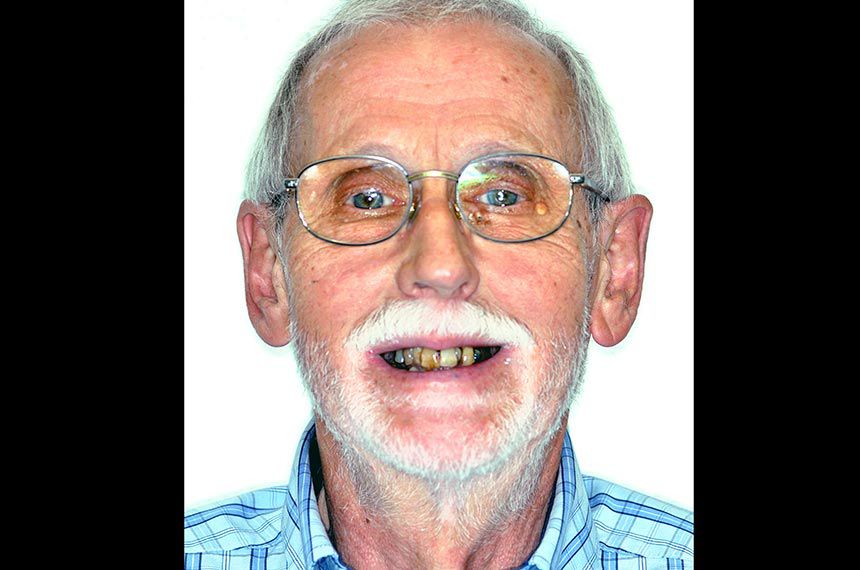
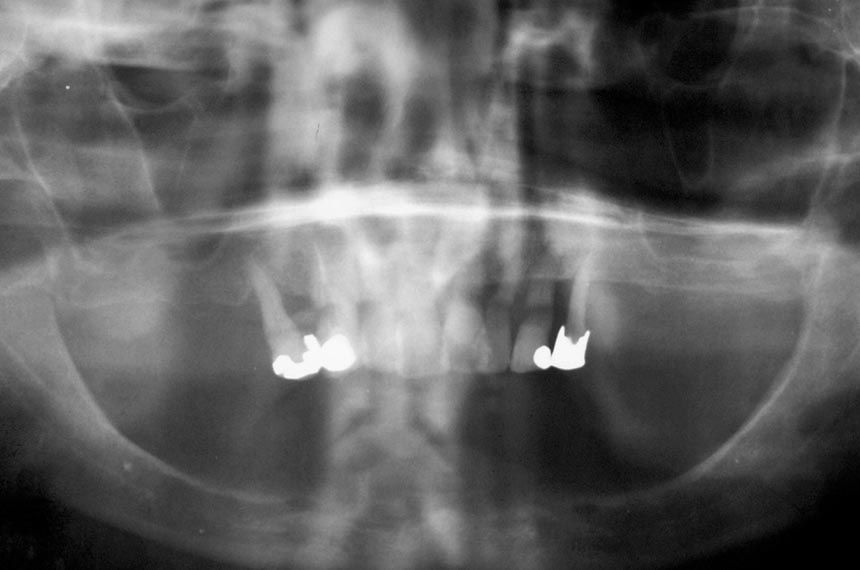
The 72-year-old healthy male patient presented at our practice in mid-2014 with the aim of improving his dental situation (Fig. 1). His quality of life was substantially impaired by his very mobile upper and lower dentures. He wanted to improve his appearance and, in particular, achieve a stable fit of his dentures, ideally by fixed implants in the upper and lower jaws. The upper jaw showed residual dentition with a very poor and unsightly periodontal situation (Fig. 2). In the lower jaw there was a complete denture on a severely atrophied bone ridge (Fig. 3).
Treatment planning
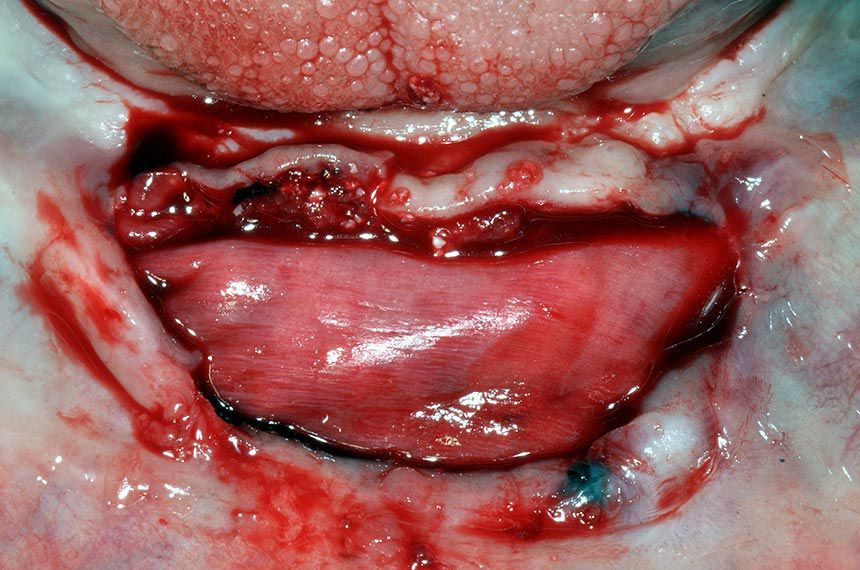
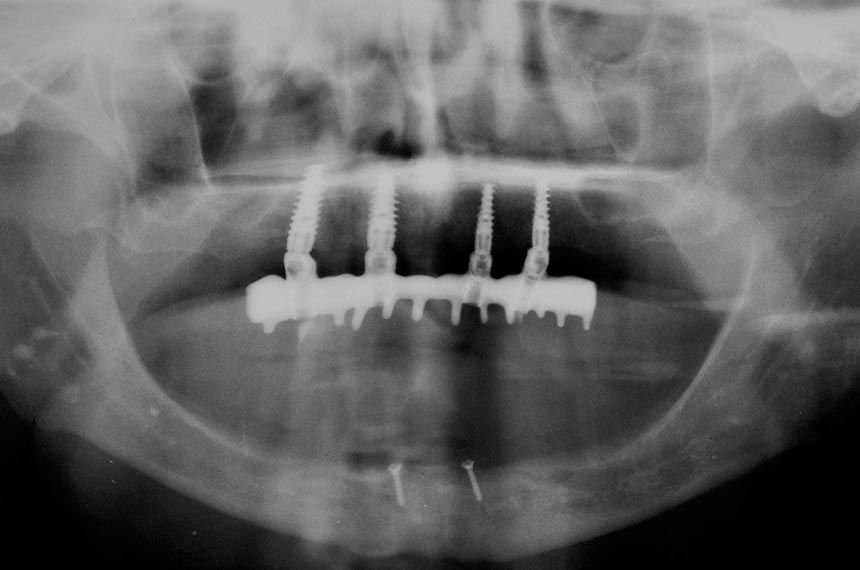
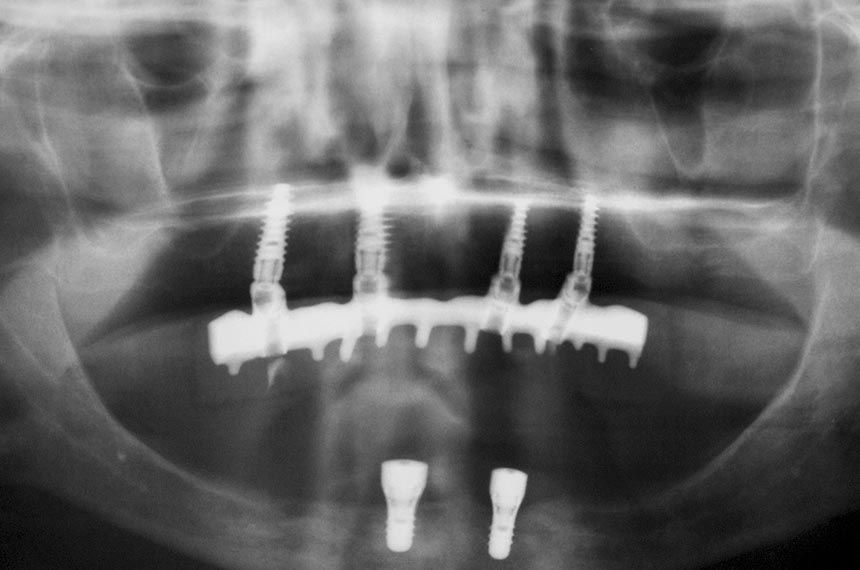
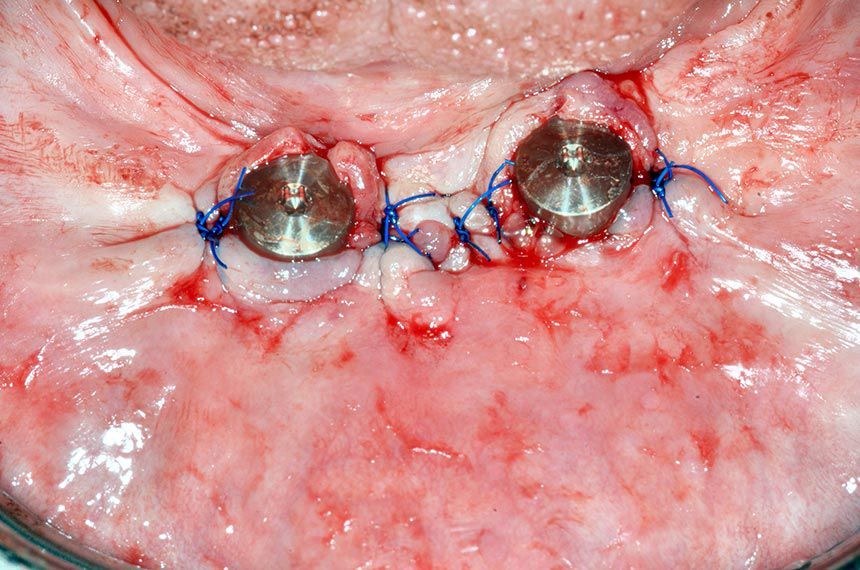
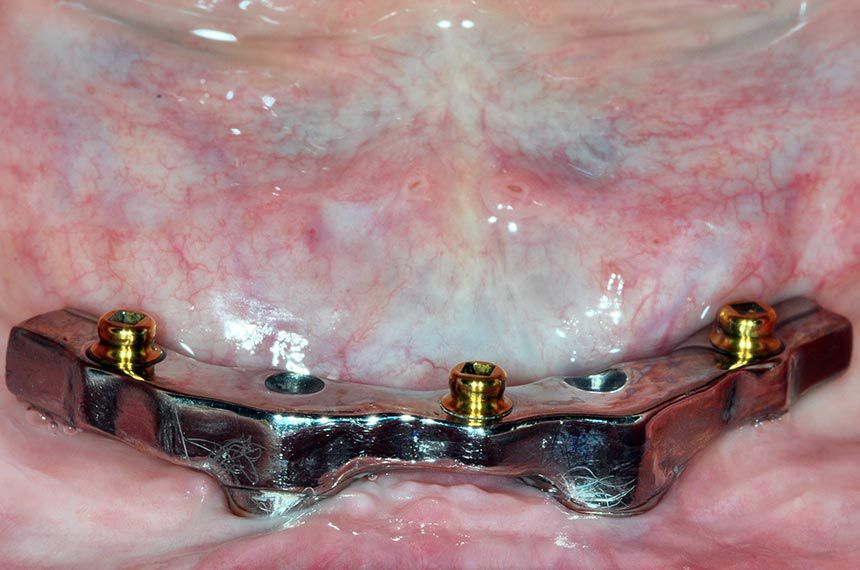
Since the volume and quality of bone in the upper jaw were satisfactory (type II according to Lekholm and Zarb criteria), following extraction of the residual teeth with a poor prognosis, we opted for a fixed prosthesis on four implants. The initial situation in the lower jaw was more difficult. The severely atrophied edentulous lower jaw and the close proximity of the bone to the inferior alveolar nerve meant that implants were possible only in the interforaminal area (Fig. 4). The bone resorption was even clearer on a CBCT scan. We therefore decided to proceed with a substantial interforaminal bone augmentation prior to implant insertion. First of all, the upper jaw was provided with an ideal solution in terms of both function and esthetic appearance. During this time the lower jaw was adapted accordingly in preparation for the definitive implant provision in a second step. Since the implant provision for the lower jaw represented the greater challenge in this patient in terms of anatomy, surgery and implantation, this case report will focus only on the procedure for the lower jaw.
Planning
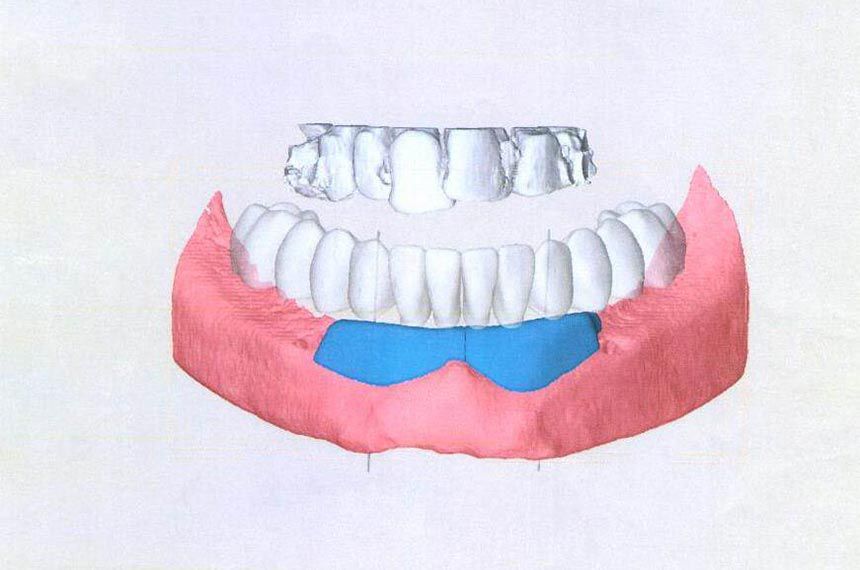
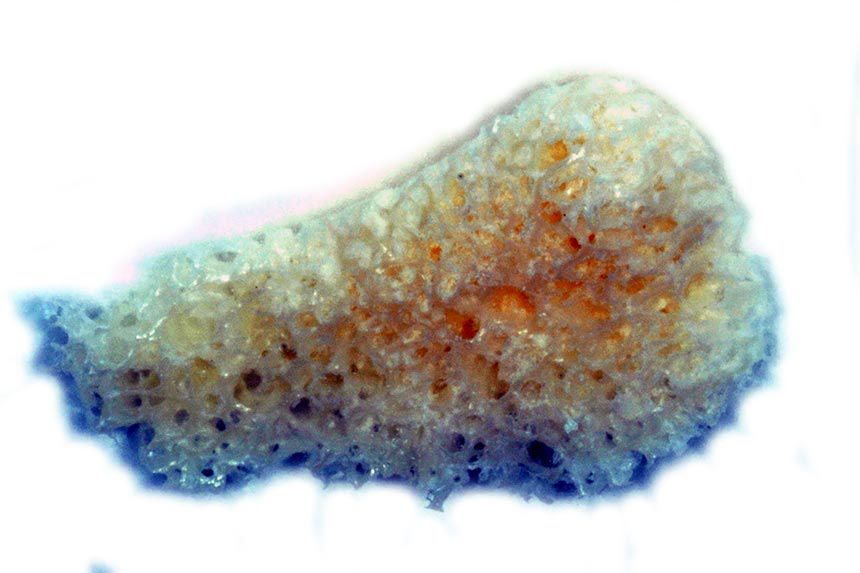
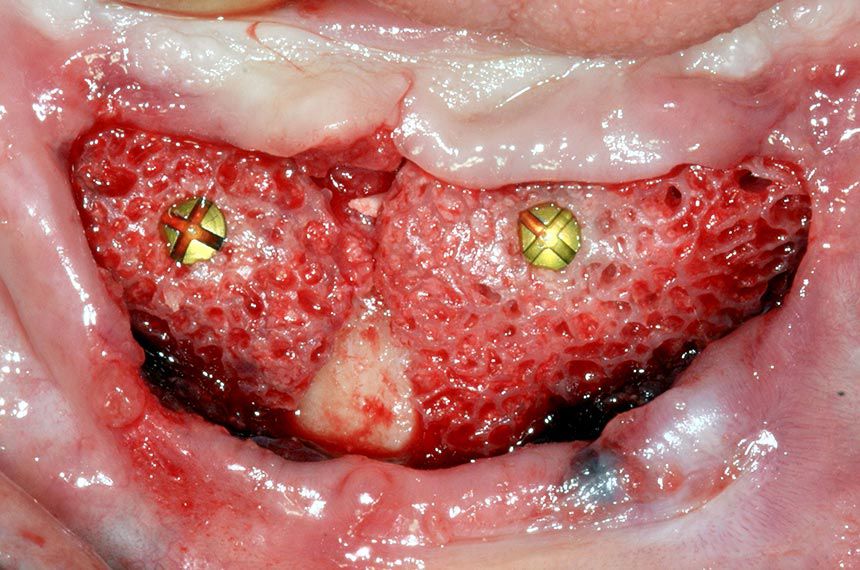
In order to obtain sufficient bone for the augmentation in the lower jaw and avoid any morbidity associated with iliac crest bone harvesting in this patient, we opted for the allogeneic bone augmentation technique proposed by the company botiss. The detailed planning included a CBCT scan and the virtual transmission of the ideal prosthetic arrangement of the lower jaw teeth (Fig. 5). The position of the implants was defined and the required bone material calculated. The data was then transmitted to botiss, who prepared our custom-made blocks from bone tissue (Fig. 6).