Abutment selection and long-term success
Julia-Gabriela Wittneben on indication-based abutment selection
The selection of the implant abutment for each individual patient case is an important part of the implant-prosthetic treatment phase. Long-term clinical studies on fixed implant-supported reconstructions show low technical complication rates regarding the abutment itself [1]. In this article, Julia-Gabriela Wittneben discusses different implant abutment types, the various abutment materials, and their clinical indications. A clinical case presenting step-by-step the treatment of a single edentulous gap with an all-ceramic screw-retained implant crown is shown here.
1. Implant abutment types
Implant abutments can be either standard or customized (Fig. 2). The use of a standard abutment is indicated if the implant is placed in an almost ideal prosthetic position. The advantages of standard abutments are time efficiency in the overall treatment and therefore shortening of the technical manufacturing time. Divergences between implants supporting multi-unit prostheses can be corrected with angled standard abutments. In the esthetic zone, it is important that the collar height of a prefabricated abutment is not a uniform 360 degrees, as the interproximal position of the crown margin would be placed too far submucosally. Therefore, the ideal design of a standard abutment should be similar to a tooth preparation, following the contour of the gingival margin2 (Fig. 1). Clinical limitations exist regarding the position of the implant in a vertical dimension. If the implant is placed too apically, standard abutments are not indicated, especially for screw-retained reconstructions, as they do not provide enough support for the veneering ceramic.
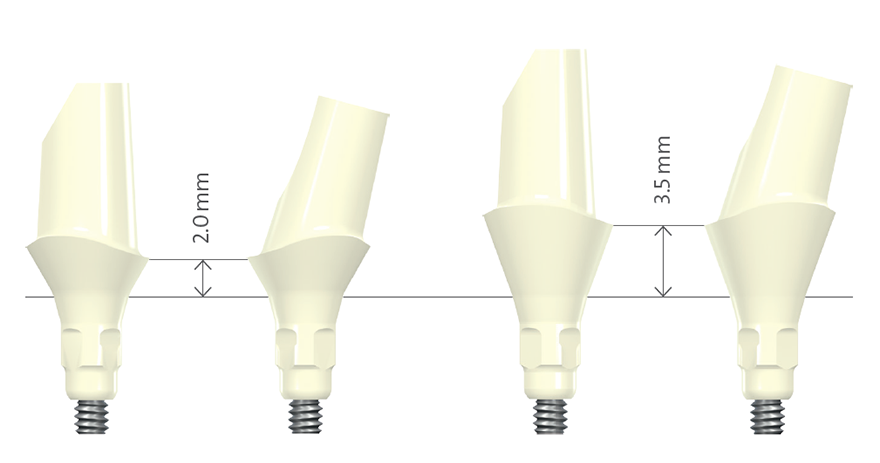
Fig. 1: Standard abutments made of zirconium dioxide
Customizing an abutment gives the clinician the freedom to individualize its position and angulation. In the case of a bone level implant, it is also possible to individualize the emergence profile and future crown margin position of the final restoration. It allows abutments to be designed to provide optimal support for the veneering ceramic material, especially for screw-retained reconstructions. Individualization may be achieved using CAD/CAM technology, gold abutments produced with traditional lost-wax casting methods, or titanium base abutments (Fig. 2). Customized abutments manufactured via CAD/CAM can be made of titanium or zirconium dioxide for bone- and tissue-level implants. They can be used for cement- or screw-retained single crowns or cement-retained bridges. The benefits of the CAD/CAM abutment include the possibility of using a high-performance ceramic material, which again offers many advantages, especially in esthetic sites. In patients with a thin tissue biotype, no grayish shining-through will be visible with a white-colored abutment. However, it is also possible to choose titanium as a material. Another advantage is individualization regarding the angulation and design of the abutment to support the veneering ceramic.
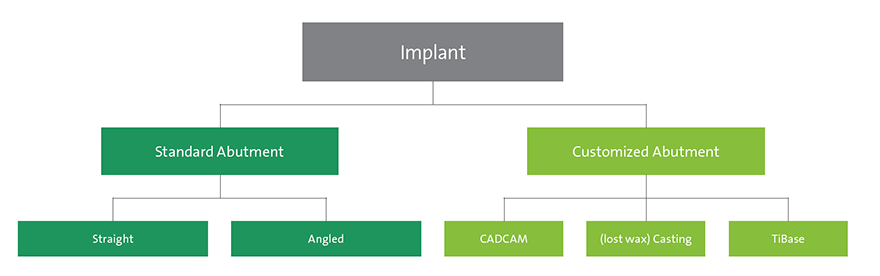
Fig. 2: Abutment decision tree
Traditional cast gold abutments can be used for screw- and cement-retained single crowns and bridges, and are available for implants placed at soft tissue or bone level. Their advantages consist in the facilitation of the screw retention with bridges. Disadvantages, however, are that gold abutments are technique-sensitive, require more time, and generate higher manufacturing costs. An in vivo histological study in dogs has demonstrated that gold alloys also have disadvantages in terms of soft tissue integration. Histologically, an apical shift of the barrier epithelium and the marginal bone around gold alloy abutments has been shown3. The third group of customized abutments on implants are the titanium base abutments. They are two-piece abutments with a titanium base. Clinicians are sometimes concerned about the handling of complications with a full ceramic abutment regarding the retrieval of broken-off ceramic fragments in the implant, which can be difficult. The main advantage of this abutment type is that there is no ceramic material inside the titanium implant connection. However, the disadvantage lies in the lack of evidence in published clinical data to date. In particular, the soft-tissue reaction regarding the bonding gap, especially in bone-level implant cases in the esthetic zone, remains unknown. In consequence, this type of abutment should be used with this current limitation in mind 4. However, use with soft tissue-level implants with a microgap above bone level might be less of a concern. An example of a soft tissue-level implant case is presented step-by-step on the following pages (Figs. 3-15).
2. Implant abutment material
Different biomaterials are available for implant abutments. PMMA (polymethyl methacrylate), titanium, and PEEK (polyether ether ketone) are indicated for abutments supporting provisionals – especially for bone-level-type implants – to customize the emergence profile and individualize the peri-implant mucosa with soft tissue conditioning5. The materials of choice for abutments for final restorations are titanium, gold, zirconium dioxide, and aluminum oxide-based ceramic. Titanium and zirconium dioxide will be discussed in this article regarding clinical and histological performance. Titanium is the biomaterial of choice regarding long-lasting and well documented behavior under functional loading for both soft and hard tissues. It has excellent biocompatibility, mechanical strength, and is resistant to corrosion. Therefore, it is the abutment material of choice for posterior sites. However, the expectations of patients in the anterior zone are increasing. In esthetic sites, mucosal thickness plays an important role. An animal study comparing different dental materials under different mucosal thicknesses showed that titanium induced the most prominent color change. Zirconium dioxide did not induce visible color changes in 2 and 3 mm thick mucosa.6 With the background of the available clinical evidence and systematic reviews, no differences were found between zirconium dioxide and metal abutments in clinical performance based upon esthetic, technical, or biological outcomes7,8,9,10. In vitro studies have shown statistically significant greater wear of zirconium dioxide than of titanium abutments inside the titanium implant11. However, the clinical relevance remains unclear. In our clinic, we have been using Straumann® CARES® CAD/CAM fabricated zirconium dioxide abutments since 2009 on a daily basis in esthetic cases with bone level implants, and have had no issues with abutment fractures so far. The correct CAD/CAM design of a zirconium dioxide abutment and the quality and precision of the connecting part into the implant play a crucial role in long-term success. Focusing on the outcome of histological studies, an in vivo study shows that there were no visible differences in soft tissue health in peri-implant mucosa adjacent to zirconium dioxide and titanium abutment surfaces12. Another study found that soft tissue around zirconium dioxide heals faster than when in contact with titanium13. A systematic review14evaluating the existing literature on zirconium dioxide abutments concludes based on evidence from animal and human histological studies that zirconium dioxide is as suitable a material for dental implant abutments as titanium. Regarding plaque accumulation, zirconium dioxide appears to have a lower tendency for surface-bound bacterial plaque in early stages, which is advantageous.
3. Conclusion and clinical recommendation
Abutment selection in esthetic sites: Implant abutments are located in a transition zone where they are in contact with the implant and the surrounding peri-implant tissues. Therefore, the choice of abutment is of major importance, especially in a sensitive region like the esthetic zone. For single-unit reconstructions, zirconium dioxide abutments are indicated, which can be either standard or customized depending on the prosthetic position of the implant. For multi-unit reconstructions, zirconium dioxide abutments are recommended for cement-retained bridges, and gold titanium abutments for screw retained bridges. Abutment selection in posterior sites: Clinical indication of each implant abutment type depends primarily on the prosthetic position of the implant and whether single or multiple units need to be replaced. Standard and Straumann® Variobase abutments are the abutment of choice in posterior sites if the prosthetic position of the implant is ideal. Angled standard abutments, individualized CAD/CAM abutments made of titanium, or cast abutments in gold are indicated in cases where the implant is not placed in an ideal prosthetic position. In multi-unit reconstructions, standard titanium or individualized gold abutments are recommended.
Clinical case report
Restoration of a single edentulous gap with an all-ceramic screw-retained implant crown in a posterior site using the Straumann® Variobase Abutment. This case was treated in a multidisciplinary approach: Prof. Dr. med. dent. Daniel Buser (Surgical), Dr. med. dent. Julia-Gabriela Wittneben, (Prosthetics), Thomas Furter, CDT (Lab).
Patient: non-smoking, healthy female, 43 years. Situation: a single edentulous tooth gap, region 46 (FDI). A Straumann® Soft Tissue Level Regular Neck Implant with Straumann® SLActive® surface was placed in a correct three-dimensional position (Fig. 3). Open-tray impression and bite registration followed eight weeks later. Peri-apical radiograph for evaluation of the impression coping position (Fig. 4). Fabrication and articulation of the master casts. Insertion of the scanbody. The cast was centralized in the scanning machine (Fig. 5). Bite registration with the scanbody in place (Fig. 6). Verification of digital image and manual modification, matching occlusion of the opposing dentition (Figs. 7, 8). A Straumann® Variobase Abutment was used (Fig. 9). An IPS e.max CAD crown made of lithium disilicate glass ceramic was ordered and delivered to the dental laboratory in a bluish color (Fig. 10). The crown was cut back with a diamond bur and crystallized in a furnace. Characterization and finalization of the crown followed by the manual addition of veneering ceramic (IPS e.max. Ceram) and the use of stain and glaze paste (IPS e.max Ceram Essences and FLUO). Different firing cycles. Cementation of the crown on the Straumann® Variobase Abutment with adhesive cement (Multilink Hybrid Abutment Cement). The excess cement was removed and polished (Figs. 11, 12). The final crown was tried intraorally and inserted with 35 Ncm inside the implant (Figs. 13, 14). Evaluation of the crown position (Fig. 15). The occlusion was adjusted and oral hygiene instructions given to the patient.
IPS e.max CAD, IPS e.max. Ceram, Essences and FLUO are registered trademarks of Ivoclar Vivadent, Schaan/ Liechtenstein.


