Early developments
Zygomatic implants were first introduced by Per-Ingvar Brånemark in 1998 for maxillectomy patients and later adapted for edentulous patients with severely atrophied maxillae1.
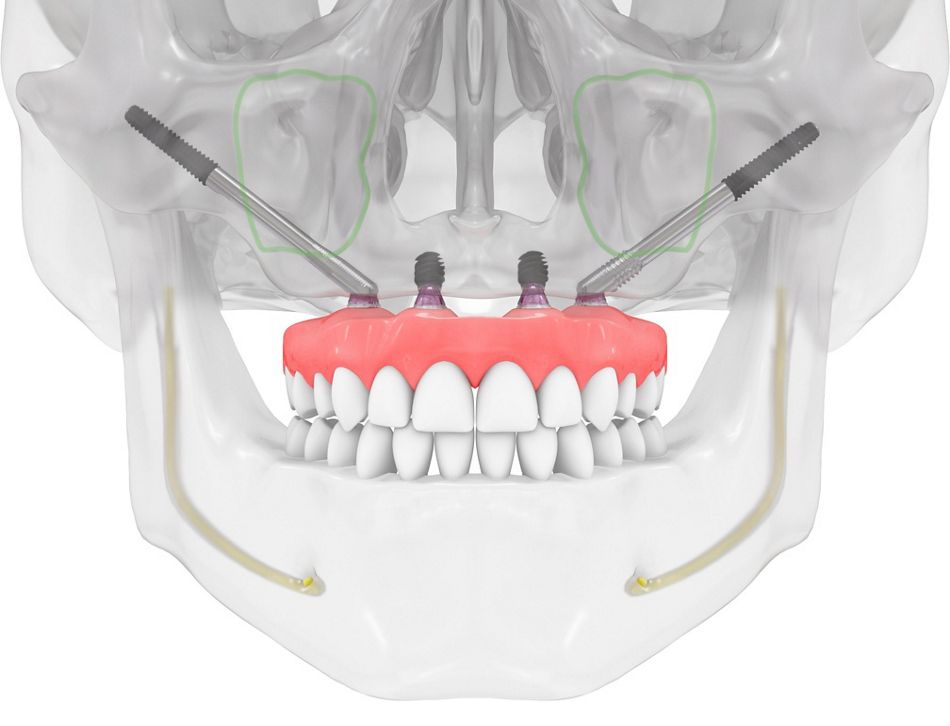
Placement methodologies evolved to the concept of 2 posterior zygomatic implants (one in each quadrant) and the "quad zygoma" approach with four zygomatic implants (two for each quadrant)t, allowing loading within 24 hours. Early studies by Brånemark et al. showed a 96% rehabilitation rate with 52 implants in 28 patients over at least 5 years. However, despite success, complications like rhinosinusitis and soft-tissue infections were common2. To reduce invasiveness, Stella and Warner proposed the “slot technique” in 2000, using a crestal entry to eradicate the problem of bulky prostheses3. In 2006, Migliorança et al. reported outcomes of 150 externally positioned zygomatic implants in 75 patients, reducing rhinosinusitis risk4. Aparicio’s group later proposed an exteriorized implant pathway to avoid sinus perforation5, though buccal soft tissue recession was observed6. In an extension of other studies, Malo et al. introduced a modified extra-maxillary technique, requiring alveolar ridge contouring, which sometimes caused sinus infections7. This led Aparicio to introduce and describe the anatomically guided ZAGA approach in 2011 following his long-term experiences with similar complications while placing zygomatic implants in patients with severe atrophy8.
Patient’s anatomy first, the ZAGAclassification
The zygomatic anatomically guided approach (ZAGA) is an evolution of the above methods devised to provide patients with long-term, complication-free, predictable implant solutions, whatever their anatomical situation8. The rationale is that patients present with differing anatomical variations, and even site variations, within the same patient. Hence, the need to have an adaptable solution rather than a one-size-fits-all protocol is paramount. Treatments can be intra-, extrasinus, or a combination of both. Aparicio developed an anatomical evaluation process known as ZAGA classification to aid the right treatment protocols in any given situation. Initially, in a cross-sectional survey9 based on 200 sites across 100 patients, he identified and classified five anatomical pathway situations as ZAGA 0-4. Classifications range from ZAGA 0 (straight lateral maxillary wall with the implant platform on the crest and the middle portion inside the sinus) to ZAGA 4 (extreme resorption of the maxillary sinus with or without significant concavity of the lateral sinus wall). This allowed for a better understanding of the shape of the maxillary wall and how it would predetermine the implant pathway9.
Such classification aims to provide the right prosthetically driven implant pathway to prevent long-term complications. The implant path is studied to achieve this aim, and three key areas are defined: the anchor zone, the antrostomy zone, and the zygomatic implant critical zone (ZICZ). As a result, everything from the initial incision and the implant path to the closing of the soft tissue is individually tailored, depending upon the classification of the patient. The classifications were identified as ZAGA 0-4 and would later be branded with an “A” or a “P” to determine anterior or posterior atrophy.
Therefore, the anatomically guided approach is more than just a treatment protocol; it’s a philosophy where everything, including the tools and technologies, is adapted to the patient’s anatomy. One such adaptation is the redesign of the zygomatic implant itself.
ZAGA Flat and ZAGA Round zygomatic implants
Because a typical zygomatic implant pathway involves the atrophic alveolar bone, the maxillary wall, and the zygoma bone, such a clinical picture may present greater difficulties in treatment planning and implementation than a conventional implant route. To overcome those obstacles and facilitate the treatment, 2 different topographies of zygomatic implants (ZAGA Flat and ZAGA Round) were proposed, designed, and developed. Both aim to improve treatment outcomes by matching the patient's anatomy, ensuring a maximum anchorage in available bone.
In clinical cases, with the presence of sufficient bone around the implant platform allowing for better occlusal force distribution, Straumann® Zygomatic Implant ZAGA Round is recommended. The bone around the implant platform will enhance occlusal force distribution and connective soft-tissue attachment, which is crucial for the stability of the facial gingival margin. On the other hand, in cases of extreme maxillary resorption and sinus wall concavity (ZAGA 4) or total/partial maxillectomy, the implant needs to be positioned below the vestibular soft tissue, making vestibular dehiscence difficult to prevent. To reduce this risk, the Straumann® Zygomatic Implant ZAGA Flat is the ideal choice. Its flattened shaft allows deeper submersion in the bone crest, and partial coronal threads maximize bone-to-implant contact and seal the bone wound. This design minimizes soft-tissue irritation and exposure, ensuring high anchoring despite severe atrophy and promoting a favorable long-term soft-tissue response.
Clinical performance of Straumann® Zygomatic implants
The body of evidence regarding the clinical performance of ZAGA Flat and ZAGA Round implants is continuously growing and demonstrating they can be considered a viable treatment option for patients with severely atrophied maxilla. When used in conjunction with the corresponding channel and tunnel osteotomies, research shows that after an average follow-up of 18.8 months utilizing the Offset, Rhinosinusitis, Infection, and Stability (ORIS) criteria, rehabilitation with ZAGA flat and ZAGA round implants resulted in no surgical complications, making them a viable treatment option when restoring atrophic maxillae10. Moreover, a recent non-interventional study by Aparicio et al. highlights the clinical effectiveness of ZAGA Round and Flat zygomatic implants in patients with severely atrophied maxillae. In this study, the patients receiving 2, 3, or 4 ZAGA implants were followed for up to 53 months, with an average follow-up of 46.5 months. This effectiveness of the treatment approach is reflected in a 100% survival rate for both implants and prostheses, along with minimal changes in the frequency of late complications compared to earlier one-year follow-up11.
The ITI gets into the game
Finally, in 2023, a meeting of 25 ITI experts in the field of zygomatic implants took place in Frankfurt, Germany, to provide consensus statements and standardized clinical recommendations for using zygomatic implants12. Three systematic reviews13–15 and one narrative review16 were compiled to address focus questions based on indications, post-surgical complications, long-term survival rates, and biomechanical principles under immediate loading. As the outcome, 21 consensus statements were substantiated, focusing on indications, quad zygoma, loading protocols, surgical risks, biological and technical complications, and PROMs. Additionally, 17 clinical recommendations were formulated around planning, case selection, diagnostics, surgical aspects, complications, restorations, and outcomes, including clinical advantages and survival rates. The meeting also highlighted recommended areas for future research, namely the development of standardized reporting data, further evaluation of implant geometry, and more randomized controlled trials for better management of sinusitis and oroantral communications. The experts also recommended continuing longer-term and multi-center case studies on zygomatic implants in patients with complete maxillary loss and congenital and resection-related defects. Establishing standardized clinical recommendations and consensus statements by leading experts provides a strong foundation for these procedures' continued success and refinement. This means that patients with little quality of life before may now experience full dental rehabilitation using proven or trusted techniques and protocols that surgeons can follow.
Conclusions
In conclusion, zygomatic implants offer a viable treatment option for patients with severely atrophic maxillae. They have demonstrated high short- and long-term survival rates, making them a reliable solution and preferred choice for complex cases where extensive GBR could be avoided. Consequently, patients report high satisfaction levels due to significant improvements in chewing functionality and esthetics17–21. The future of zygomatic implants looks bright, with a commitment to innovation driving the field forward. With ongoing research and the development of new techniques, zygomatic implants will continue to evolve, providing reliable and tailored treatment options, improving patients' quality of life, and equipping dental professionals with the tools and knowledge to deliver optimal care.
