Abstract
This case report from Dr. Benjamin Kurfürst, Dr. Lea Hoffmann and Prof. Dr. Dr. Dirk Nolte describes the oral rehabilitation of a patient who had hypodontia, with four missing premolars and ankylosed and infra-position deciduous molars as well as two impacted, displaced canines, which were found to be ankylosed on exposure. The asymmetry of this dentition made it difficult to treat; treatment was approached in close collaboration between the orthodontist and maxillofacial surgical team.
In adolescence, techniques of autologous premolar transplantation and surgical luxation were selected to resolve the defects in the upper and lower jaw. This allowed the orthodontist to restore symmetrical distribution of the existing teeth and to prepare the dentition for later implant treatment once the patient reached adulthood.
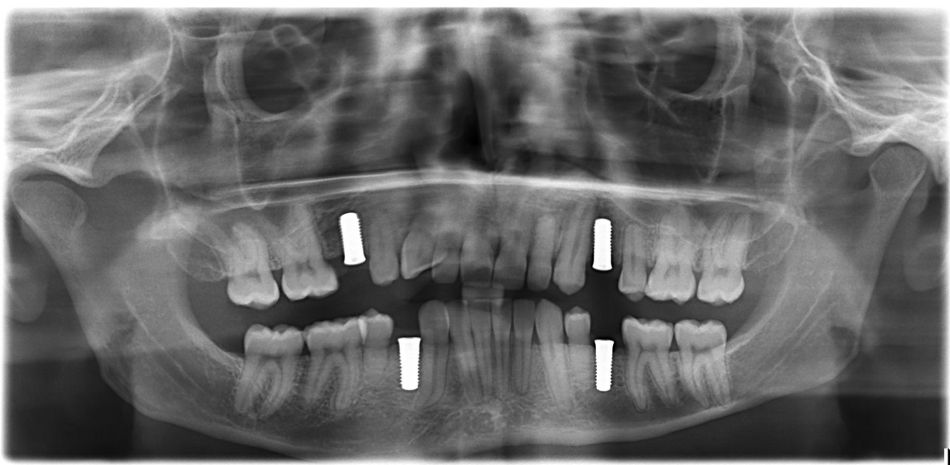
Once skeletal growth was completed, the orthodontic therapy had progressed to the point that after the appropriate prosthetic planning, the remaining gaps were prepared for later insertion of ceramic implants.
The follow-up time for the patient case is now 8 ½ years since the start of therapy.
With early interdisciplinary planning and treatment intervention, the patient's complex malocclusion could be treated successfully both in terms of function and esthetics using the aforementioned surgical techniques.
Introduction
The male patient was 14 years old when he first presented to us in 2013. His general health was unremarkable, and he is not known to have any syndromes. There were also no known cases of craniofacial growth abnormalities in his family, and specifically no information on oligodontia.
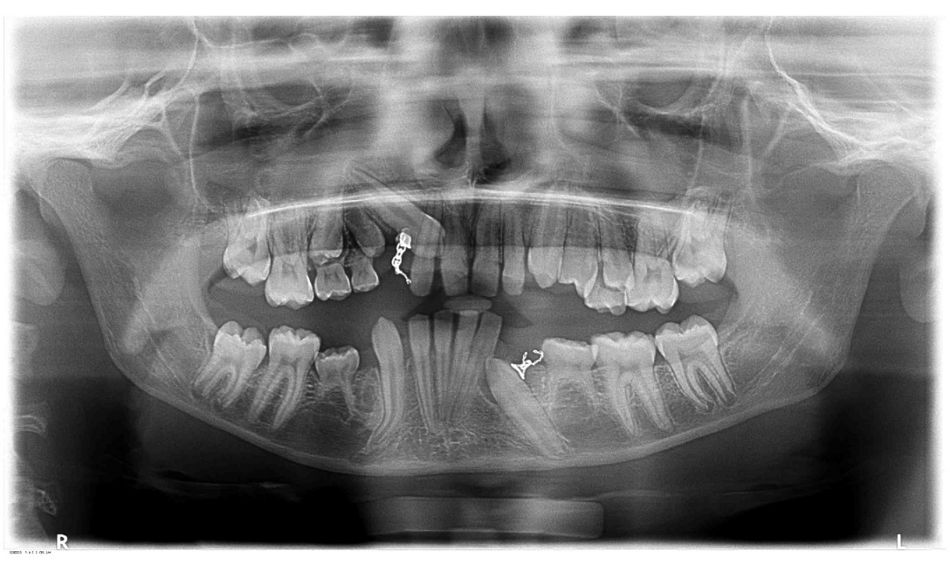
The orthopantomogram (OPG, Fig. 1a) showed aplasia of teeth 34, 35, 44 and 45 (n=4). Teeth 13 and 33 are impacted and displaced; they were already exposed at a different clinic and orthodontic extrusion therapy showed that they were ankylosed (developmental disorder total: n=6). Both canines still have brackets and wires (Fig. 1b and c). The orthodontist discontinued treatment to move the canines and an alternative treatment route was explored. It was documented that this orthodontic treatment attempting to adjust the position of the canines had taken 1.5 years.