Introduction
Tooth extraction and long-term edentulism can cause deficient alveolar bone and horizontal and vertical ridge defects, representing esthetic and functional challenges for implant placement. Ridge augmentation may be carried out simultaneously with, or prior to, implant placement if implant stability or appropriate positioning cannot be achieved1. A sufficient volume of healthy bone should be present at potential implant sites to expect a predictable long-term prognosis for osseointegrated implants2.
A number of techniques, such as ridge-splitting, guided bone regeneration (GBR) procedures, autologous bone transplantation, and the use of bone substitute materials, have been introduced. They have shown promising results in the correction of bone defects in the alveolar ridge3.
GBR is the gold standard technique for bone regeneration in patients with atrophic ridges, and it is considered one of the most predictable ridge augmentation techniques4.
The following case report shows how the area of tooth #22, which presented a horizontal and vertical bone deficiency, was rehabilitated using harvesting of an autologous bone block, a GBR technique, and a Straumann® Bone Level implant.
Initial situation
A systemically healthy 58-year-old female patient who reported being a non-smoker and having no allergies came to our clinic seeking a reliable implant treatment. She expressed her situation as follows: “My tooth was extracted three months ago, and now I would like to replace it. I was previously told that it was not possible to place an implant because there was insufficient bone in the area, but I do not want to grind my other teeth to replace the one I lost.”
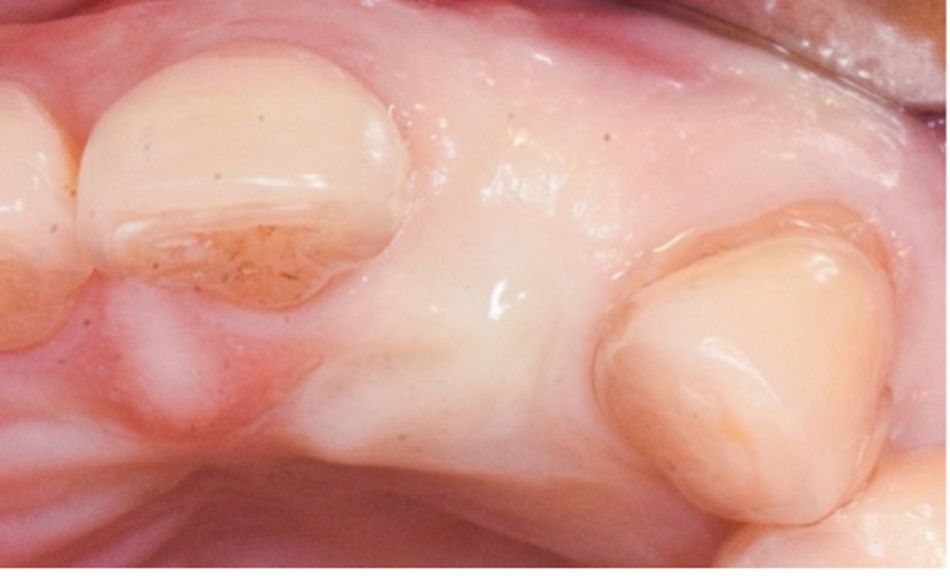
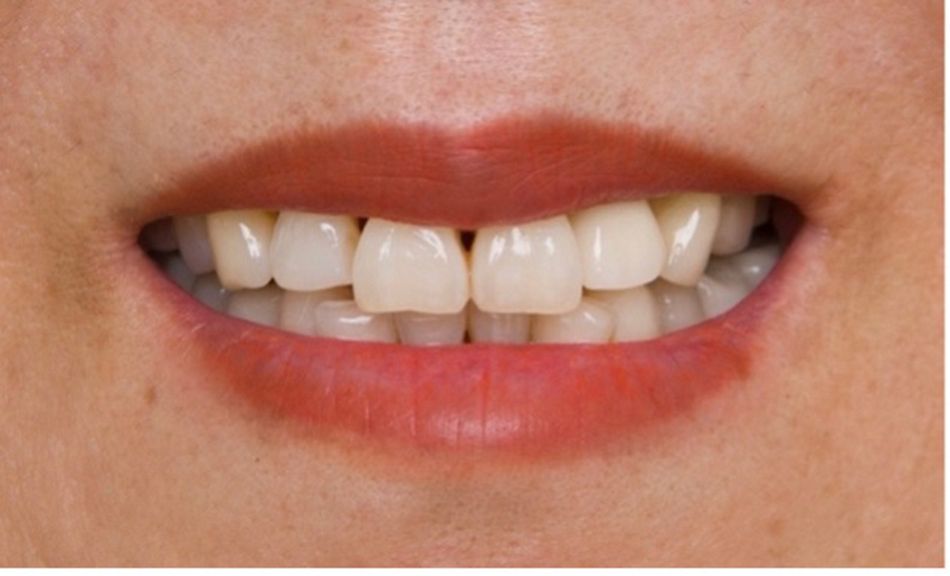
The extraoral examination revealed a high smile line with slightly protruded central incisors and mild gingival recessions with a slight loss of papillae.
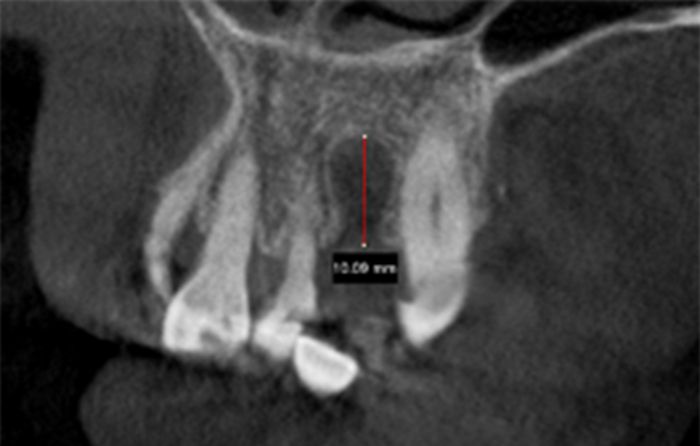
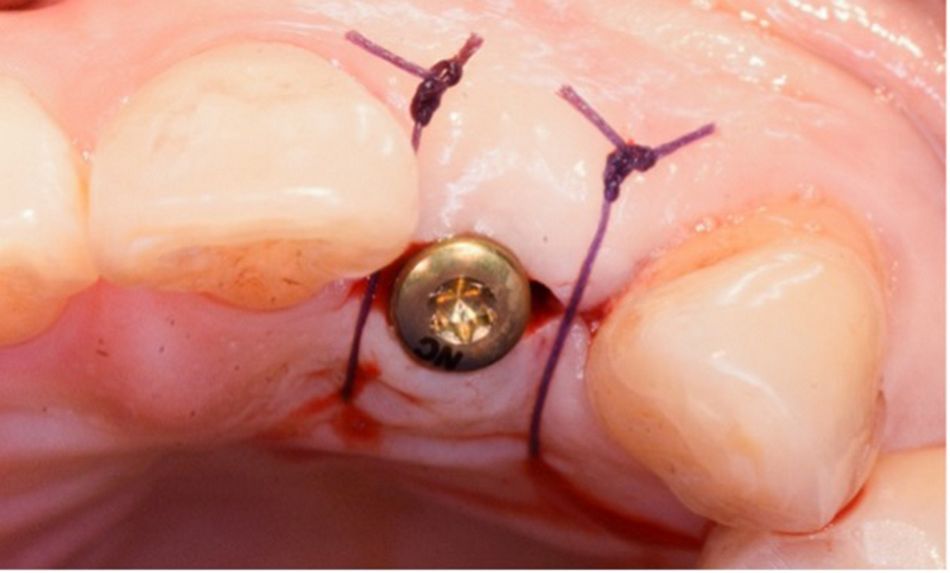
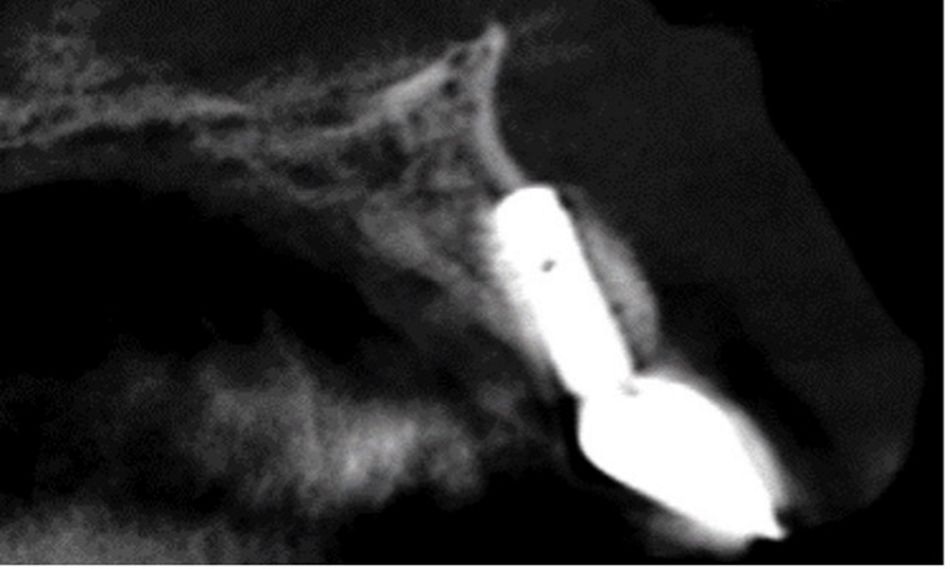
The intraoral examination revealed the absence of tooth #22 and loss of contour of the buccal plate in the area of #22 (Fig. 1). The amount of bone in the edentulous area was determined using CBCT. The CBCT scan confirmed the absence of horizontal bone availability for implant treatment. In addition, there was a vertical defect of 10.09 mm (Fig. 2).