Introduction
However, the pre-surgical wax-up preparation, surgical guide, and provisional preparation can be time-consuming and arduous, mainly if the clinician does not have an in-house dental technician or is not well aligned with the lab. On this matter, digital workflows have changed the way we perform immediate treatments nowadays.
Digital dentistry has been improved with technology through the development of software and computerized tomography to enable virtual planning and to guide the surgery toward a specific target precisely. Digital dental implant planning enables a prosthetically driven approach, resulting in better results in terms of the prosthesis design, aesthetics, and occlusion, eliminating the shortcomings and minimizing the misfit of the conventional lab work, among other advantages.
The following case report demonstrates the time chair-time saved and the improved patient comfort when we digitize. Moreover, digital scanning replacing conventional impression-taking created less trauma on the surgical site, thus improving the patient’s experience. Furthermore, 3D printing reduced the cost and time needed for provisional fabrication and allowed an accurate fitting.
Initial situation
A 58-year-old male, who reported being a former smoker for 40 years (10 cig/day), with no medication, or allergies, came to our clinic; and expressed, “I cannot bite with my lower front teeth anymore without hurting. I would like to find a more permanent solution. Not being able to chew has affected my lifestyle tremendously”. In addition, his expectations included a fixed and minimally invasive solution, as he didn’t want to spend a day without teeth.
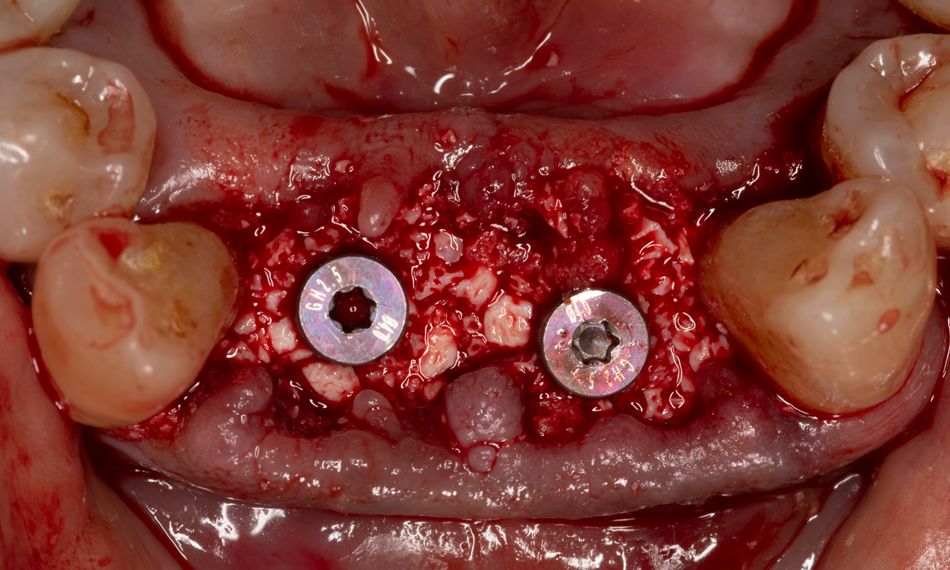
The intraoral examination revealed the absence of teeth #18, #28, #38, and #36. In addition, the clinical assessment showed mobility grade III, calculus, gingival inflammation, bleeding on probing, suppuration, and extrusions associated with teeth #32, #31, #41, and #42 (Fig. 1). Furthermore, large and bilateral bony masses in the premolar region of the lingual mandible were palpated.
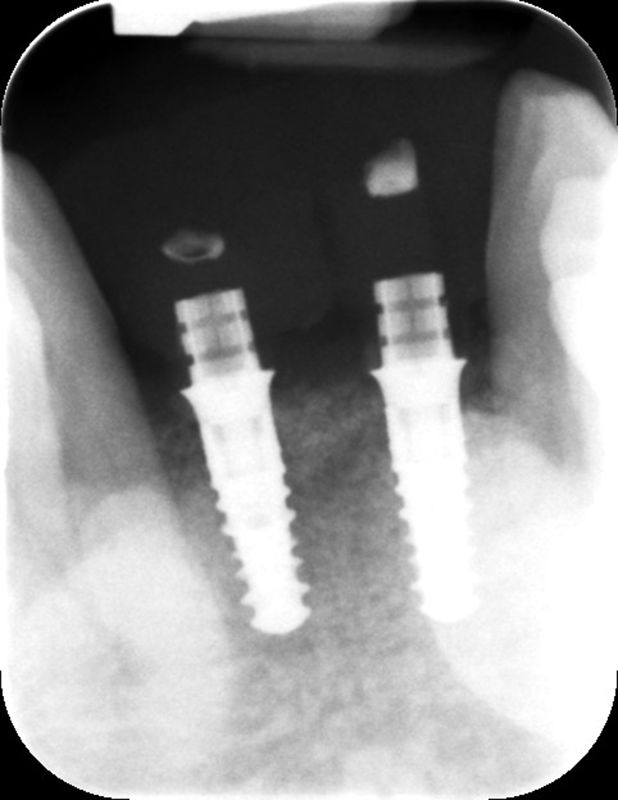
The radiographic evaluation showed severe bone loss with intrabony defects on the anterior mandible. Additionally, bilateral well-defined ovoid radiopacities were observed superimposed over the mandibular canine and premolars roots compatible with torus mandibularis (Fig. 2).