Fig. 1
Courtesy of Camargo/Camargo/Kanashiro – see clinical case report here.
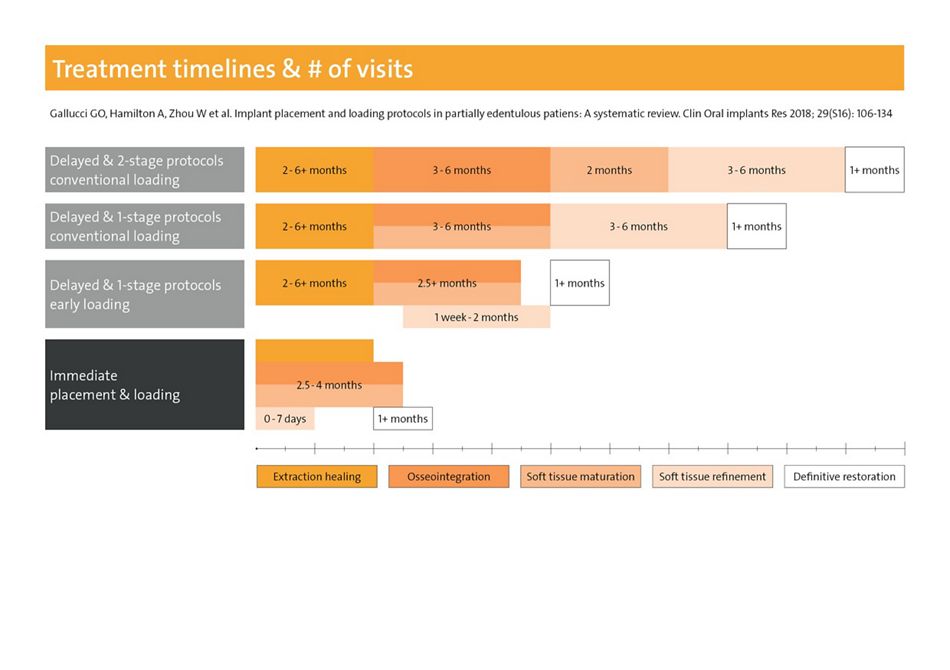
Depending on the chosen protocol, the duration of implant treatment can vary substantially. A 2-stage delayed placement protocol with conventional definitive loading (Type 3C) may take up to two years (Fig. 1) 1. In contrast, an immediate-immediate procedure (Type 1A) with, mostly temporary, restoration can be feasible with no delay, i.e. on the day of surgery. The final restoration can then be scheduled to suit the individual situation, with most cases needing soft tissue refinement in the anterior maxilla.
Based on the number of case reports published in dental media, the latter and other abbreviated protocols have become much more popular in recent years 2. In addition to patient preferences, this is due to an increasing number of digital workflow options 3. In selected cases and with 3D diagnostics available, these workflows allow immediate placement and restoration. They are feasible even without an analogous or digital impression, using only virtual data sets.
Implant placement within 4 months
According to a current ITI Consensus Report, implants should be placed within the first four months after tooth extraction 1. This is “due to the risk of alveolar resorption and reduction in bone volume, as well as the extended treatment time” for Type 4 placement (6 months or longer). Alternatively, a post-extraction (Type 1) or early (Type 2 or 3) implant insertion is preferable. Decisions will depend on diagnostic findings and the expertise of the team.
As far as immediate placement is concerned, tissue preservation does not appear to be the most relevant aspect. Bone remodelling occurs mainly in the central part of the buccal bone. In principle, it cannot be prevented by any of the protocols, including socket grafting 4. However, in selected cases and with the aid of simultaneous hard and soft tissue augmentative measures, a favourable buccal contour is achievable. In these cases, according to the literature, the resulting mean bone level will be situated approximately 1 mm more coronally than without augmentation 5.
“The shares of immediacy has grown over the years because it´s so attractive to patients” Stephen Chen at the Buser Symposium 2019 in Bern, Switzerland
Careful case selection
For patients, and consequently for the implant team, a satisfactory and long-term stable aesthetic result is highly relevant. Cases should therefore be evaluated carefully using suitable guidelines, e.g. the SAC Classification and the ITI Treatment Guide for Implant Placement in Post-Extraction Sockets 6, 7. Recently, the renowned ITI members Urs Belser, Daniel Buser, Vivianne Chappuis and Stephen Chen summarised differential indications for Type 1, 2 and 3 placement 2. According to this review, immediate implants should only be placed “in ideal clinical conditions”, which include an intact buccal bone wall of > 1.0 mm thickness and a thick gingival phenotype 8.
These tissue-related factors determine if adequate soft tissue margins can be achieved in a predictable way, which is not always the case 9, 10.
However, immediate provisionalization of post-extraction implants may help to preserve tissue for good aesthetic results 11, 12. To avoid complications, augmentation of the buccal hard and soft tissues is indicated in practically all instances 4, 13. Other prerequisites for Type 1 protocols include 8:
- adequate bony dimensions of the implant site
- a sufficient primary stability in the range of at least 25 Ncm or ISQ >70
- for immediate restoration, adequate control of functional forces flapless implant placement if possible 2
- patient compliance
Moreover, when the existing bone is limited, small diameter implants with adequate strength and osseointegrative potential may be an option 14. And most importantly, the clinician and his or her team need to be surgically experienced and well trained in implant procedures 2.
Smooth restorative protocols
When immediate implant placement is not an option, treatment time can be reduced using abbreviated restorative procedures. In many cases, after insertion following partial bone healing (after 12-16 weeks, Type 3), immediate or early loading is feasible 1. Although scientific documentation is still limited, when combined with one-stage placement, this protocol leads to a reduced treatment time of approximately 10-12 months (Fig. 1). Another, well documented alternative is to restore the implant conventionally (i.e. within 2 months), following Type 2 placement (4-8 weeks post-extraction) and simultaneous contour augmentation 15.
Time-saving insertion and restoration protocols can be simplified by modern implants. For increased primary stability independent of implant timing and bone quality, specific macrodesigns have been developed 16, 17. In comparison to conventional implants, these implants are designed to improve bone management, e.g. by means of a conical shape with reduced neck diameter, deeply structured threads, bidirectional cutting and bone condensing properties.
To enhance osseointegration, with a focus on secondary stability during bone remodeling (after 2-4 weeks), chemically modified surfaces have been developed 18, 19. This is especially relevant in connection with early loading or in patients with compromised systemic health 20. Although evidence is still limited, the combination of macro, micro and chemical implant features can be expected to increase predictability of immediate and early protocols.
Digital opens fast lanes
Computer-aided implantology is a further important factor which can save time. Based on 3D data from a cone beam computer tomography and an intraoral scan, surgical guides, immediate definitive abutments, gingiva formers, temporary or even final restorations can be designed in dedicated software. These virtual or hybrid workflows allow, for example, the immediate implant-retained temporary restoration of edentulous arches on the day of extraction. Basically, this was possible before the advent of 3D workflows 21. However, the latter appear to have benefits, e.g. in terms of post-operative pain, especially when implants are placed flapless 3.
Last but not least, computer-aided protocols facilitate the chair-side fabrication of implant-retained restorations. With modern equipment, such as intra-oral scanners, practice-based milling machines and 3D printers, patients can be treated in a reduced number of sessions and without the need to order surgical guides or temporary restorations from external partners. Although to date clinical benefits have not been shown in comparison with conventional workflows 22, they are clearly economically relevant, with at least comparable clinical reliability and patient-reported outcomes 3, 23, 24.