Initial situation
A healthy 72-year-old male, a non-smoker on no medication, came to our clinic as, a few months before, he began to notice gingival inflammation and bleeding in the area of his two central incisors. He visited a previous dentist who, following the clinical and radiographic assessments, concluded that the teeth presented vertical fractures and, therefore, needed to be extracted. The patient stated that he would like to restore them in the shortest possible time and maintain pleasing esthetics until the end of the treatment.
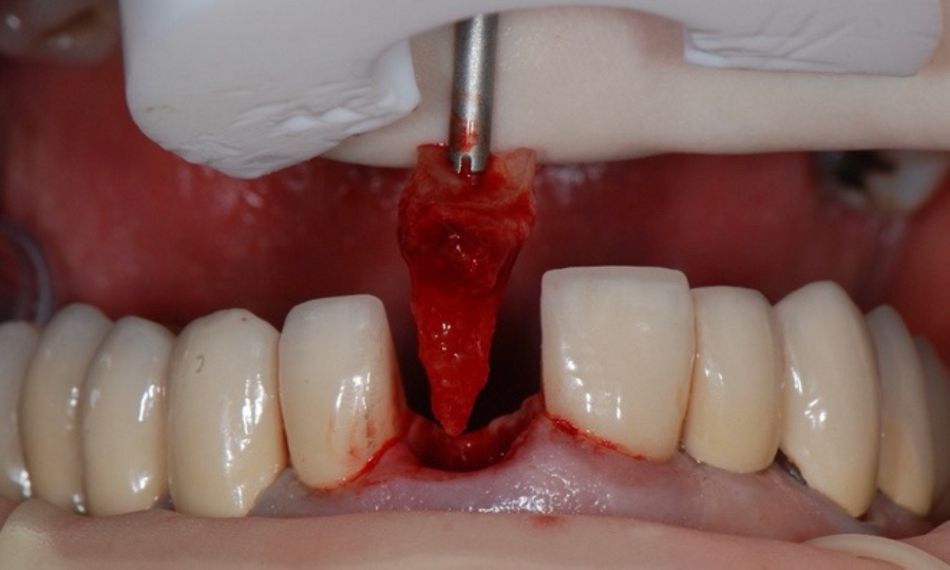
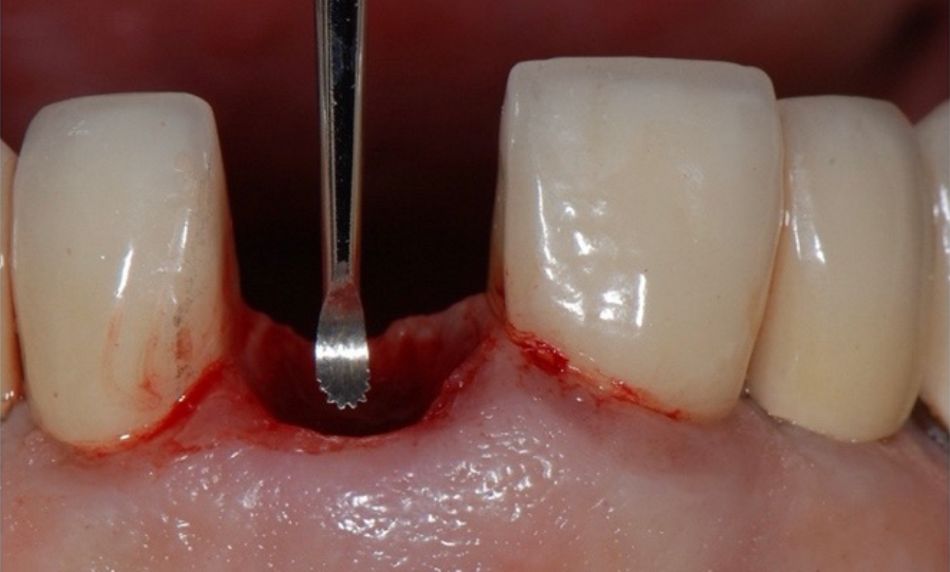
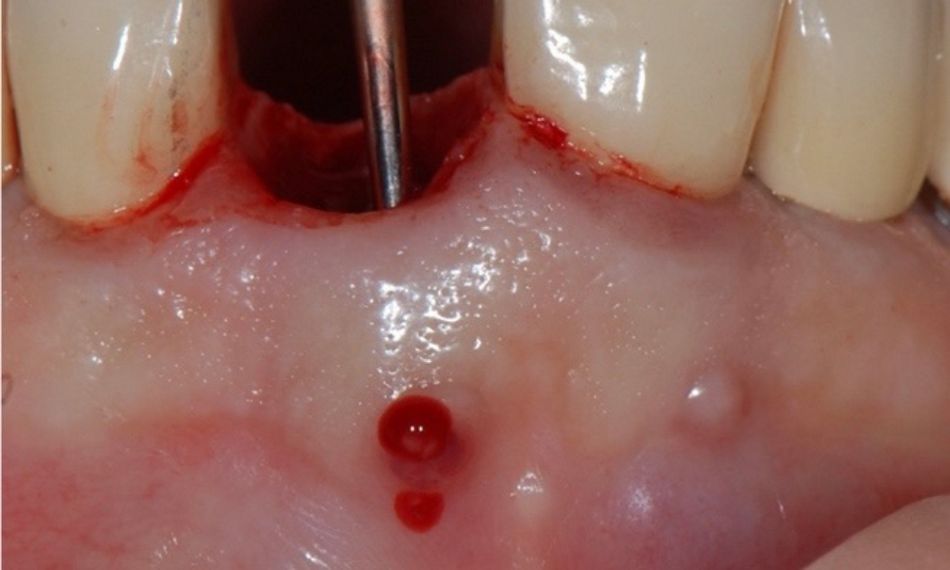
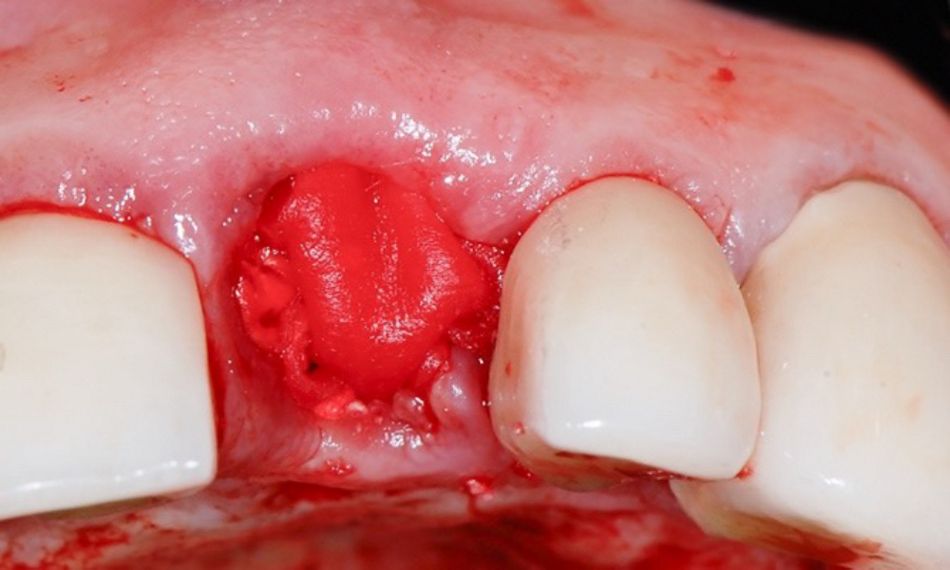
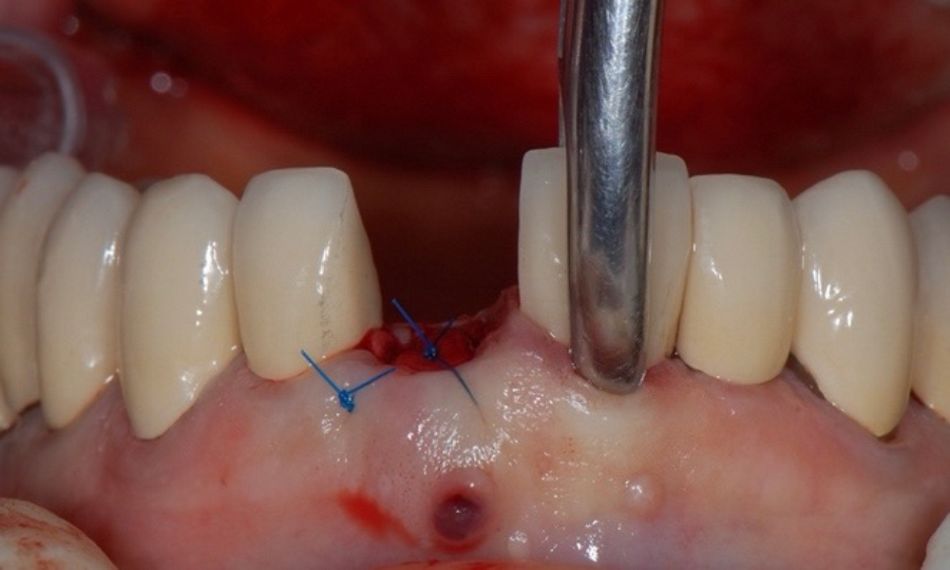
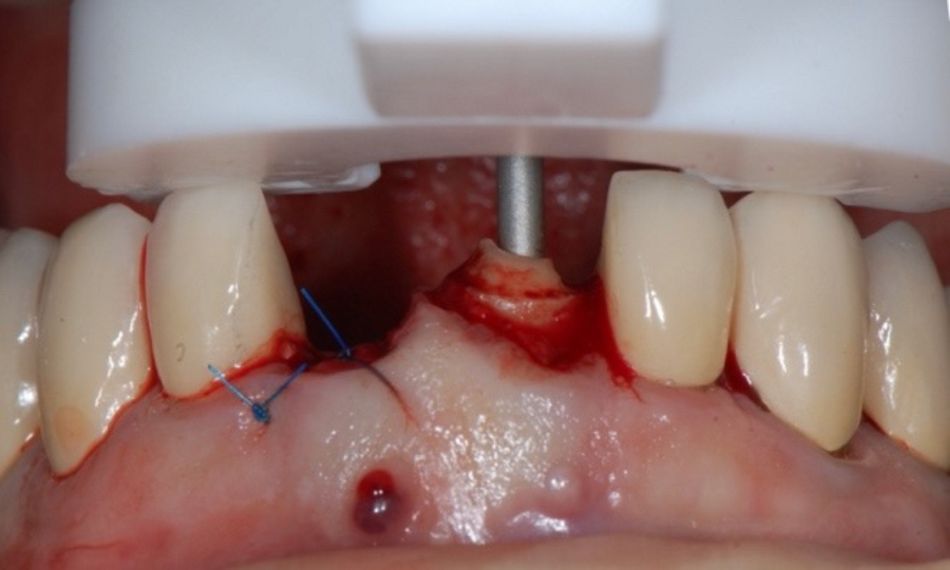
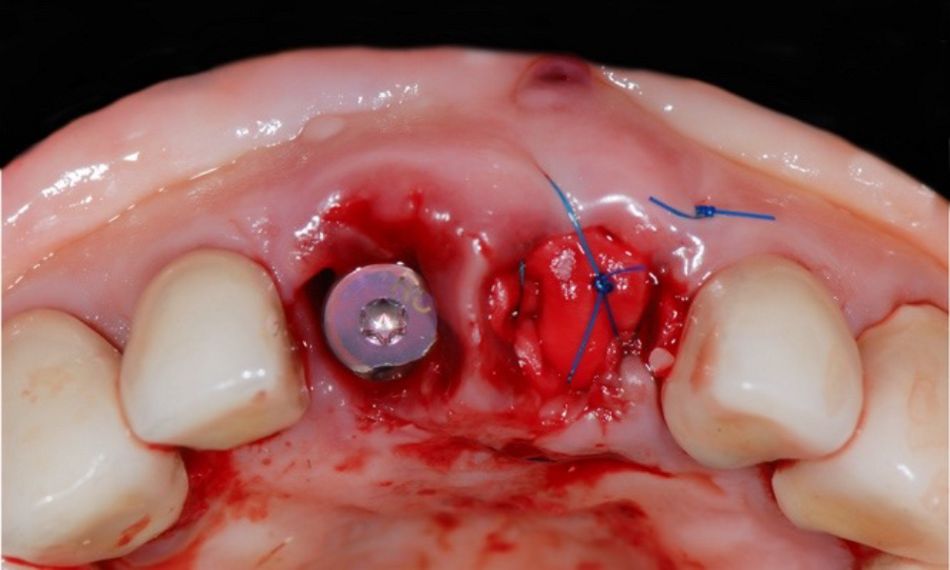
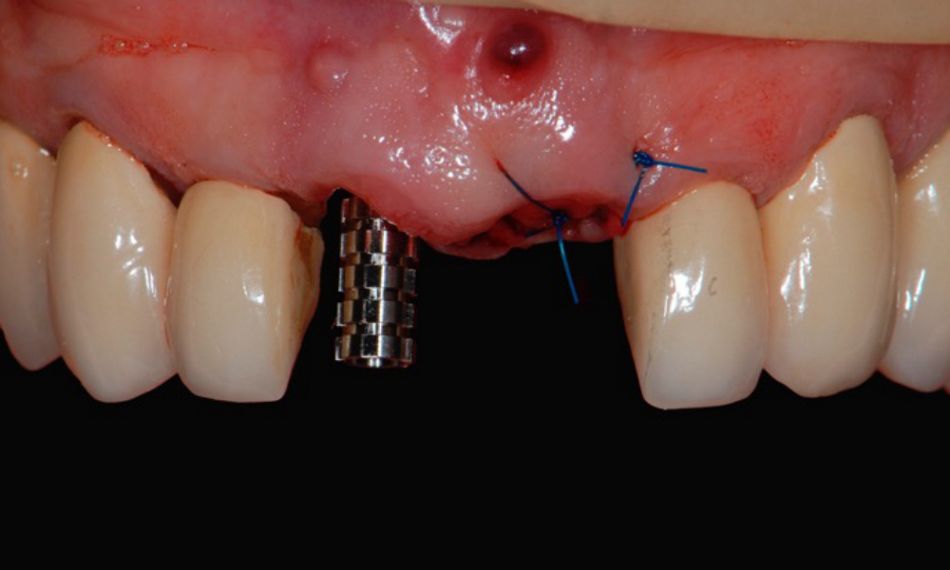
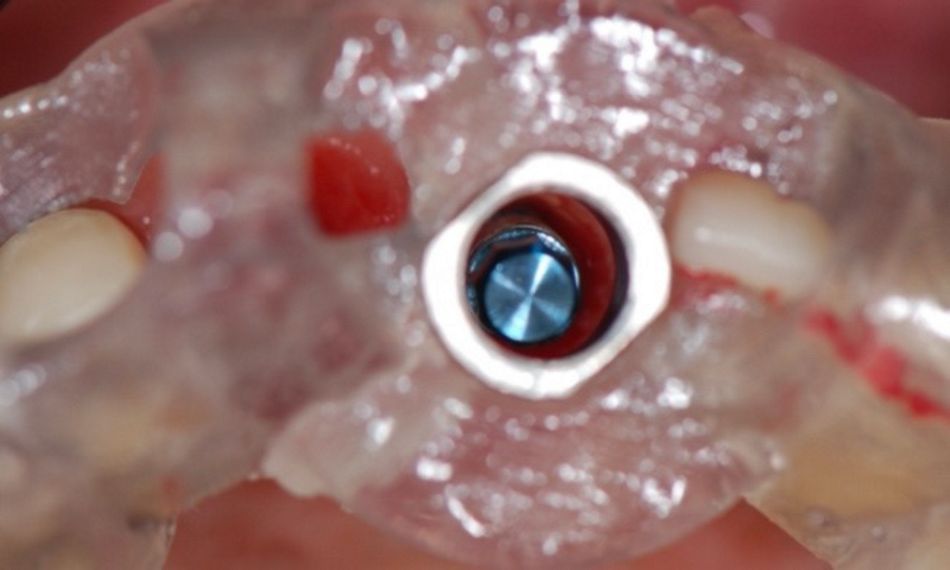
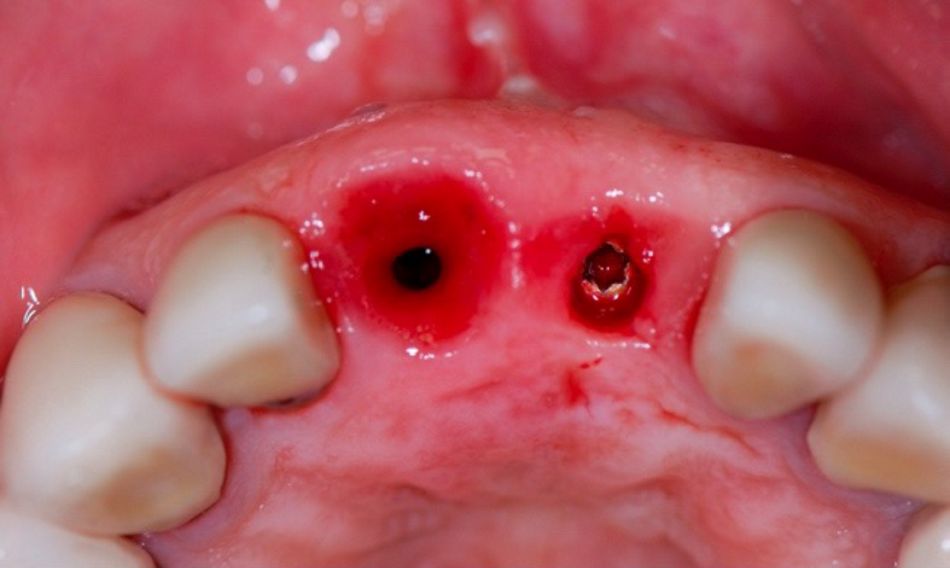
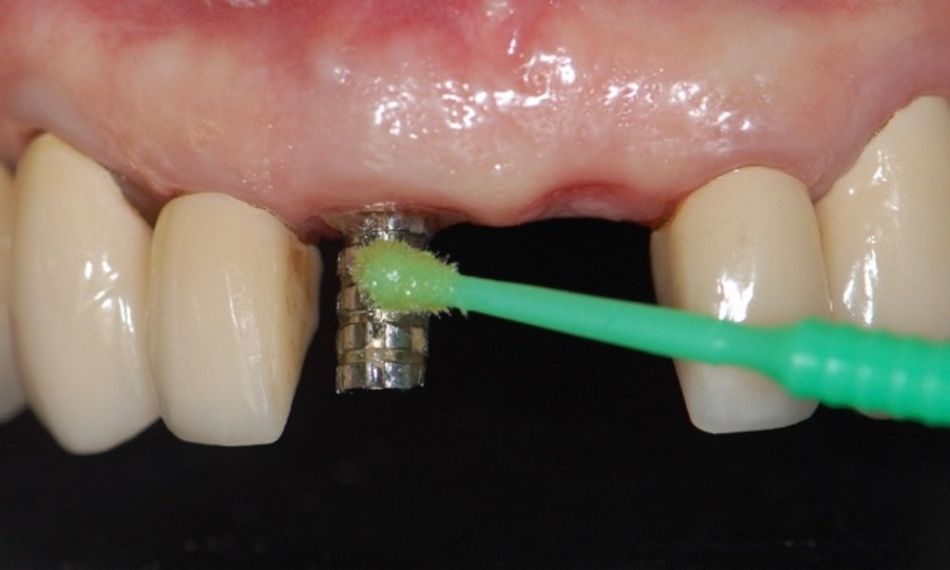
The extraoral examination revealed a low smile line (Fig. 1) The intraoral and CBCT examination showed hopeless teeth #11 and #21 with vertical root fractures. Moreover, tooth #21 also presented an active fistula and loss of the buccal bone plate (Figs. 2-4).
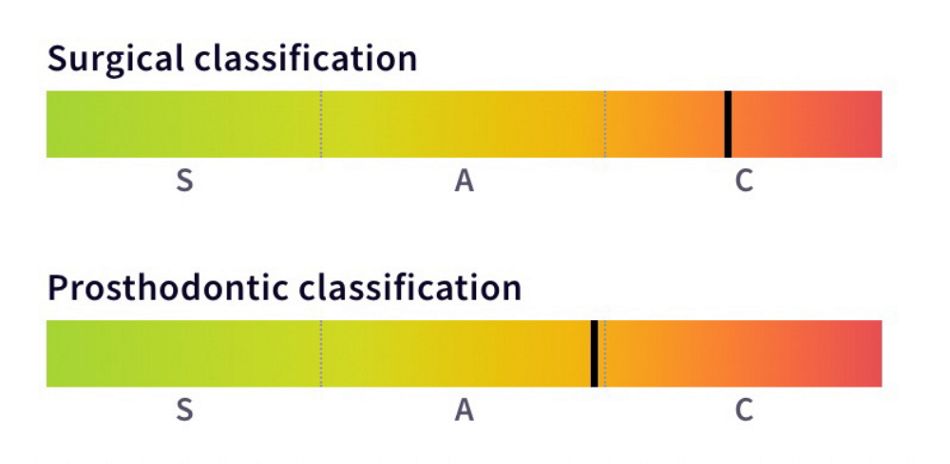
The SAC classification was used, since it provides an objective, evidence-based framework for assessing the potential difficulty, complexity, and risk of an implant-related treatment associated with individual implant dentistry cases in an easy-to-use process. It also helps clinicians with patient selection and treatment planning. The patient was classified as a complex surgical and advanced prosthodontic case (Fig. 4).
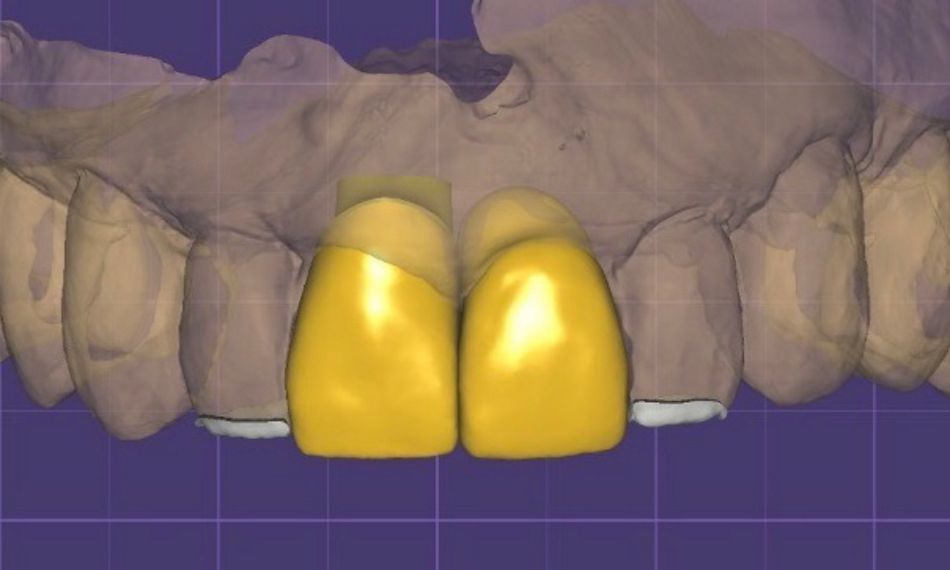
Treatment planning