Author’s testimonial
It was great to plan such a complex case with a full digital approach and see how this planning has been turned into practice with incredible precision. In addition, the Straumann® Novaloc® system was the key to reduce invasiveness by placing implants in the existing bone and then re-align the prosthetic axes for the retention of the removable prostheses.
What is this about?
- How a fully digital workflow including AI-assisted planning, guided surgery, Novaloc® digital workflow components and Smilecloud prosthetic setup can be applied to manage a complex full-arch rehabilitation case even with removable prostheses.
- How Straumann® Novaloc® abutments enable minimally invasive treatment by allowing implants to be placed in available bone while correcting prosthetic angulation for optimal retention.
- What clinical steps and decision-making processes lead to predictable esthetic and functional outcomes in a patient requiring comprehensive maxillary and mandibular restoration. Understand how to approach full-arch mandibular rehabilitation in an elderly patient with advanced periodontal disease and system.
Introduction
Full-arch rehabilitation in patients with a history of failing prostheses, residual roots, and previously misplaced implants presents considerable clinical complexity. Achieving predictable outcomes in such cases requires a treatment approach that integrates accurate diagnostics, prosthetically-driven implant positioning, and minimally invasive surgical protocols. Advances in digital dentistry and modern attachment systems now offer clinicians enhanced precision and flexibility when addressing these multifactorial challenges.
The following case report describes the treatment of a 70-year-old patient presenting with compromised dentition, deteriorating implant-supported restorations, and significant esthetic concerns. Despite these limitations, the patient exhibited favorable bone volume and quality, allowing for a digitally guided, implant-supported rehabilitation. The case was categorized as complex according to the ITI SAC classification due to the extent of dental compromise, the need for multiple extractions, and the requirement for precise three-dimensional implant positioning.
A fully digital workflow was implemented, beginning with intraoral scanning and CBCT AI-assisted segmentation of the maxillary and mandibular arches using coDiagnostiX®. The integration of prosthetic setup data from Smilecloud facilitated a restorative-driven planning approach, ensuring harmonization between implant trajectories, bone anatomy, and the intended esthetic outcome. This digital methodology supported the fabrication of surgical guides, thereby enhancing accuracy during implant placement and reducing the risk of positional deviations.
A critical component of the rehabilitative strategy was the incorporation of the Straumann® Novaloc® retention system. The availability of straight and angulated ADLC-coated abutments allowed implants to be positioned in areas of optimal bone availability while subsequently correcting divergence to achieve appropriate prosthetic alignment. This approach reduced the need for bone augmentation and contributed to a less invasive overall treatment plan, while ensuring reliable retention for the removable prostheses. The recently released Novaloc® Digital workflow facilitates digital impressions and prosthetic planning.
This clinical report illustrates how the integration of digital planning tools and modern attachment technologies can improve precision, reduce procedural complexity, and support predictable functional and esthetic outcomes in demanding full-arch rehabilitations.
Initial situation
The patient was a 70-year-old woman who presented with the chief complaint of wanting to restore her ability to smile and chew comfortably. Her main expectation focused on improving esthetics, as she had expressed dissatisfaction with her dental appearance and wished to regain a natural, confident smile. She reported no systemic risk factors, was classified as ASA I, and was a non-smoker (Figs. 1,2).
Her dental history included multiple extractions, misplaced implants, and dental decay. Clinically, she demonstrated good plaque control and minimal soft tissue inflammation, although several remaining roots were present in both the upper and lower jaws. In the maxilla, the patient presented with an implant-supported removable prosthesis, and in the mandible, a fixed bridge, both of which were in poor condition (Fig. 3).
After removing the upper jaw prostheses and the lower jaw bridge, the remaining teeth were found to be compromised. Some malpositioned implants were displayed in both arches (Figs. 4-8).
Radiographic assessment showed adequate vertical and horizontal bone dimensions with good bone quality.
The prognosis of the remaining teeth was unfavorable due to compromised roots and decay. According to the ITI SAC classification, this case was considered complex.
Treatment planning
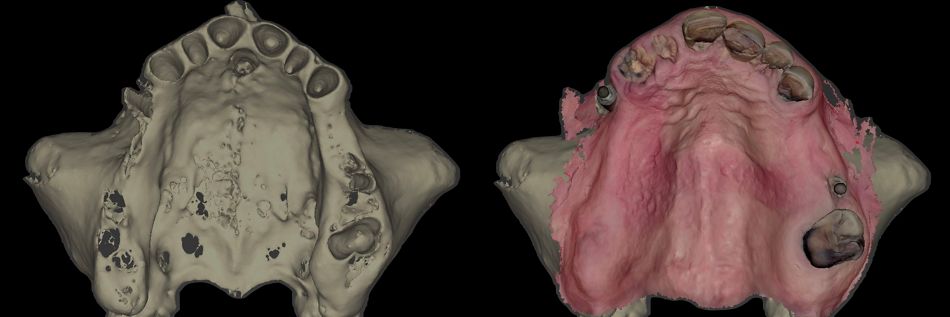
1. Data Acquisition: Initial scan of the upper jaw as the starting point (Figs. 9,10) along with intraoral and extraoral pictures.
2. Smilecloud Analysis: Upload of images and STL files into Smilecloud and creation of a new smile, also thanks to AI tools. The 2D “before and after” images were animated into a 3D preview with Smilecloud YES, allowing the patient to immediately understand the practical application of what had been virtually planned.
3. Creation of a 3D dental set-up in Smilecloud: Once the proposed new smile was approved, an STL file was generated and exported (Fig 11).
4. coDiagnostiX® Planning:
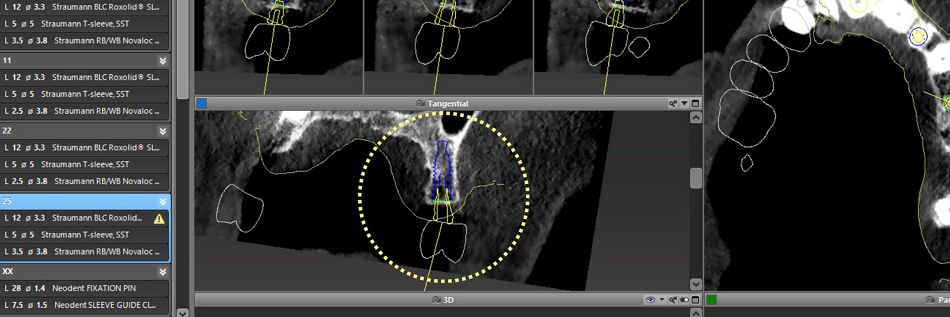
- Segmentation of the bone using AI and superimposition of the intraoral scan file (Fig. 12).
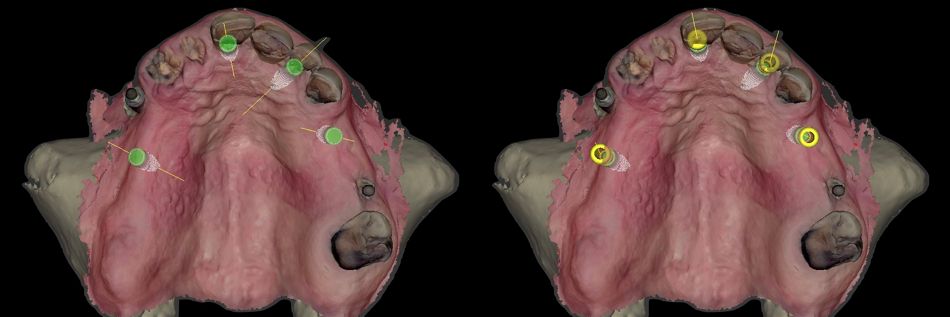
- Positioning of implants and Novaloc® abutments (Fig. 13).
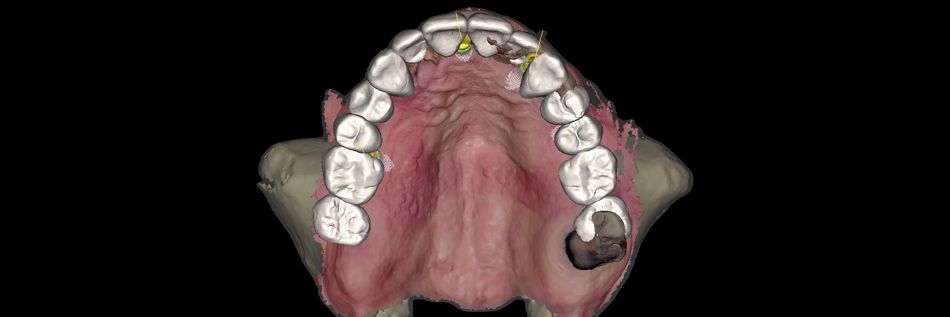
- Superimposition of dental setup coming from Smilecloud (Fig. 14).
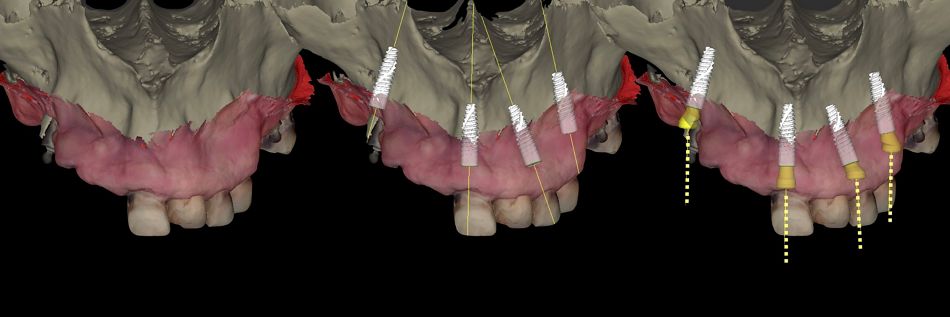
- Implant placement and Novaloc® abutment realignment following the ideal prosthetic axis (Fig. 15).
- Detailed prosthetic realignment confirmed in coDiagnostiX® (Fig. 16).
5. Extractions of hopeless teeth: Teeth were carefully extracted using an atraumatic and strategic approach.
6. Placement of surgical guides: Proper seating and accurate fit were confirmed.
7. Implant placement: At sites 16, 11, 22, and 25, Straumann® BLC™ Ø 3.3 mm Regular Base, 12 mm length, SLActive® surface; at site 34, a Straumann® BLC™ Ø 3.3 mm Regular Base, 12 mm length, SLActive® surface; and at site 43, a Straumann® BLC™ Ø 3.3 mm Regular Base, 10 mm length, SLActive® surface.
8. Guided bone regeneration: Dental bone grafting material was used for guided bone regeneration (GBR) in the post-extractive implant sites 11, 22, 34 and 43.
9. Installation of the provisional
10. Final prosthetic rehabilitation: Using the Straumann® Novaloc® Abutments.
Surgical procedure
The procedure began with the extraction of teeth 13, 12, and 11 under local anesthesia, followed by thorough debridement of the extraction sites (Figs. 17,18).
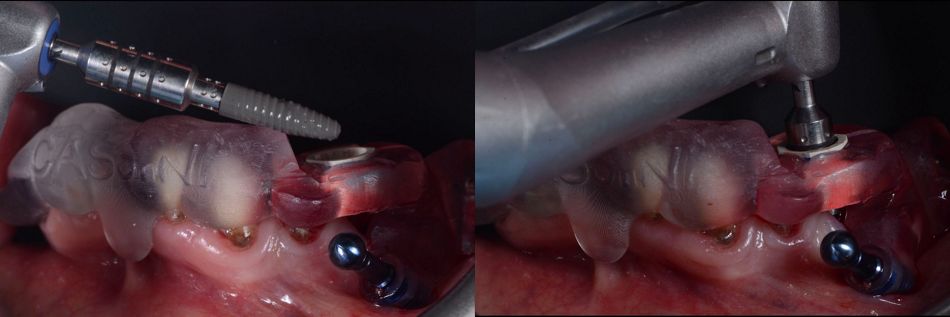
Next, the surgical guide was positioned and stabilized using the remaining teeth and implants as support, ensuring accurate fit and proper seating before proceeding (Fig. 19).
The planned implant sites were then marked. After removing the guide, small flaps were elevated at the previously marked sites 16 and 25 to facilitate access (Figs. 20,21).
The surgical guide was placed, and fixation pins were inserted to secure them in position. The implants were placed following the manufacturer’s recommended protocol. At sites 16, 11, 22, and 25, Straumann® BLC™ Ø 3.3 mm Regular Base, 12 mm length, SLActive® surface implants were placed (Figs. 22-26).
Once the implants were inserted, the guide was removed, and tooth 21 was extracted (Fig. 27).
Subsequently, the following abutments were placed: RB/WB Novaloc® ADLC straight, Ø 3 mm, GH 2.5 mm, TAV for implant site 11 (Figs. 28,29).
RB/WB Novaloc® ADLC angulated 15°, Ø 3 mm, GH 3.5 mm, TAV for implant site 22 (Figs. 30,31).
RB/WB Novaloc® ADLC angulated 15°, Ø 3 mm, GH 2.5 mm, TAV for implant site 25 (Figs. 32,33).
RB/WB Novaloc® ADLC angulated 15°, Ø 3.8 mm, GH 3.5 mm, TAV for implant site 16 (Figs. 34,35).
Dental bone grafting material was used for GBR in the post-extractive implant sites 11 and 22.
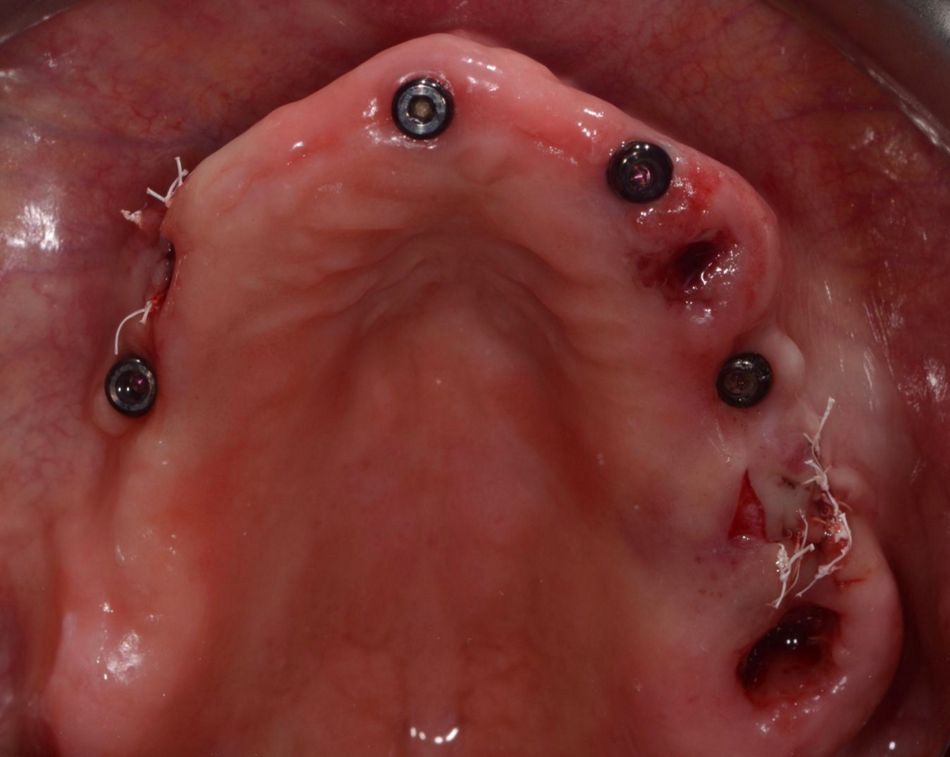
The flaps at sites 16 and 25 were then closed with sutures, ensuring an adequate amount of keratinized tissue on the buccal side of the implants (Figs. 36,37).
It was important to check the lack of contact between the Novaloc® abutments (used in this case as healing caps) and the prosthesis.
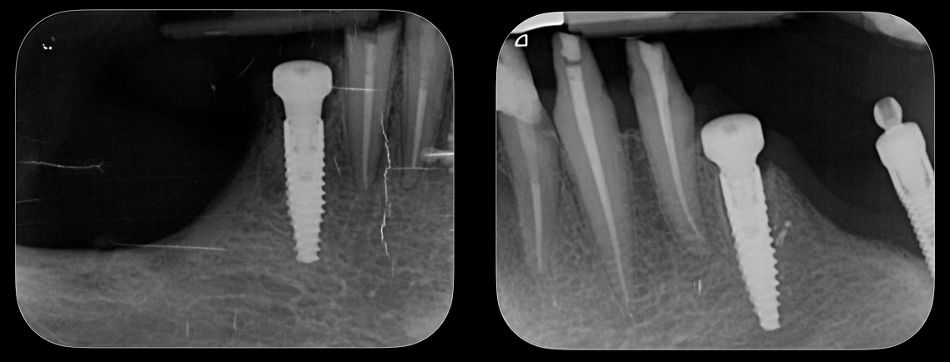
The postoperative x-ray images confirmed the precision of the implant placements in sites 16, 11, 22 and 25 (Fig. 40).
At the 45-day follow-up visit, the upper jaw showed uneventful healing. Frontal and occlusal views indicated stable tissues and satisfactory postoperative outcomes (Figs. 41,42).
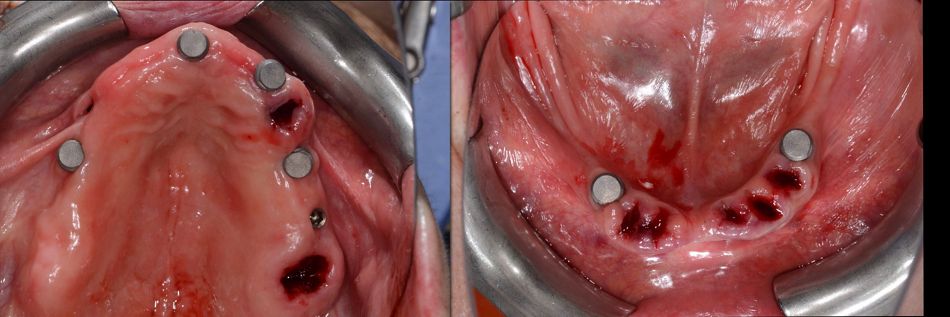
The lower jaw was then treated under local anesthesia. Prior to the surgical phase, the prosthesis was removed, followed by the extraction of teeth #34 and #43 (Figs. 43,44).
For the lower jaw, implants were placed using a surgical guide following the planned drilling protocol (Figs. 45,46).
Implant placement was performed using Straumann® BLC™ implants: a Ø 3.3 mm Regular Base, 12 mm SLActive® implant at site 34 and a Ø 3.3 mm Regular Base, 10 mm SLActive® implant at site 43 (Fig. 47).
Dental bone grafting material was used for GBR in the post-extractive implant sites 34 and 43.
Healing abutments were placed, and primary stability of the implants was confirmed. Postoperative evaluation after immediate flapless implant placement showed stable soft tissues at the surgical sites, with minimal trauma observed (Fig. 48).
Postoperative radiographs of the lower jaw were taken following implant placement, confirming proper positioning and angulation of the implants (Fig. 49).
The pre-existing bridge was used as a provisional after adjustment.

A Center of Dental Education (CoDE) is part of a group of independent dental centers all over the world that offer excellence in oral healthcare by providing the most advanced treatment procedures based on the best available literature and the latest technology. CoDEs are where science meets practice in a real-world clinical environment.
Prosthetic procedure
The patient returned for a follow-up three months after the placement and healing of the upper and lower implants. Examination showed healthy surrounding tissues, osseointegrated implants, and no signs of inflammation or complications. X-ray images taken at this stage confirm the quality of osseointegration in the upper and lower jaws (Fig. 50).
Healing appeared satisfactory, and the case was ready to proceed to the prosthetic phase (Figs. 51-54).
The healing screws in the lower jaw were removed and replaced with straight (0°) Novaloc® abutments, preparing the implants for the next stage of prosthetic restoration (Fig. 55).
X-rays taken at this stage showed the precise positioning of Novaloc® abutments (Fig. 56).
The seating surfaces of the Novaloc® abutments were verified, ensuring they were free of residue and dry. The Novaloc® Scanbodies were then placed on each Novaloc® abutment and pressed down firmly to ensure proper seating (Figs. 57,58).
Printed models were fabricated from intraoral scans, and the final upper and lower removable prostheses with a resin and metal framework were prepared in advance, prior to the extraction of the remaining teeth and removal of failed old implants (Figs. 59,60).
The upper and lower prostheses were evaluated, with occlusal and basal views of the lower prosthesis taken prior to the placement of the Novaloc® matrices (Figs. 61,62).
In the upper and lower jaws, the remaining teeth were extracted, and the Novaloc® matrices were positioned (Fig. 63).
In the upper jaw, the remaining old implants were extracted (Fig. 64).
The Novaloc® matrices were connected to the upper and lower prostheses (Fig. 65).
Final rehabilitation of the upper and lower jaws (Figs. 66,67).
View showing the upper and lower prostheses fitted with Novaloc® matrices (Fig. 68).
The patient’s smile after final prosthetic rehabilitation (Fig. 69).
The patient’s appearance was noticeably improved, and she was very pleased with the result. She appeared cheerful and satisfied, clearly happy with how everything turned out (Fig. 70).
Treatment outcomes
The case was planned and carried out using a fully digital workflow, achieving precise implant placement and prosthetic alignment. The Novaloc® system helped reduce invasiveness by allowing implants to be placed in the existing bone while adjusting the prosthetic axes for the removable prosthesis. The patient was very happy with the result, noticing a significant improvement in both appearance and function, and was impressed by how the digital approach enhanced her smile.
Take-aways
- Fully digital workflows allow precise planning and execution of complex implant and prosthetic cases, improving accuracy and efficiency.
- Minimally invasive systems like Novaloc® can optimize implant placement and prosthetic alignment, reducing surgical trauma while maintaining prosthesis retention.
- Patient-reported outcomes highlight high satisfaction with both esthetics and function, demonstrating the effectiveness of digital approaches in enhancing smiles.
Acknowledgements:
The author would like to express his sincere gratitude for their invaluable contributions to:
- Dr. Federico Chiari, DDS, pre-surgical treatment and conventional planning
- Dr. Luca Repetto, DDS, digital planning
- Mr. Alessandro Giacometti, DT, laboratory procedure