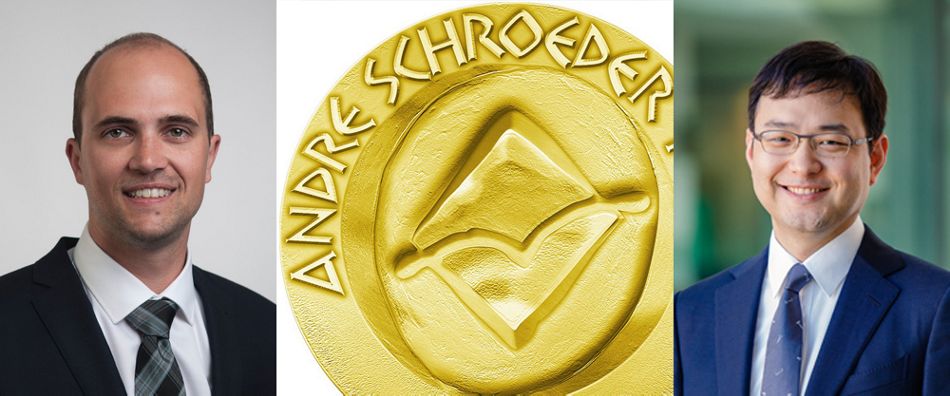
Winning this Prize allows the researchers to make their work known to a broader public and opens doors and opportunities for their careers. This year, the winners were Ryan Lee from Australia and Stefan Bienz from Switzerland.
Ryan Lee and his co-authors received the Prize for Preclinical Research for their study entitled "Re-establishment of macrophage homeostasis by titanium surface modification in type II diabetes promotes osseous healing."
Stefan Bienz and his team received the Prize for clinical research on "Clinical and histological comparison of the soft tissue morphology between zirconia and titanium dental implants under healthy and experimental mucositis conditions—A randomized controlled clinical trial."
We asked the winners to give us a brief insight into their studies and how their scientific contributions will help dentistry and future dental research.
Could you summarize the findings of your study?
Ryan Lee: The research topic was to investigate the effects of different implant surface characteristics on immune cells, particularly macrophages, in an experimental model of diabetes. The implant surfaces we used were SLA and SLActive. It has been well documented that the SLActive surface enhances the rate of osseointegration at the early stage of osseous healing, however the underlying mechanisms have not been fully elucidated. I was intrigued by this particular biological phenomenon, and I started asking (research) questions about interactions between the cells involved in wound healing and different biomaterials. The macrophage is truly a versatile immune cell that can orchestrate inflammatory responses via its phenotype expression; pro-inflammatory M1 or anti-inflammatory M2 phenotype. Evidently, this is over-simplified, but its role in wound healing is crucial. Immunomodulatory effects of implant surfaces in association with different macrophage phenotypes are still poorly explored in vivo, especially, under compromised systemic conditions, like diabetes. Hence, the study investigated the interactions between macrophage phenotypes (M1 and M2) and different titanium implant surfaces (SLA and SLActive) under Type 2 diabetic conditions.
Apply for the André Schroeder Research Prizes 2023 by September 15
If you have new findings in implant dentistry, oral tissue regeneration, and related fields, check the application requirements and apply now!
Stefan Bienz: The project's rationale was to evaluate the soft tissue morphology around zirconia and titanium implants. Zirconia appears to be a very promising material at the level of the soft tissues, some studies indicated less plaque accumulation, and there were preclinical studies that reported a more favorable soft tissue integration. Therefore, the study's main goal was a comparison at the soft tissue level, not a comparison of the osseointegration or the prosthetics. We are proud of the study design, including a within-subject control and an experimental mucositis phase where patients omitted cleaning for three weeks. The primary outcome, inflammatory cells evaluated by histomorphometry, was not significantly different.
Furthermore, the study did not confirm differences in terms of the length of junctional epithelium and other parameters as indicated by preclinical studies. However, the clinical measurements have revealed more plaque around titanium implants in case of the absence of oral hygiene, and in the same context, bleeding on probing increased more around titanium implants as compared to zirconia implants. The conclusion was that both implants rendered similar outcomes under healthy conditions, but lower plaque and bleeding scores were detected for zirconia implants under experimental mucositis conditions. Histologically, only minimal differences were observed.
How would your findings contribute to dentistry and future research?
Ryan Lee: As clinicians, we are dealing with wound healing every moment when we see patients. The current study has provided a valuable insight into the interaction between biomaterials and immuno-inflammatory responses in a compromised systemic condition. As this was a preclinical study, it obviously warrants further studies to confirm. Still, it has highlighted the importance of inflammation response control at the initial phase of wound healing, including osseointegration, and the biomaterials we use daily have a capacity to modulate the immune responses. In this regards, future implant dentistry research should focus on these immuno-modulatory effects of biomaterials. Wound healing is an essential aspect of implant dentistry, and host-modulation by biomaterials will be of our great research interest for improvement of clinical outcomes.
Stefan Bienz: If we consider that an implant should serve for many years, we have to acknowledge that it is very likely that our implants will experience the condition of mucositis from time to time. This is confirmed by the prevalence calculated from large-scale studies with hundreds of patients. And in this particular situation, zirconia seems to offer a certain advantage over titanium. This can also be achieved by using zirconia abutments on titanium implants. The rationale for using two different implants in the study with an almost similar design was to avoid as many confounding factors as possible.
Surface modifications to further improve soft tissue integration will be of high interest in future research, maybe for both materials. In addition, it is important to keep in mind that this study did only focus on the biological point of view. From the technical side, there are still limitations when using ceramics, mainly in regards to connections and some other prosthetic aspects.