Introduction
Clinical usage of ceramic dental implants is a reliable treatment alternative to titanium implants, supported by increased scientific evidence. Ceramic dental implants meet the growing desire for metal-free treatments and a natural, highly esthetic look, and address the needs of patients with metal hypersensitivities.
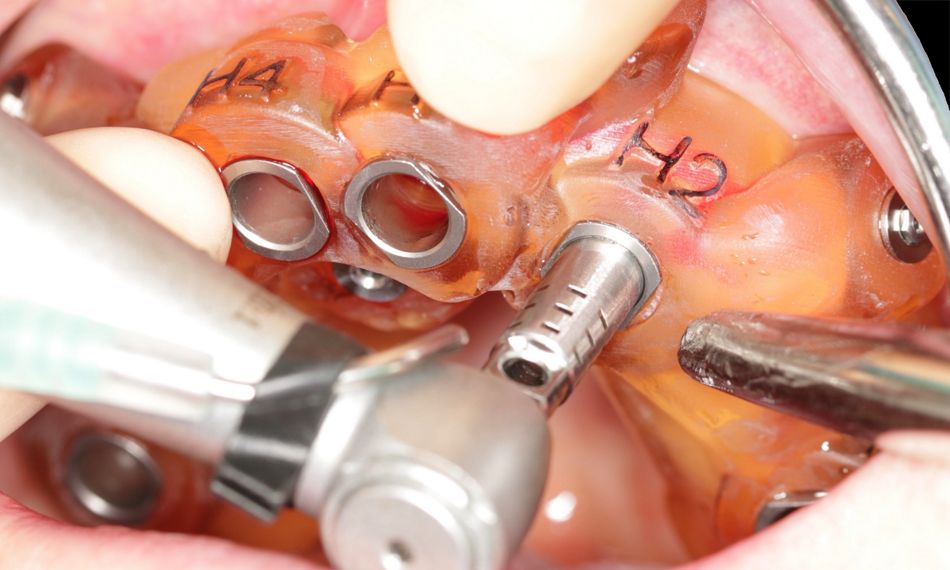
The Straumann® PURE Ceramic Monotype Implant consists of an implant and abutment made from zirconium dioxide ceramic. It is based on features of the Straumann® Soft Tissue Level Standard Plus and Straumann® Bone Level Implants. Therefore, they are very straightforward to implement in our practice, as the surgical cassette used is the same as that for the Straumann® Bone Level Implants.
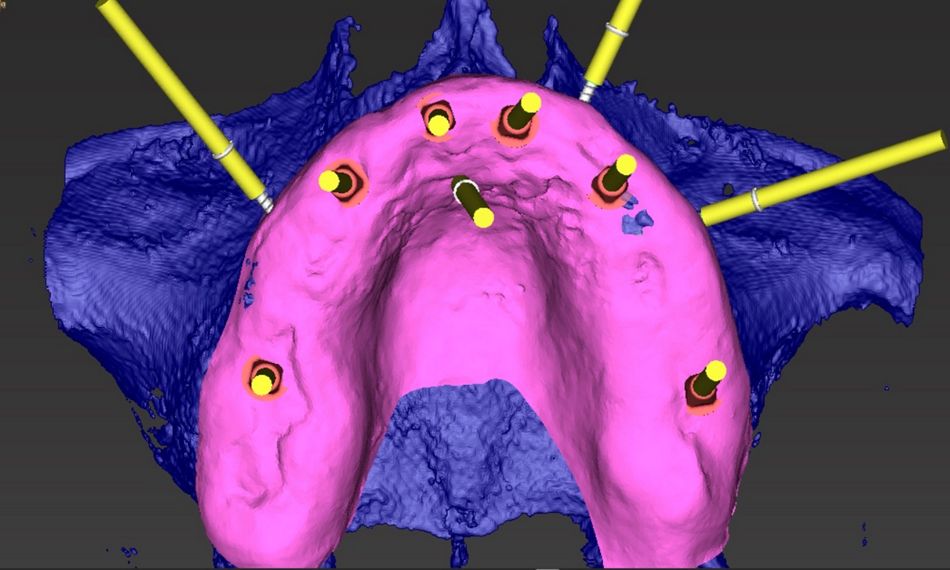
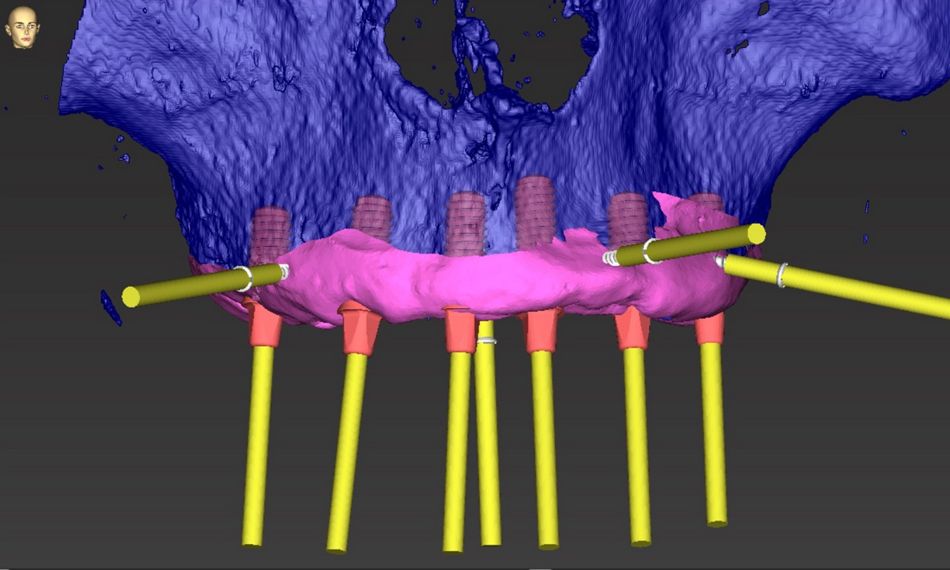
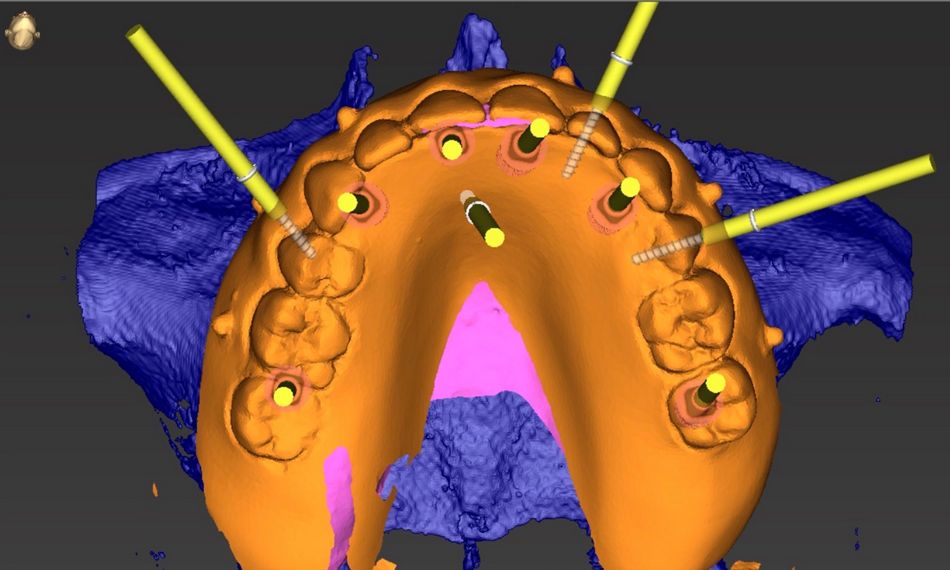
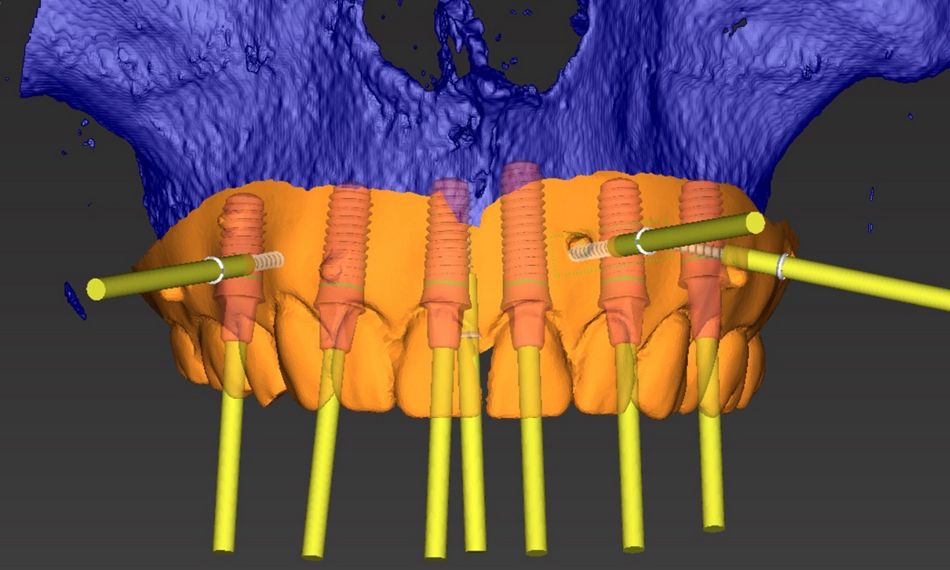
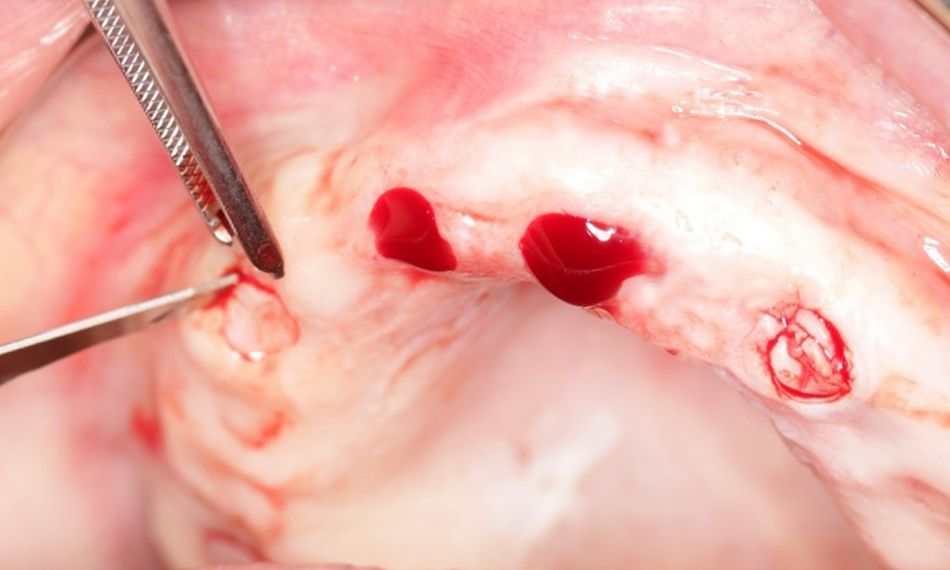
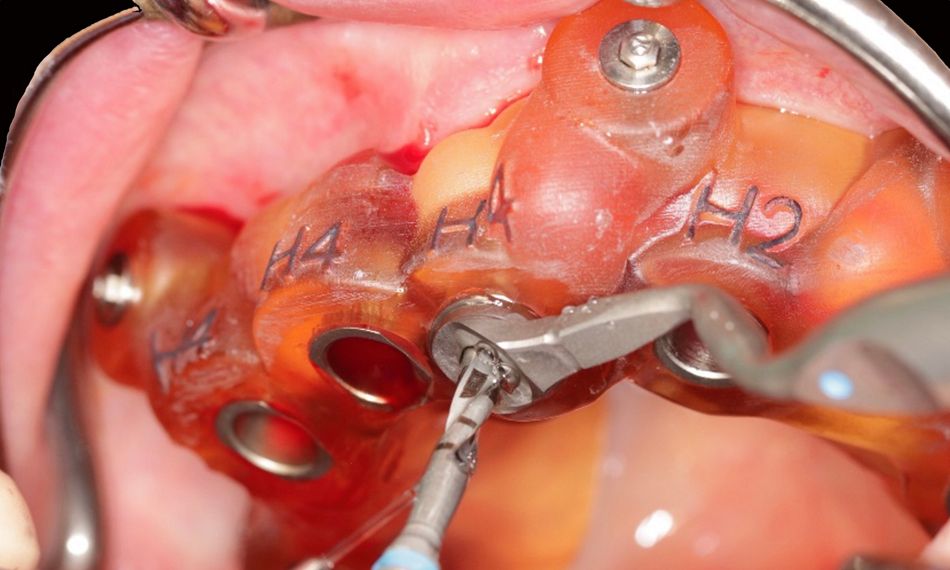
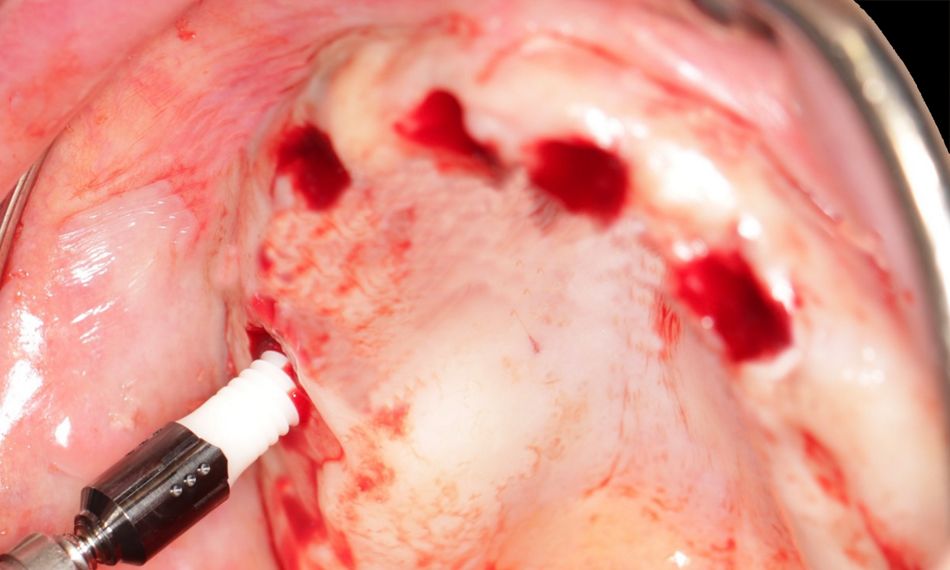
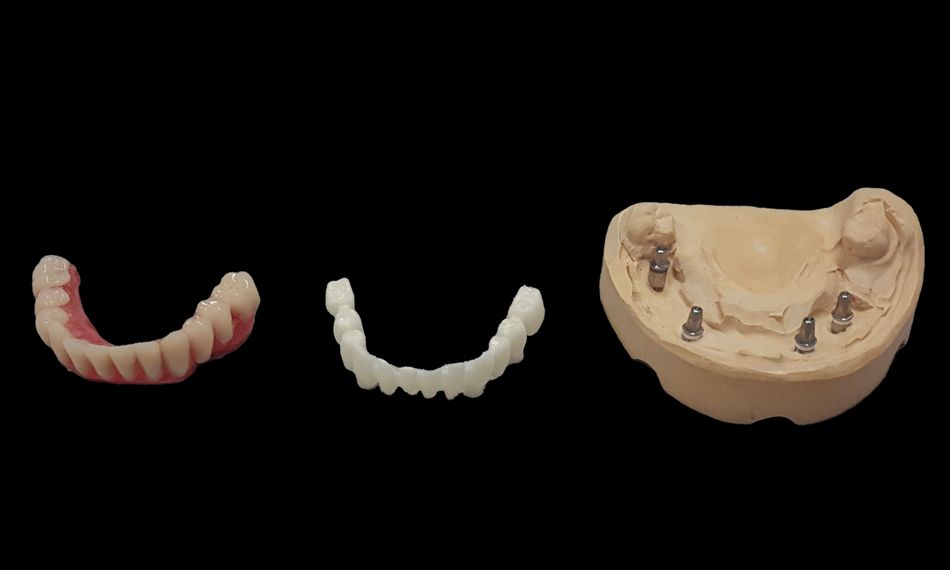
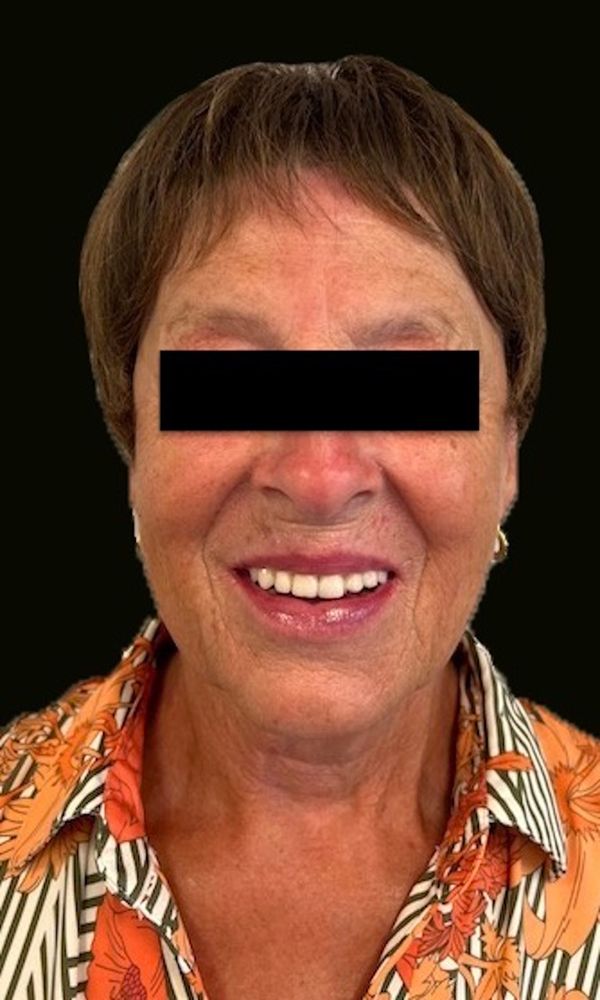
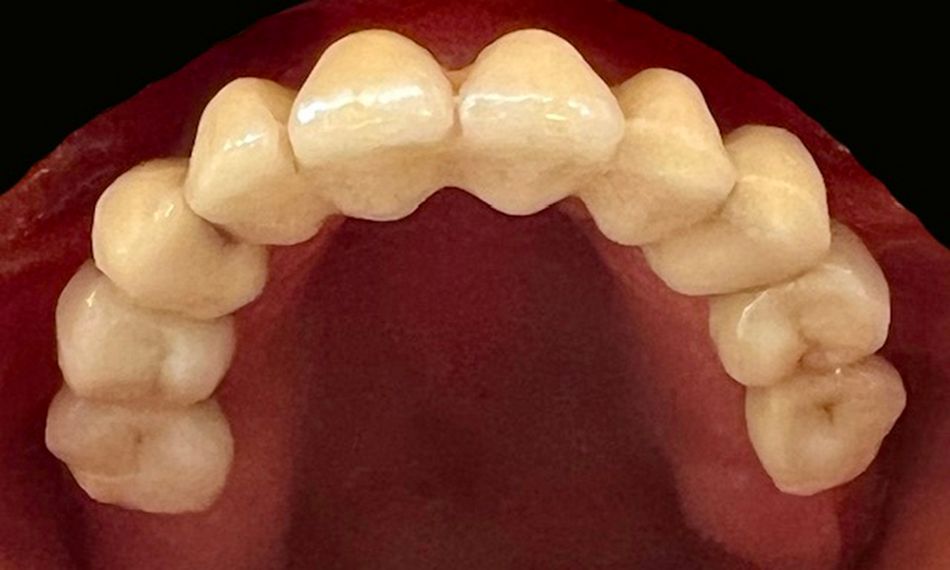
The following clinical case shows a successful bimaxillary full-arch rehabilitation with zirconium bridges in the lower and upper jaws supported, respectively, by four and six Straumann® PURE Ceramic Implants Monotype in a patient who requested a metal-free solution for her unstable prostheses. The patient later received chemotherapy for a tonsil carcinoma. Even 5 years after completing the implant treatment, the patient remained satisfied with the outcome and did not report any mechanical or biological complications during the follow-up visits.
Initial situation
A 70-year-old female patient presented herself to our clinic in 2014. Her main complaints concerned unstable lower and upper restorations that did not allow her to chew or speak properly; moreover, she explained that these issues also affected her general quality of life and self-confidence. Her medical history revealed alopecia due to an underlying autoimmune disorder. In addition, she reported poly-allergic features to nickel and emphasized her desire to keep a fixed bridge with a metal-free solution for her peace of mind.
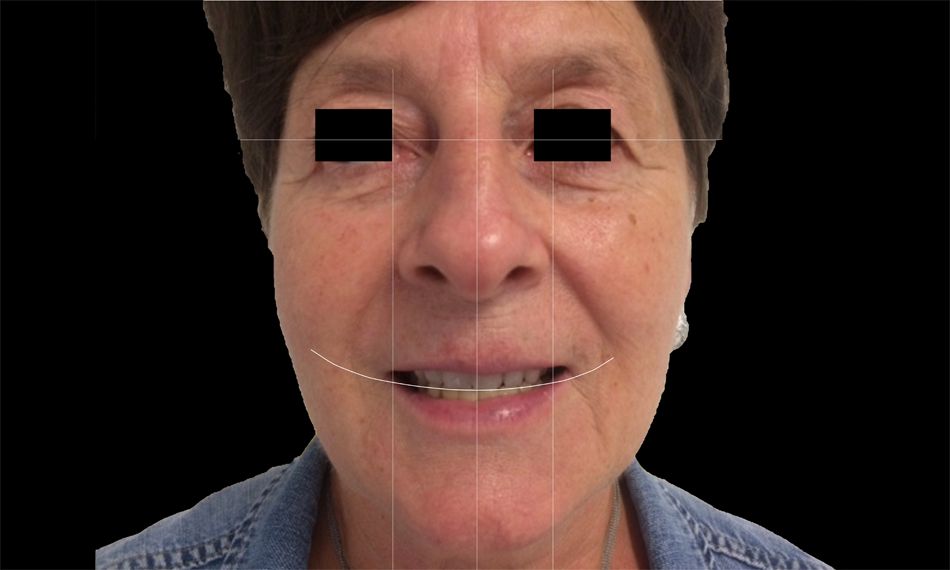
The extraoral examination showed mild face asymmetry and an average smile line (Figs. 1-3).
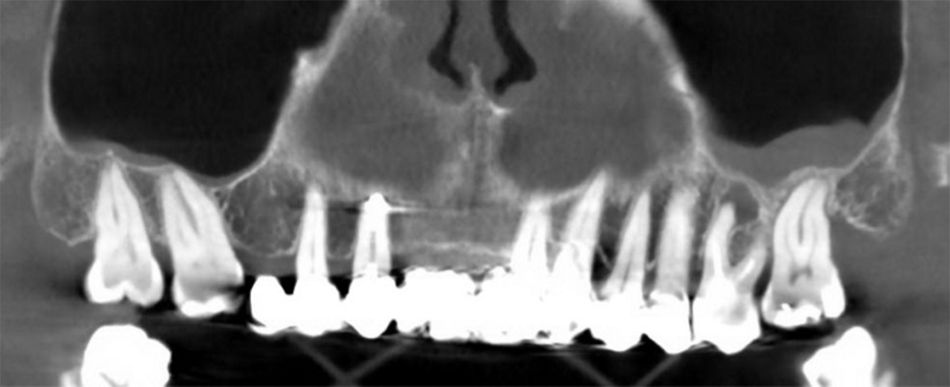
The intraoral examination showed an edge-to-edge bite with upper midline deviation. The patient was periodontally compromised on the remaining teeth, with the presence of deep periodontal pockets, inflammation, dental mobility, and bleeding on probing on all sites, except on teeth #37 and #47.