The patient, a 62 year-old female, non-smoker, and in good general health, underwent multiple dental treatments in the past. She came to my practice with an unsatisfactory tooth 21, and wanted this tooth replaced. 21 was previously root-filled and restored with a post and metal-ceramic crown. Radiographically, a gap is seen between the root and post core (Fig. 1), which was consistent with the clinical assessment of a crown-root fracture.
Treatment planning
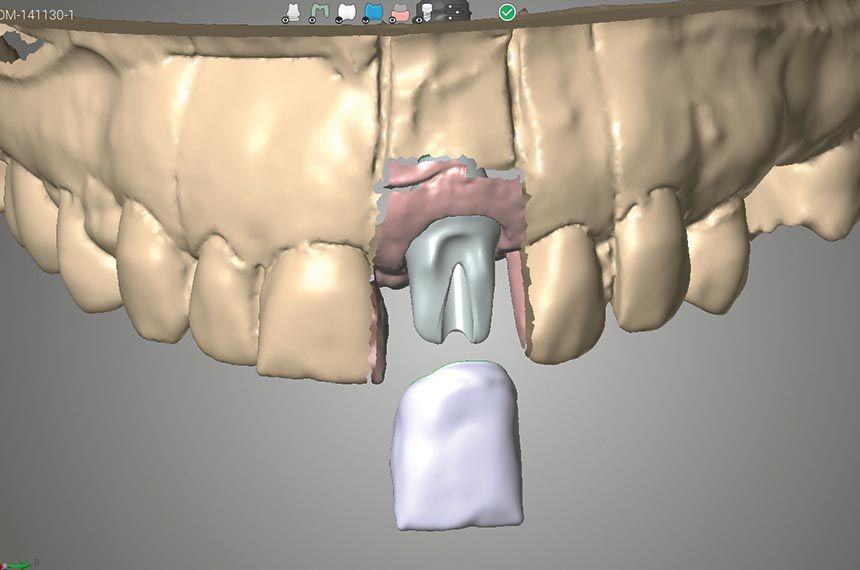
Accurate and thorough treatment planning plays a fundamental role in ensuring a successful treatment outcome. Various treatment options were presented and discussed together with the patient. Tooth extrusion (post/core and crown) leads to very good esthetic results and the tooth can be preserved but the treatment time is prolonged. On the other hand, immediate implantation results in tooth loss, but has the advantages of a good predictable prognosis and long-term result. In the end, the patient opted for implant therapy. Esthetic demands required the use of a strong and fast-healing implant with prosthetic flexibility in order to achieve the desired goal. Since tooth 11 was tilted slightly labially by previous periodontal inflammation, a veneer for this tooth was included in the treatment plan.
Surgical procedure
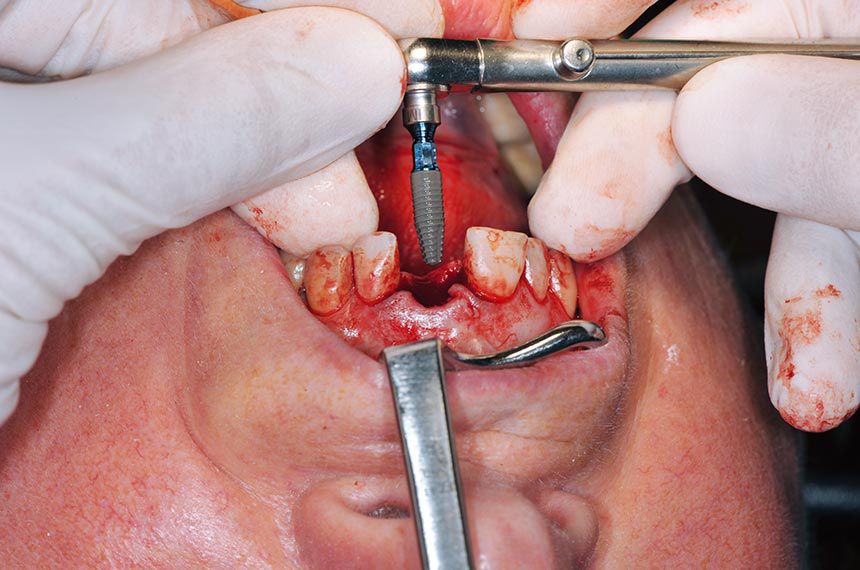
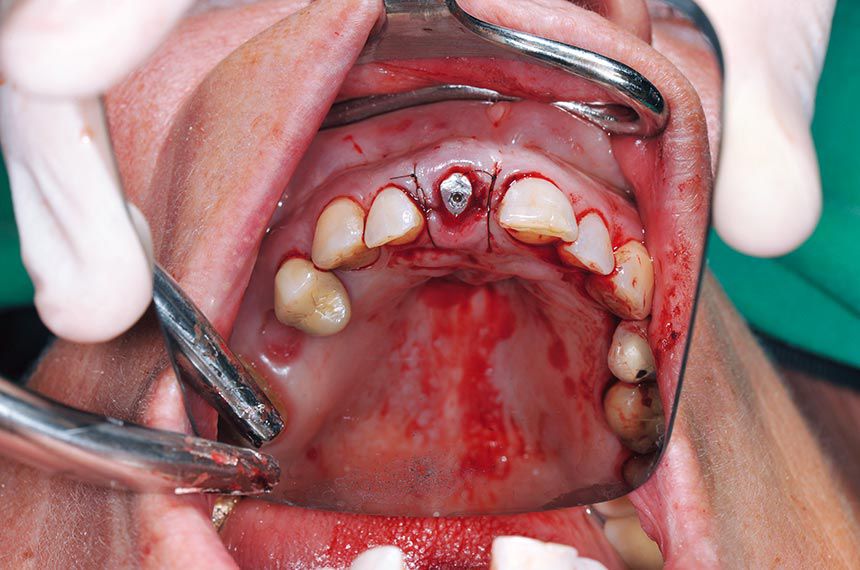
After careful removal of the crown on 21, the initial suspicion of a crown-root fracture was confirmed (Fig. 2). The remaining root was removed with special consideration to preserve the buccal bone lamella. The preparation of the implant bed was carried out with constant contact of the drill on the palatal bone wall, to avoid any damage of the buccal bone lamella and to ensure that the implant position lies behind the esthetic border line. A Straumann® Bone Level Tapered implant (BLT) was selected for better primary stability and to facilitate immediate loading. The implant bed was underprepared at ∅ 2.8 mm to accommodate a ∅ 4.1 mm Straumann® BLT Implant (Roxolid® SLActive® 12 mm). With the aid of alignment pins and the probe, the implant axis and position were checked in relation to the esthetic border line. The implant was placed with the ratchet and torque control device, and sealed immediately with a healing abutment (Figs. 3, 4). The flap was closed with a 5/0 monofilament suture to allow for a period of transmucosal healing. A post-operative radiograph was taken as a reference (Fig. 5).