Treatment of two adjacent infrabony defects with Straumann® Emdogain®
A clinical case report by Martina Stefanini, Italy
In the following case, periodontal regenerative surgery with amelogenins (Emdogain®) produced complete filling of two adjacent vertical, deep and non-contained defects in the lower jaw. Moreover, the results were well maintained in the long term (6 years), as demonstrated clinically and radiologically. The periodontal regenerative treatment changed the prognosis of the lower first molar in a young patient, avoiding extraction and subsequent implant placement. The strict regimen of post-surgical control visits was critical for the successful long-term maintenance of the regenerative results.
Initial situation
A systemically healthy 33-year-old patient was diagnosed with localized aggressive periodontitis. A pre-operative x-ray (Fig.1) revealed an intra-bony defect in the distal aspect of tooth #46 and on the mesial aspect of tooth #45. Following the initial preparation, a residual 10 mm periodontal pocket was evident distal to tooth #46 and a 7 mm periodontal pocket mesial to tooth #45 (Figs. 2-3).
Treatment planning
After causal therapy, the patient showed a good standard of supragingival plaque control (FMPS and FMBS<15%), and regenerative periodontal surgery with Emdogain® was scheduled.
Surgical procedure
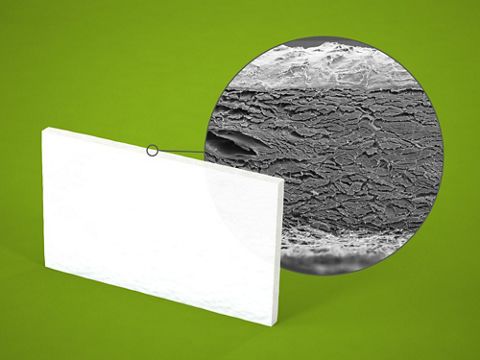
Following local anesthesia, an envelope-type flap extending from distal #43 to mesial #47 was raised. The supracrestal soft tissue above the angular defects was preserved with the amplified papilla preservation technique between #47 and #46 and with the simplified papilla preservation technique between #45 and #44 (Figs. 4-5). The flap was elevated in a split-full-split approach. The surgical papillae were elevated split thickness, while the central portion of the flap was elevated full thickness until the bony defects were completely exposed. The lingual flap, together with the interdental supracrestal soft tissues, was raised full thickness. The flap elevation was followed by debridement: both bony defects were degranulated, and the root surfaces were planed with ultrasonic and manual instruments. The infrabony defect on #46 was classified as a two-wall defect in the most coronal portion (missing vestibular wall), becoming a three-wall defect in the apical portion. The infrabony defect on #45 was classified as one-wall defect in the most coronal area while, in the apical area, a three-wall defect was evident (Figs. 6-7). The root surfaces were conditioned with EDTA gel 24% for two minutes to remove the smear layer produced by the root planing. After rinsing with saline solution, Emdogain® was applied on the exposed root surface and in the defects (Figs. 8-9).The anatomical papillae between #43 and #44 and between #45 and #4.6 were de-epithelialized, and the buccal flap was moved coronally in order to suture the surgical papilla to the connective tissue of the anatomical papilla with single interrupted sutures. The interdental soft tissues preserved in the area of the infrabony defects (#44-#45 and #46-#47) were sutured by first intention with single interrupted Vicryl 6-0 sutures (Figs. 10-11). The patient was instructed not to brush the treated area. Plaque control was performed with chlorhexidine solution 0.12% three times daily for 15 days. Systemic antibiotic therapy (amoxicillin 1 g twice daily for 7 days) together with anti-inflammatory therapy (ibuprofen 600 mg twice daily for 2 days and subsequently as needed) were prescribed. The sutures were removed after 15 days (Figs. 12-13).
Final results
The patient was recalled every month for the first 3 months, and then every 3 months for the first year. At each visit supragingival scaling was performed if needed, and oral hygiene instructions were reinforced. After 1 year, the x-ray showed completely filling of the defect with no clinical signs of inflammation (no BoP), and the residual probing pocket depth was 4 mm distal to #46 and 3 mm mesial to #45 (Figs. 14-16). The patient was recalled every 4 months for professional oral hygiene procedures, and after 6 years the successful result obtained with the regenerative surgery was well maintained: the x-ray showed complete filling of the defect and no clinical signs of inflammation, and no PPD greater than 4 mm were present. (Fig. 17-19)