Successful immediate implant placement associated with immediate loading remains one of the biggest clinical challenges. In addition to the placement of an implant into a tooth socket concurrently with extraction, the creation of a screw-retained CAD/CAM provisional prosthetic restoration is critical for the esthetic outcome. Currently, the procedure can be achieved using a conventional approach resulting in a high number of patient appointments with time-consuming steps for the dentist. For the patient, the day of the immediate loading treatment remains a long and tiring experience from the surgery to the provisional restoration. Instead of exposing the patient to a “marathon” day, the treatment could be shortened considerably by fully involving the patient, the surgeon and the dental technician and by having a predictable treatment protocol for the tooth extraction and the prosthetic restoration design (including the individual emergence profiles prior to the surgery). This would also lead to a better patient experience and improved satisfaction. The goal of this clinical report is therefore to introduce an innovative one-step surgical approach for immediate screw-retained CAD/CAM provisionalization by using the latest technological improvements in prosthetic and surgical planning software and seamlessly integrating the dental technician into the development of the fully digital treatment planning and new prosthetics options.
Initial situation
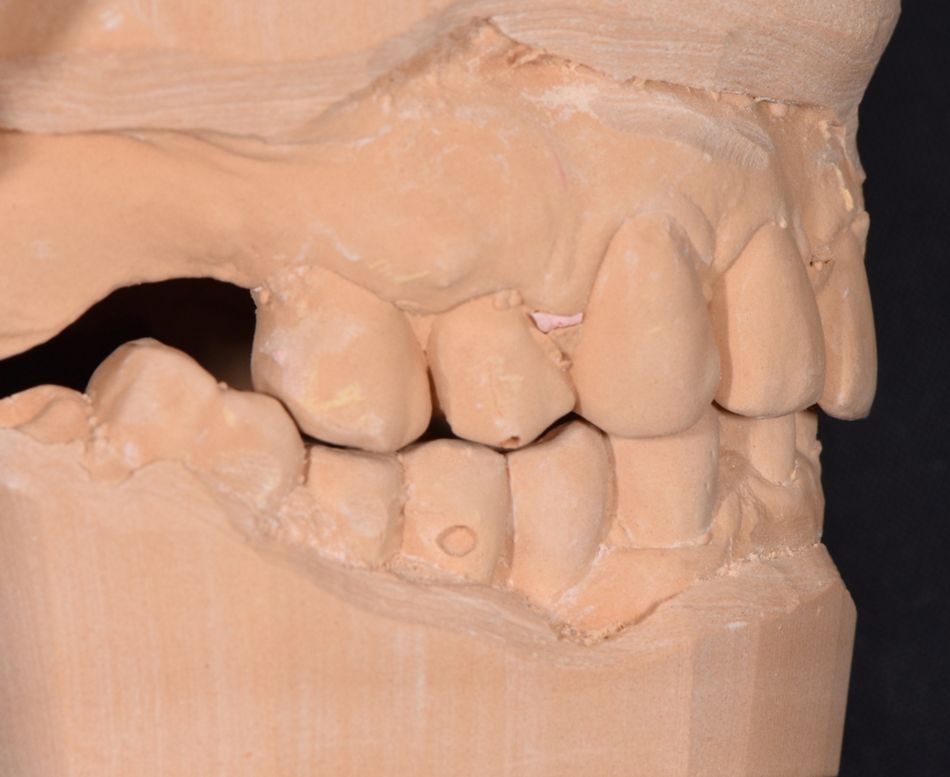
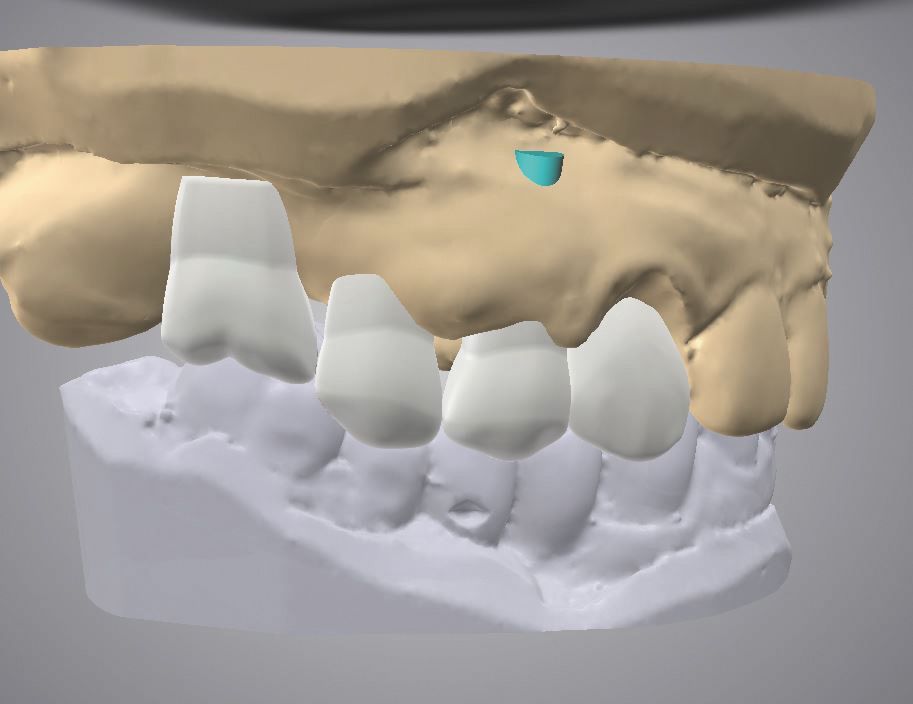
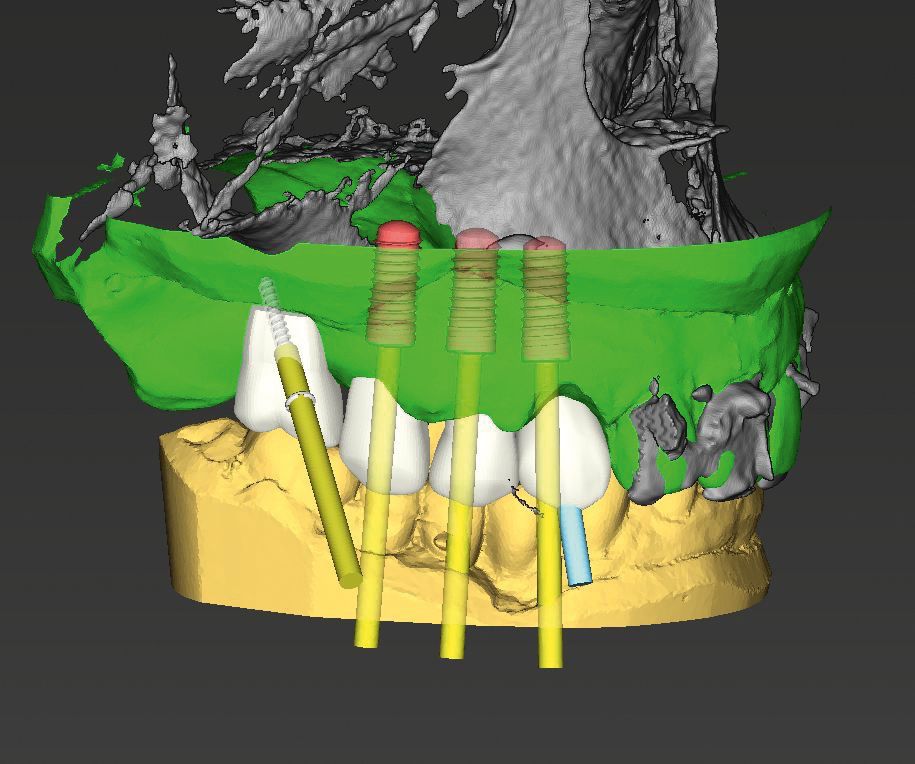
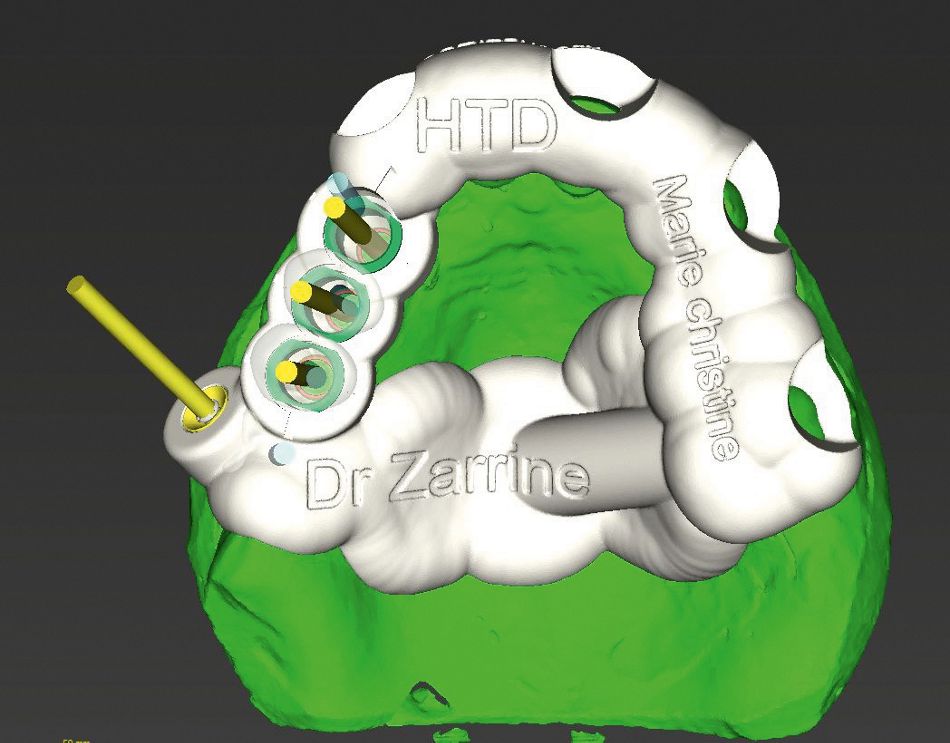
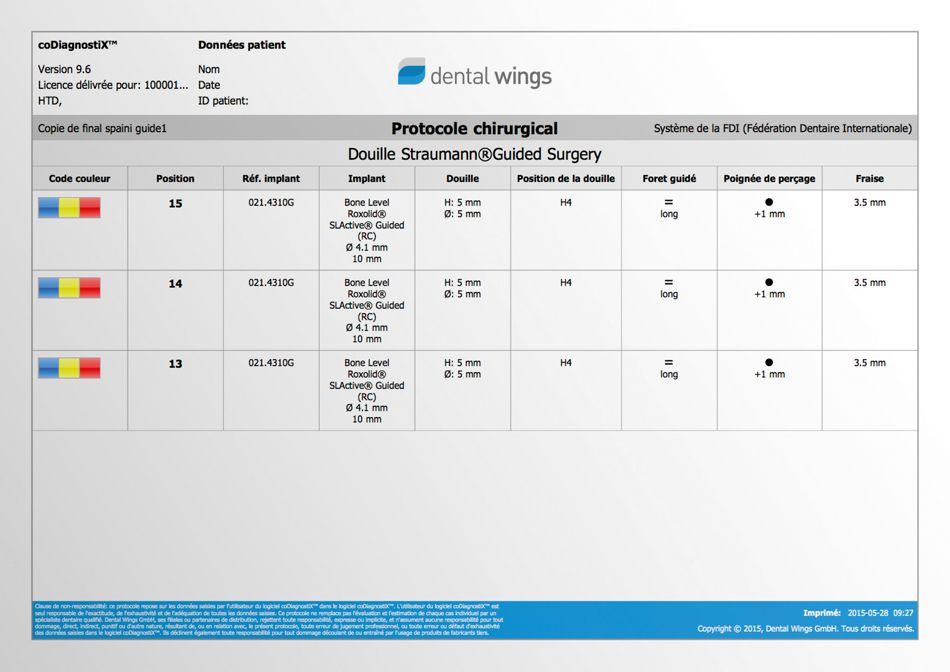
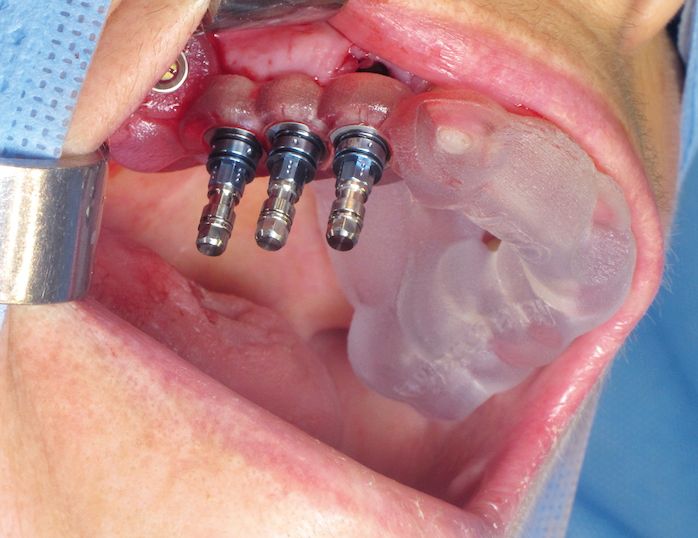
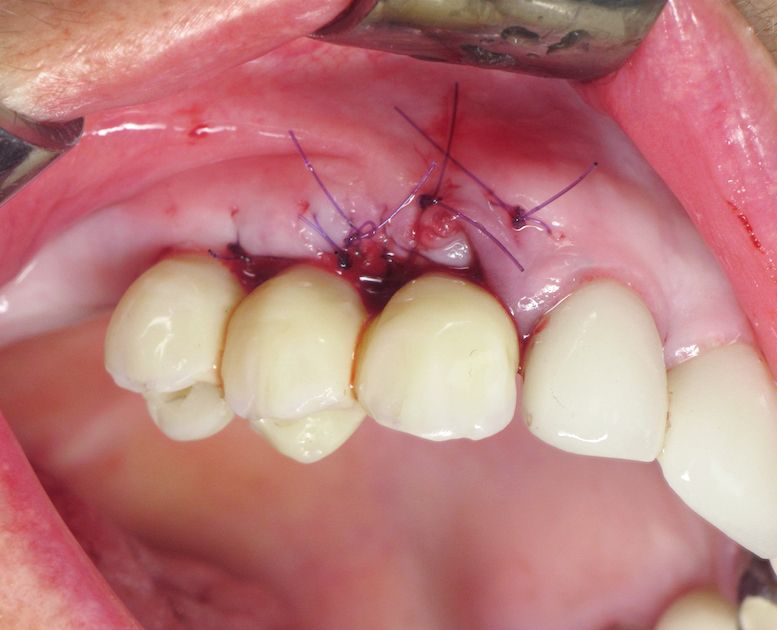
The patient was 65 years old, female, non-smoking, with a fragile health condition, and willing to get back an adequate chewing capability. The patient suffered from cachexia following a stomach ablation resulting in an obvious compromised digestion which is an aggravating factor in the dental condition (Fig. 1). The molars in sector 3 were missing, tooth 26 had to be restored and the occlusion curves adjusted. Teeth 13, 14 and 15 had a mobility classification of 3 according to Lindhe and Muehlmann. The roots were decayed and fractured, with the gum suffering from inflammation in 14 and 15 without abscess and sinusitis. Tooth 47 underwent an eruption, and bridge from 47 to 43 seems to follow this new curve of occlusion. This situation does not allow for sufficient inter-arch height in order to have number 16 as antagonist. To prevent an over-infection as well as for esthetic and comfort-related reasons, the urgency consisted in the treatment of sector 1. The overall health condition and drug treatment reinforced our decision to use a non-invasive surgical approach. The treatment plan was as follows: #47 and #43: recreating sector 4 with two individual implant-borne restorations (Straumann® Soft Tissue Level Implant RN, Roxolid® material, SLActive® surface) respecting the occlusion curves. #26: root treatment with a tooth-borne restoration in the occlusal plane. #35# 36, placing of two individual implant-borne restorations (Straumann® Soft Tissue Level Implant WN, Roxolid® material, SLActive® surface). From #13 to #16: implant-borne restoration after tooth extraction of 13, 14 and 15 (Straumann® Bone Level Implant RC, Roxolid® material, SLActive® surface) The patient will have a reduced arcade. However, the occlusion will be balanced and provide a good masticatory coefficient. The current situation forced us to compromise (Fig. 2) and to place three implants in place of three teeth: canine, premolar and molar. The aim was to extract atraumatically the three decayed teeth and to perform an immediate implant placement after extraction with flapless surgery in conjunction with immediate loading enabling restoration of the other sectors. In order to maximize accuracy and to reduce the number of steps, a fully digital approach using guided surgery was selected, allowing us to preoperatively produce a screw-retained CAD/CAM provisional restoration.