What is this about
This article outlines a clinical case demonstrating full-arch rehabilitation using Straumann’s Pro Arch™ concept with BLX implants.
- Presents the treatment sequence and main considerations for immediate full-arch restoration.
- Highlights the advantages of the BLX implant design within the Pro Arch workflow.
- Emphasizes digital planning using Smilecloud, coDiagnostiX®, and Straumann® RevEX™ to achieve precise implant positioning, predictable prosthetic design, and fewer clinical visits.
Introduction
Full-arch rehabilitation is a complex procedure that requires careful planning and precise execution to achieve optimal function, esthetics, and long-term stability. Recent advances in digital dentistry, including intraoral scanning, guided surgery, and CAD/CAM technology, have improved the predictability of these treatments. Tools such as Smilecloud, coDiagnostiX®, and Straumann® RevEX™ facilitate accurate implant placement, efficient prosthetic design, and fewer clinical visits. In this case, the patient was treated with Straumann’s Pro Arch concept using BLX implants. In the maxilla, treatment involved guided placement of four implants combined with crown lengthening and bone removal, while the mandible received a full-arch rehabilitation. This report details the clinical workflow, highlighting how digital planning and precise execution contributed to predictable functional and esthetic outcomes.
Initial situation
A 65-year-old female patient presented with significant difficulty in eating and speaking. She reported that these functional limitations had a considerable impact on her quality of life, affecting both her social interactions and self-esteem. The patient expressed dissatisfaction with the appearance of her smile and reported avoiding smiling in public due to a lack of confidence (Fig. 1).
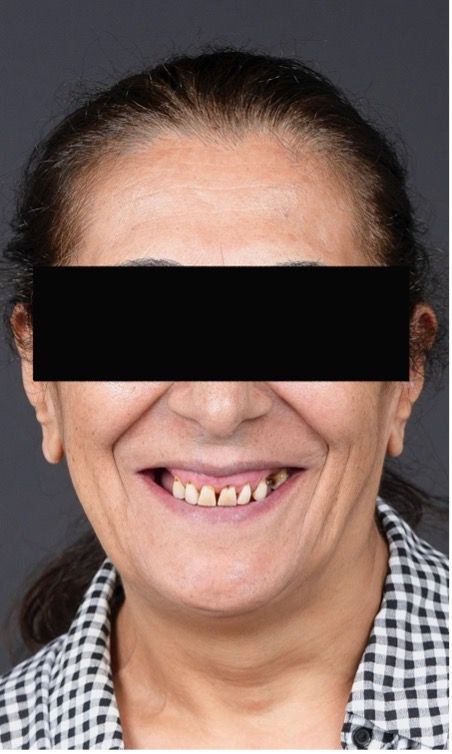
Her main expectations were to correct the gummy smile, replace missing teeth, and restore both function and aesthetics. The patient reported no history of systemic diseases, smoking habits, or regular medication use.
The patient had lost all mandibular teeth several years ago and reported discomfort from ill-fitting dentures that moved during eating. She had also undergone several extractions in the maxilla, resulting in partial edentulism in the upper arch.
Clinically, she exhibited an edentulous mandible with atrophy and a partially edentulous maxilla (Fig. 2). Radiographic and cone-beam computed tomography (CBCT) evaluation revealed insufficient vertical bone height in the posterior mandible and poor bone quality in both the mandible and posterior maxilla (Fig. 3). The remaining maxillary teeth showed a good prognosis, though some presented carious lesions.
The case was classified as complex according to the ITI SAC classification for both surgical and prosthodontic considerations.
Treatment planning
Step 1: Initial evaluation, dental scans, diagnosis and preoperative planning using Smilecloud (Fig. 4). A mock up was also made (Fig. 5).
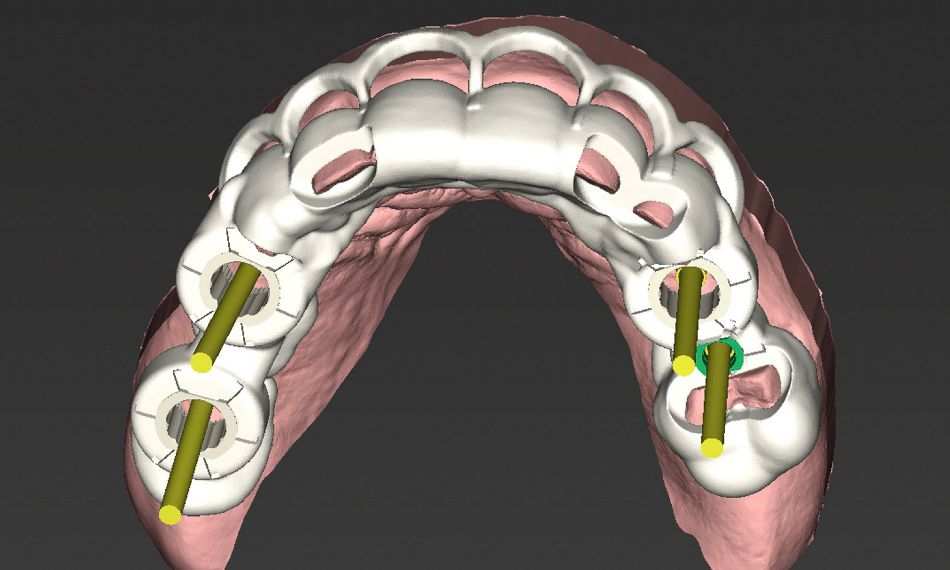
Step 2: Virtual implant positioning and surgical guide design were performed using the coDiagnostiX® implant planning software, including guide design for four upper implants and crown lengthening with bone removal (Fig.6). Due to insufficient space for two regular guide sleeves in the left posterior maxilla, we used a 2,8 mm sleeve for site #25 and regular 5 mm sleeves for the remaining implant sites.
Step 3: Straumann® Roxolid® SLActive® implants were placed in the upper jaw at the following positions: #14: Straumann® BLX, Ø4.0 mm, length 12 mm, #16: Straumann® BLX, Ø4.0 mm, length 8 mm, #24: Straumann® BLX, Ø3.75 mm, length 10 mm, #25: Straumann® BLX, Ø3.75 mm, length 10 mm and Crown Lengthening was performed.
Step 4: In the lower jaw, implants were placed using a freehand technique: two tilted and two axial implants.
Step 5: Provisionalization was carried out, with early loading applied to the four maxillary implants and immediate loading to the four mandibular implants.
Step 6: Straumann® RevEX™ workflow.
Step 7: Definitive screw-retained rehabilitations.
Author’s testimonial
Guided crown lengthening with bone removal and guided implant surgery was performed, placing 8 implants with precision and expertise. This complex case required meticulous planning and execution to address both surgical and prosthodontic challenges. Utilizing Straumann's advanced digital tools such as Smilecloud, coDiagnostiX® and Straumann® RevEX™ integrated into our fully digital workflow to optimize treatment planning and execution, ensuring optimal outcome for our patient. The treatment successfully restored the patient's oral function, stability, and aesthetics, significantly improving overall quality of life.
Surgical procedure
Prophylactic antibiotics were prescribed prior to surgery. Local anesthesia was administered to both the maxilla and mandible. Regular crestal incisions were performed to access the alveolar ridge. The guided surgical guides were then positioned, and their fit and stability were verified (Fig. 7).
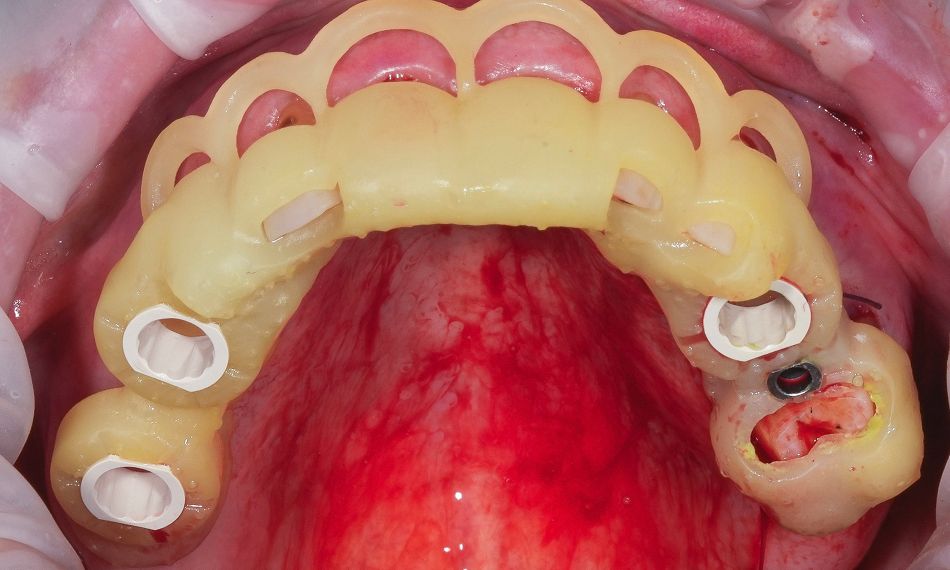
Once proper seating of the guides was confirmed, guided osteotomies were performed according to the preoperative virtual plan, using sequential drilling under copious irrigation to minimize trauma. The accuracy of guide positioning enabled precise execution of the crown lengthening procedure with controlled bone removal, ensuring ideal prosthetic space and emergence profiles. Furthermore, the implants were placed at the following sites: #14 – Straumann® BLX Ø4.0 mm, length 12 mm; #16 - Straumann® BLX Ø4.0 mm, length 8 mm; #24 – Straumann® BLX Ø3.75 mm, length 10 mm; #25 – Straumann® BLX Ø3.75 mm, length 10 mm; (Figs. 8 - 9).
Optimal contour and soft tissue adaptation were achieved, and the surgical sites were thoroughly irrigated with sterile saline to remove any bone debris. The flaps were repositioned and carefully sutured to ensure a tension-free primary closure (Fig. 10).

In the lower jaw, all implants were placed in healed sites, as the patient had undergone extractions several years earlier (late implant placement). The lower jaw presented an atrophic edentulous mandible (Fig. 11).
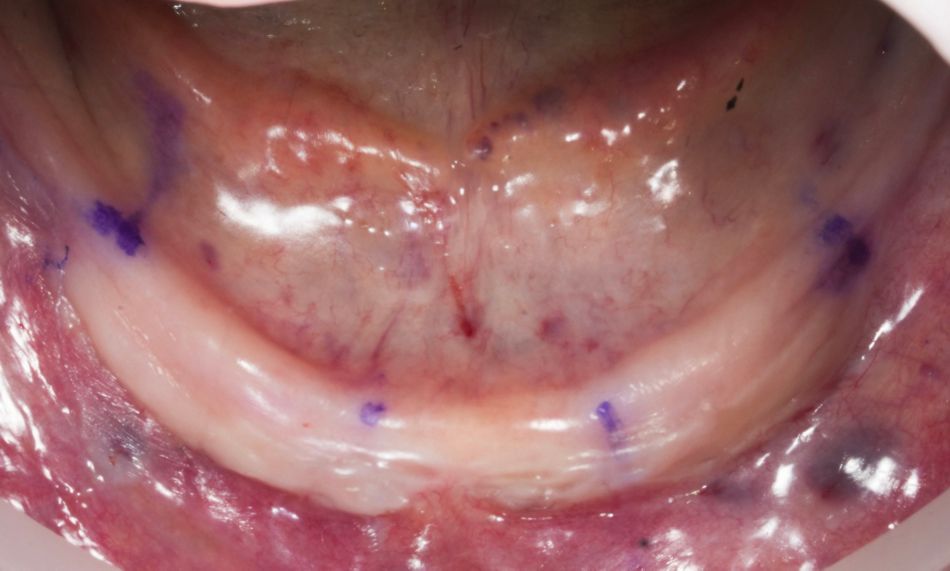
In this region, two tilted and two axial implants were placed freehand. Straumann® Roxolid® SLActive® implants were inserted according to the surgical plan to achieve optimal primary stability. The following implants were placed: #32 – Straumann® BLX Ø3.75 mm, length 10 mm; #35 – Straumann® BLX Ø3.75 mm, length 12 mm; #42 – Straumann® BLX Ø3.75 mm, length 10 mm; and #45 – Straumann® BLX Ø3.75 mm, length 12 mm (Fig. 12).

Implants were placed with a torque of 35 Ncm, which suggests that adequate primary stability was achieved (Fig. 13). The postoperative view showed correct alignment and integration after implant placement, with proper soft tissue adaptation and satisfactory implant positioning in relation to the planned prosthetic restoration (Fig. 14).
No bone augmentation procedures were required, and soft tissue management was performed to achieve a tension-free closure. Postoperative medications and standard postoperative instructions were provided. Follow-up evaluations confirmed uneventful wound healing.

A Center of Dental Education (CoDE) is part of a group of independent dental centers all over the world that offer excellence in oral healthcare by providing the most advanced treatment procedures based on the best available literature and the latest technology. CoDEs are where science meets practice in a real-world clinical environment.
Prosthetic procedure
Early loading was applied to the four maxillary implants, while immediate loading was performed for the four mandibular implants. The provisional restoration was delivered the day after surgery using screw-retained abutments (SRA), torqued to 35 Ncm, and a screw-retained prosthesis that was picked up intraorally. The interim restoration was fabricated from CAD/CAM-milled PMMA, ensuring optimal fit, esthetics, and hygiene during the osseointegration period.
Three months after surgery, successful osseointegration was confirmed. A passive fit of the temporary restoration was achieved.
At the first appointment, a functional mock-up was fabricated to evaluate occlusion, esthetics, vertical dimension, and phonetics before proceeding with the definitive restoration (Fig. 15). The extraoral reverse scanning technique was used to digitally capture implant positions for prototype prosthesis fabrication. Three digital scans were acquired with an intraoral scanner (TRIOS 5, 3Shape). The first scan recorded the conversion prostheses in situ, capturing occlusal, palatal/lingual, and buccal surfaces, as well as the patient's occlusion. The second captured the soft tissue morphology of the arches with screw-retained abutments after prosthesis removal; and the third was an extraoral reverse scan of the prostheses with Straumann® RevEX™ scan bodies to accurately record the 3D implant positions and facilitate the design of the definitive prosthesis (Fig. 16).
The three scan sets were imported into CAD software, aligned, and used with an implant library to connect the prostheses to titanium bases. A CAD/CAM verification jig confirmed accurate implant position capture. At the second appointment, verification jigs and prototype prostheses were tried in to assess fit, esthetics, phonetics, occlusion, and hygiene access, with minor adjustments as needed. Once approved, the STL files were sent to the lab to fabricate the definitive prosthesis, which consisted of a CAD/CAM-milled monolithic zirconia restoration with a vestibular cut-back to enhance esthetics. The prosthesis was delivered and torqued at the third appointment. The patient reported excellent satisfaction with the treatment, and clinical, intraoral, extraoral, and radiographic examinations revealed no apparent issues (Figs. 17-19).



The patient was followed for 13 months, showing stable functional and esthetic outcomes throughout the follow-up period, with good oral hygiene maintained (Fig. 20).

Treatment outcomes
The patient exhibited stable functional outcomes throughout the 13-month follow-up period, with no signs of implant mobility, peri-implant inflammation, or prosthetic complications. The esthetic result was highly satisfactory, with harmonious integration of the prosthesis into the patient’s smile, natural emergence profiles, and excellent soft tissue support. Both the patient and clinician reported high levels of satisfaction regarding esthetics, phonetics, and masticatory function. The vestibular cutback in the definitive monolithic zirconia restoration enabled enhanced esthetic customization, fully meeting the patient’s expectations.
Patient testimonial: „After losing all my lower teeth years ago and struggling with unstable dentures, I was hesitant about implants. However, the doctors showed me the final result even before starting the treatment, which gave me confidence. I knew my case was complex, but everything was done smoothly and without any problems. Now, I have a stable, beautiful smile and can eat comfortably again without any worries."
Overall, the treatment demonstrated predictable outcomes in terms of implant stability, prosthetic function, and esthetic integration, providing both clinical success and high patient satisfaction. The following images show the before and after results of the treatment (Fig. 21).

Key take-aways
- Early and immediate loading of maxillary and mandibular BLX Full Arch implants with CAD/CAM provisional and definitive restorations can achieve stable functional and esthetic outcomes in complex full-arch cases.
- Digital workflows using Smilecloud and coDiagnostiX®, along with Straumann® RevEX™, enable precise implant position, support predictable prosthetic design, and reduce the number of clinical visits.
- Patient satisfaction is high when treatment provides a stable, comfortable, and esthetically pleasing result, even in complex cases, confirming the effectiveness and reliability of modern implant-prosthetic approaches.

