Reducing invasiveness with a Straumann® Bone Level 3.3 mm narrow-diameter implant and botiss mucoderm®
A clinical case report by Andrea Pandolfi, Italy
In this case, the patient refused to have the bone volume increased by means of a block graft or GBR technique in a two-step approach. Therefore she was offered a less invasive protocol with a single surgical step and a minimally invasive flap, GBR and use of botiss mucoderm® for horizontal tissue augmentation.
Initial situation
The patient was a 72-year-old woman who wanted to replace a missing lower right posterior tooth in position #44 that had been extracted many years ago, with a dental implant. The general periodontal state of the patient could be described as moderately compromised. Reported comorbidities included gastritis, gastroesophageal reflux, with easy retching and bruxism, as was apparent by the wear on teeth facets shown in Figs. 2 and 3.
Treatment planning
Clinical examination revealed severe ridge resorption, accompanied by thin soft tissue in the position #44. Intraoral X-ray showed sufficient space between the roots for a 3.3 mm Straumann® BL implant (Fig. 1). However, the ridge was very thin and required horizontal augmentation in order to produce sufficient bone for implant placement (Figs. 2,3). Since she refused to have the bone volume increased by means of a block graft or GBR technique in a two-step approach, she was offered a less invasive protocol with a single surgical step and a minimally invasive flap, GBR and use of mucoderm® for horizontal tissue augmentation.
Surgery
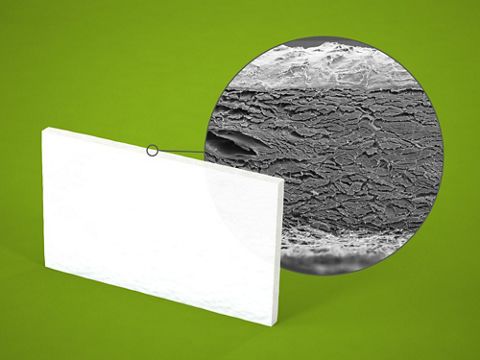
The entire surgical procedure was performed under local anesthesia. The paramarginal incision was made to obtain a minimal full thickness mucoperiosteal flap. The drilling was performed with piezosurgery tips combined with a calibrated drill for the insertion of a Straumann® BL ⌀ 3.3mm SLActive® implant according to the manufactures instructions. The traditional non-guided template was used. The surgical site was prepared at a low speed so that autologous bone debris could be collected for the recovered autologous bone technique. The mucoperiosteum was reflected, and the Straumann® BL implant (Roxolid®, SLActive® 3.3mm/14mm) was placed in the 44 site (Figs. 4 — 8). botiss cerabone® mixed with the patient’s autologous bone was used for augmentation of the vestibular bone wall. (Figs. 9,10). The horizontal augmentation of the soft tissue was performed with mucoderm® (Figs. 11,12). Afterwards, a healing cap was fitted, and the site was properly sutured with non-absorbable monofilament suture (Fig. 13). Healing was uneventful, and sutures were removed at one week post-surgery (Figs. 14,15).
Prosthetics
After two months of soft and hard tissue healing (Figs. 16,17), the soft tissue around the implant abutment was healthy, and the buccal contour was maintained (Figs. 18,19). Next, an impression (conventional approach using soft impression material) was taken, and a personalized crown consisting of veneered monocrystalline zirconia on the Straumann® Variobase® abutment was designed using abutment designer software (Figs. 20,21), fabricated and cemented (Figs. 22 — 26).
Final results
After one year (Fig. 27) and two years (Figs. 28 — 31) of follow-up, the clinical situation was stable. No biological or technical complications were reported. Clinical assessment showed a stable position and volumes of both hard and soft tissues. The outcome was a complete reconstruction of the horizontal defect of the tissue. The entire therapy was well planned, the surgical interventions and prosthetic procedures were carefully performed. The final prosthetic result was very satisfactory. The patient was very pleased to have achieved the result with only one-step surgery according to a less invasive protocol.