This non-smoking patient was healthy and did not take any medication. Soft tissues were quantitatively and qualitatively in good shape (Fig. 1). They were no molars at the mandible. The panoramic X-Ray showed a lack of bone at the posterior part of the maxillae (Fig. 2)
Treatment planning
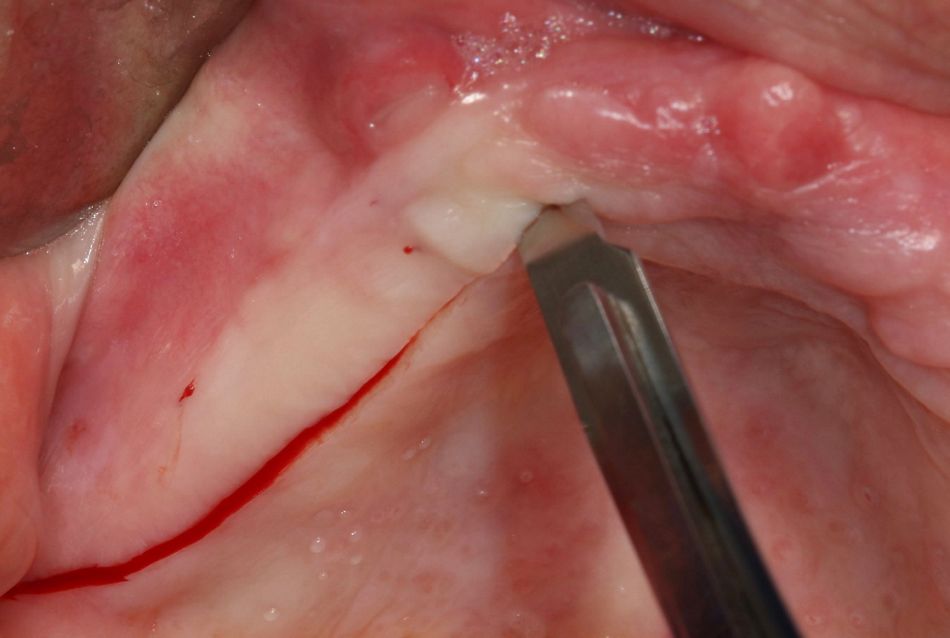
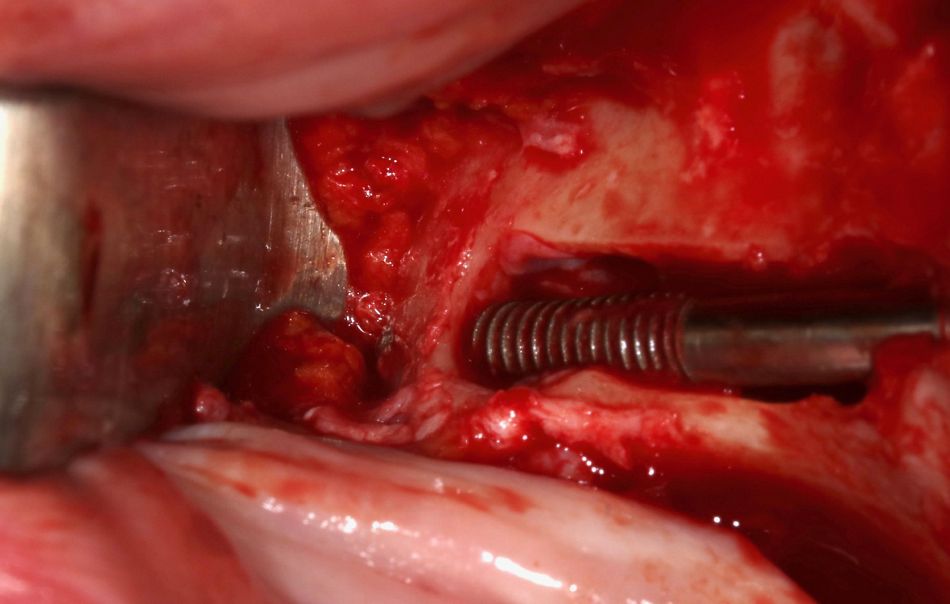
The CBCT showed the presence of remaining bone in the canine region on both sides and confirmed a lack of bone at both posterior parts of the maxilla. A wisdom tooth was foreseen to be removed on the left side, as well as a small piece of root under the mucosa. (Fig. 3,4,5).
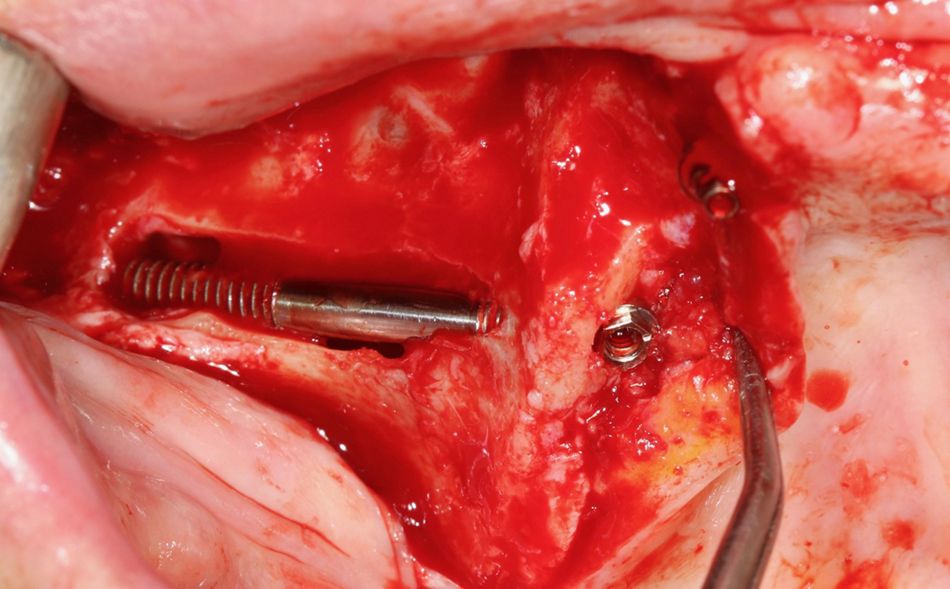
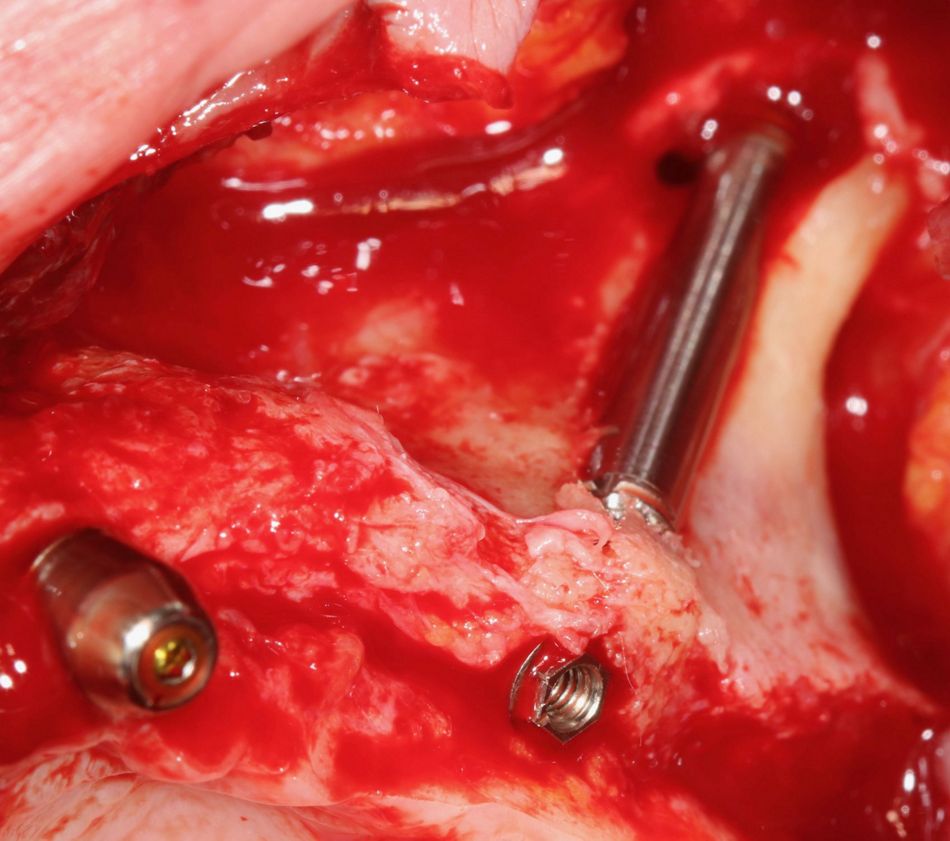
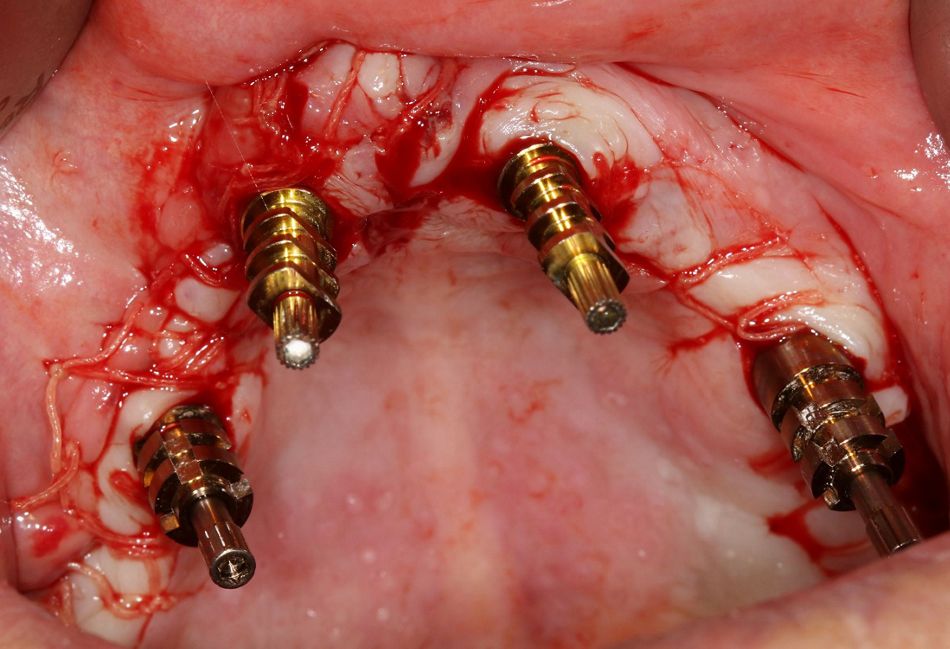
It was decided to place two regular implants in the anterior area, combined with two Straumann® zygomatic implants (one on each side) in order to provide the patient with a fully screwed fixed restoration immediately after the surgery. The anatomical situation in the posterior area was classified ZAGA 1/2 and thus, two round implants were inserted.
The main advantages of this type of implants are as follows:
- The small diameter rough surface at the apex of the implants allows to leave enough space available
- The machined threaded part underneath the abutment permits to steady an excellent initial stability which is decisive to perform securely an immediate loading.
Surgical procedure