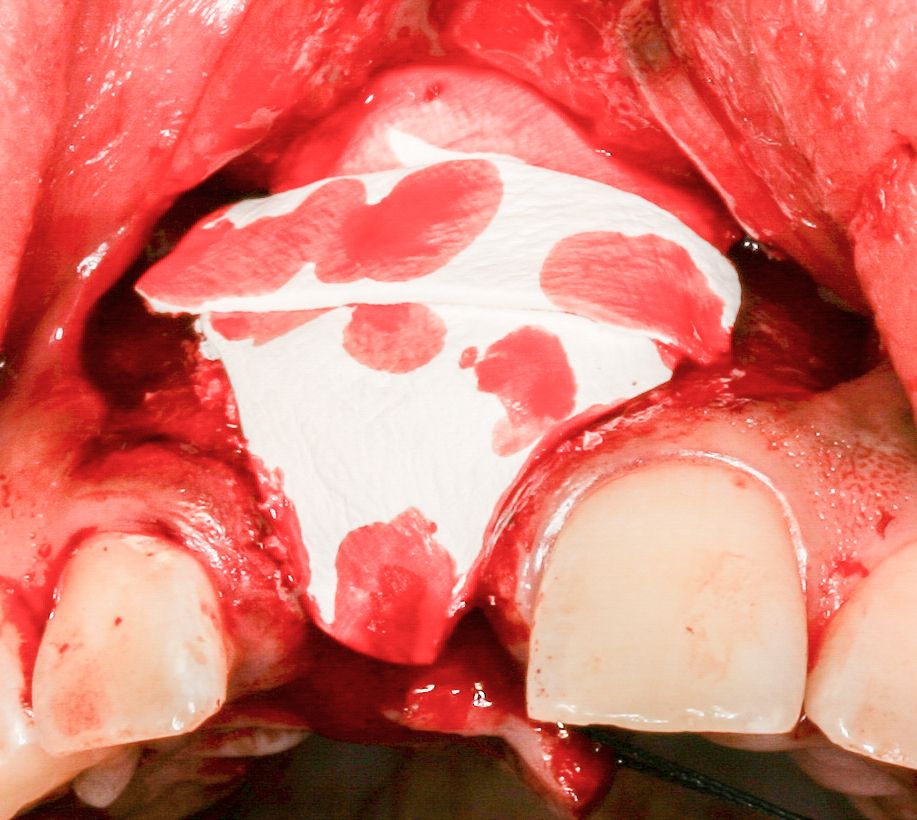
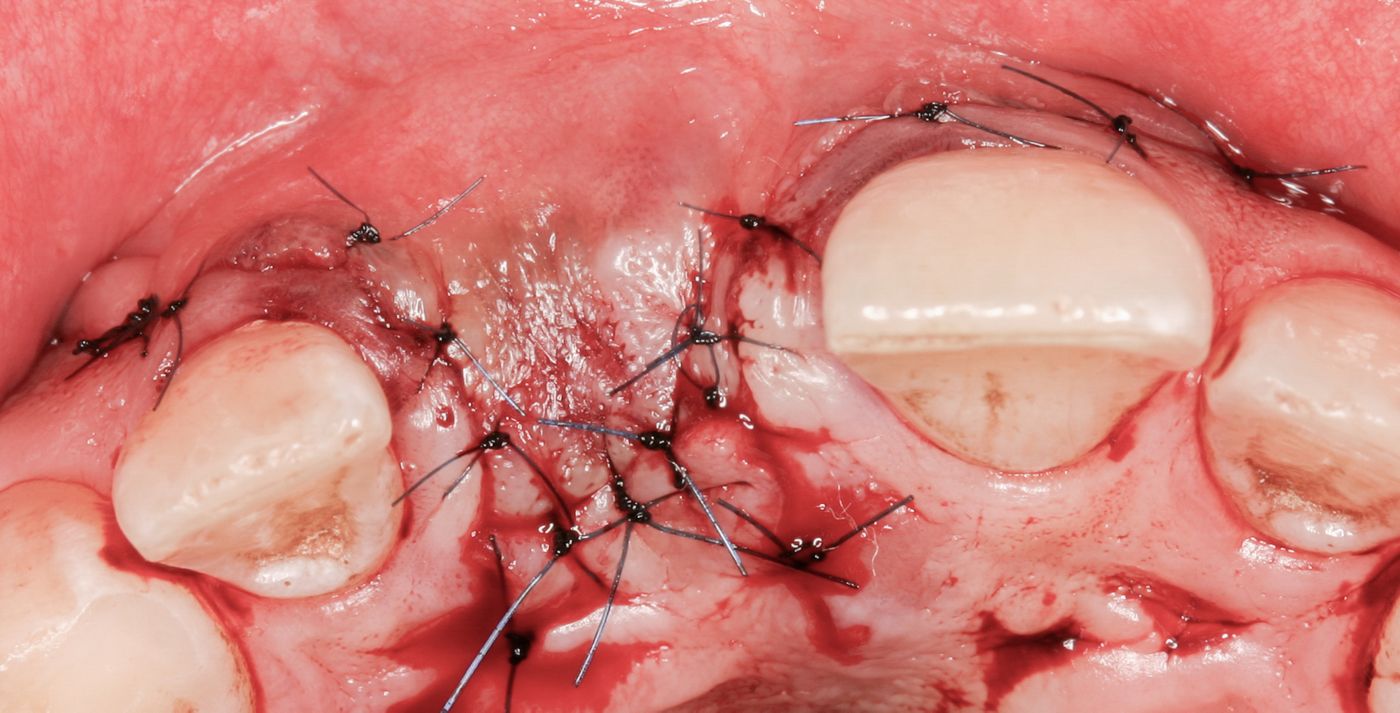
After six weeks healing (Fig. 3a-b) a curvilinear, papilla preserving incision was made. A circumferential bone defect with a broad base but limited to the coronal aspect was encountered. (Fig. 3c). The granulation tissue was thoroughly debrided to leave a clean bone surface. Implant site was prepared in an ideal 3-dimensional position for a screw-retained restoration (Fig. 3d). A Straumann Tissue Level design Tapered Effect SLActive implant was placed with adequate primary stability. The bone defect was grafted with autogenous bone shavings harvested locally followed by deproteinised bovine bone and finally covered by porcine collagen membrane (Fig. 3e-3g). The implant was submerged after achieving a tension free primary closure of flaps (Fig. 3h). Implant exposure was carried out 3 months later and a bevel healing abutment of 3.5mm height was placed.
Prosthetic procedure:
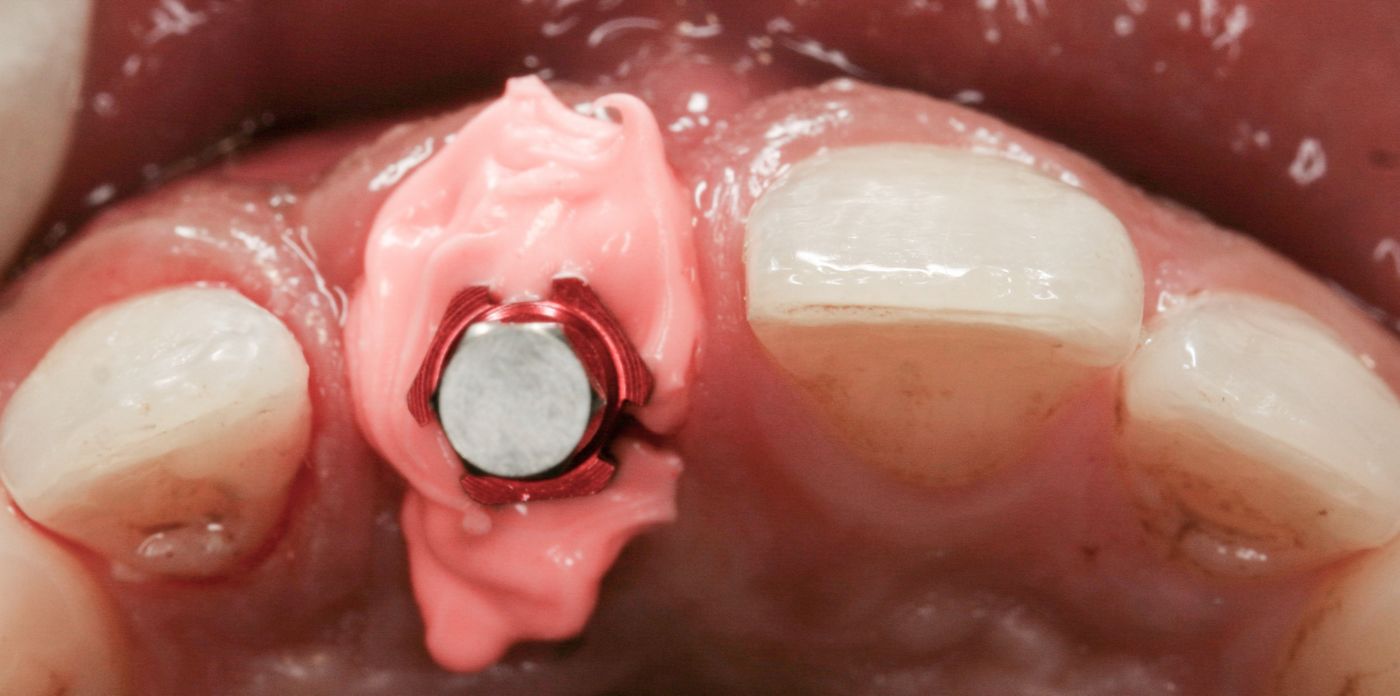
A provisional screw retained crown was used for peri-implant soft tissue manipulation to idealise the pink esthetics (Fig. 4a). After the first review, the contour of the crown was modified to further shape the tissues (Fig. 5a-5e). At the next visit, the soft tissues were deemed to be ideal (Fig. 6a) and a new impression for the definitive crown was recorded with a customized impression coping using addition cured silicone bite registration (Fig. 7a-b) material followed by a conventional impression using addition cured light- and heavy-body silicone impression material. A castable Synocta abutment was waxed-up, cast in semi-precious metal followed by layering with feldspathic porcelain (Fig. 8a-8b). A one-piece screw retained crown was tightened to 35Ncm (Fig. 9a-9b).
Treatment Outcome:
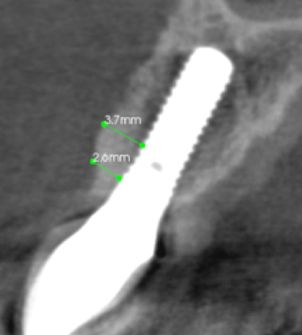
A CBCT scan taken after 5y (Fig. 10-10a) confirms successful bone regeneration which is translated in stable pink aesthetics at 5y (Fig. 11) and maintained after 10y (Fig. 12a-12b). The patient remains delighted with a successful aesthetic outcome.
Conclusion:
This case illustrates successful use of Tissue Level design, hydrophilic SLActive surface implant in achieving and maintaining ideal aesthetic with a long-term follow up of 10 years.
Acknowledgement:
The author acknowledges Mr Alaa Abou Hassan, Chief Ceramist at Ceramic Studios, London, who carried out all the technical aspects of this case.