Immediate implant placement following tooth extraction might be a viable alternative to delayed placement. However, it requires careful case selection. The implant position and the available peri-implant soft tissue become increasingly important in a patient with a high lip line. This case report describes a surgical technique that preserves anterior esthetics, combining minimally invasive extraction, immediate implant placement and provisionalization, grafting of the buccal space and a connective tissue graft from tuberosity.
Patient history
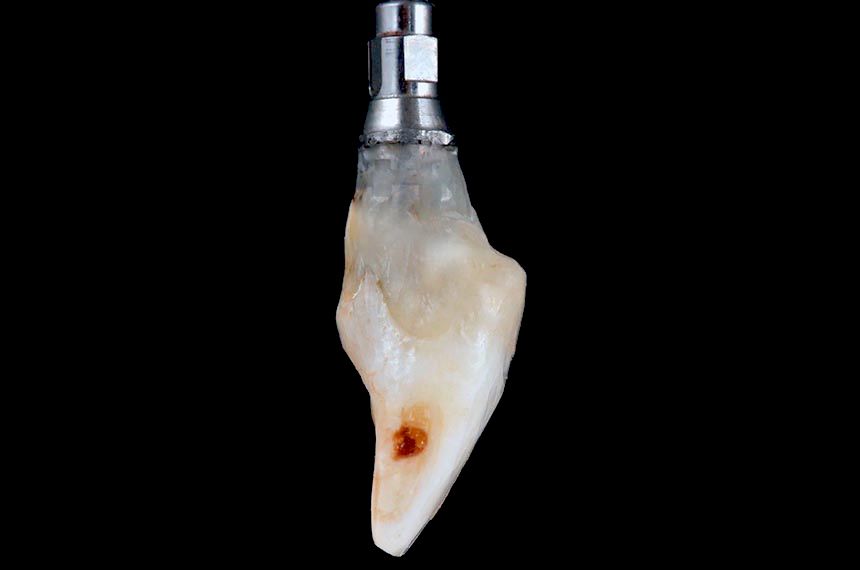
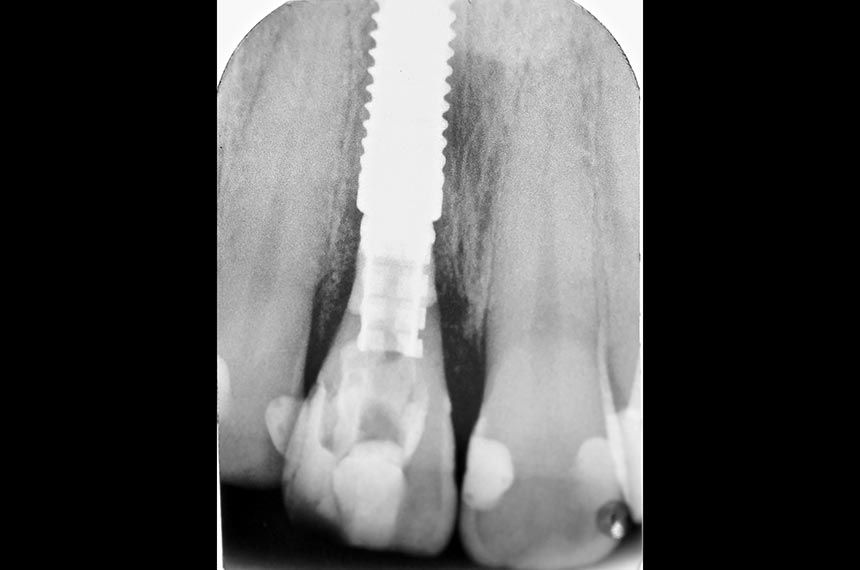
The patient, a 29 year-old Caucasian woman, non-smoker in good general health, was referred to the author’s private dental office with symptoms of vertical root fracture on the maxillary left central incisor (Fig. 1). There was no significant bone loss. The maxillary left central incisor had a history of periapical surgery and endodontic retreatment (Fig. 2). Patient’s oral hygiene was fair. The patient’s history showed no pathological findings and no contraindications with regard to dental implant therapy. The patient has a high lip position that exposes the gingiva so her expectations with regard to the esthetics of the treatment outcome were very high (Fig. 3). It was decided that the maxillary left central incisor should be replaced by an immediate implant.
Surgical procedure