Introduction
This clinical report describes the complete rehabilitation of a 69-year-old male patient using the Straumann® Pro Arch “All-on-6” approach with immediate loading of BLX implants. Fully digital planning in coDiagnostiX® allowed the fabrication of stackable surgical guides, enabling precise implant placement despite advanced alveolar resorption.
Immediate loading within 72 hours minimizes patient discomfort and accelerates the return to normal function. High primary stability - facilitated by the macro-geometry of BLX implants and their hydrophilic SLActive® surface - was pivotal. Short and narrow Roxolid® implants reduced the need for bone-grafting procedures, and screw-retained prostheses with palatal/occlusal screw channels enhanced retrievability and esthetics.
Initial situation
- Patient: Male, 69 years old, electrician
- Habits: Heavy smoker (>10 cigarettes ⁄ day)
- Dental history: Removable prostheses for >5 years, poor retention, incompetent fixed restorations, difficulty chewing, esthetic dissatisfaction.
- Clinical findings:
- Mobile abutment teeth supporting a failing maxillary bridge
- Inadequate porcelain-fused-to-metal (PFM) crowns in the mandible.
- Radiographic findings: CBCT showed pronounced vertical and horizontal bone resorption in both jaws.
- Chief complaint: Impaired mastication, missing posterior support, unstable dentures, unsatisfactory smile.
(Figs. 1-6)
Clinical examination revealed an unsatisfactory tooth-borne maxillary denture with mobile abutment teeth as well as inadequate PFM restorations in the mandible.
ITI SAC Classification of the Case
C – Complex
- Nearly edentulous maxilla and posterior mandible
- Pronounced vertical and horizontal ridge resorption
- Multiple hopeless roots to be extracted first
- Likely need for extensive bone grafting with or without bilateral sinus floor elevation
- Close proximity to the maxillary sinus and inferior alveolar canal
Restorative / Prosthetic
C – Complex
- Full-arch rehabilitation in the maxilla and extended posterior restoration in the mandible
- Compromised inter-arch space and opposing dentition
- Need for screw-retained, multi-unit splinted prosthesis (or full-arch bars / fixed bridges)
- Challenging path of insertion, emergence profile, and hygiene access
Overall SAC rating
C – Complex
Since both surgical and prosthetic aspects fall into the Complex category, the overall ITI SAC rating for this case is Complex.
Summary
Under the ITI SAC classification system, this situation qualifies as Complex (C) from both the surgical and restorative standpoints due to the extensive edentulism, severe ridge deficiencies, and the need for advanced grafting and full-arch implant-supported rehabilitation.
CBCT confirmed pronounced bone resorption in both the maxilla and mandible (Fig. 7).
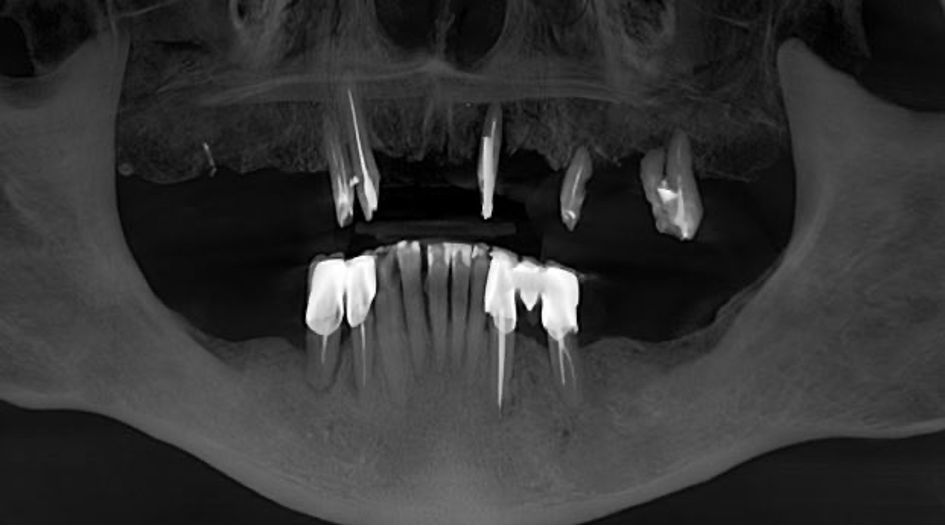
Fig. 7
Treatment planning
Treatment plan (digital workflow)
1. Diagnostics
- Intra-oral scans (STL) and CBCT (DICOM).
- Digital smile design and mock-up for patient approval.
2. Data fusion in coDiagnostiX®
- Prosthetically driven implant planning.
- Design of stackable tooth-borne surgical guides (positioner, bone-reduction guide, dual implant guides).
3. Maxilla
- Extraction of remaining hopeless teeth.
- Guided placement of six BLX implants:
- 16 – Ø5.5 × 8 mm
- 14 – Ø4.0 × 12 mm
- 12 – Ø3.5 × 10 mm
- 22 – Ø3.75 × 10 mm
- 24 – Ø3.5 × 12 mm
- 26 – Ø5.5 × 6 mm
- Immediate loading with a relined PMMA provisional 24 h post-op (torqued to ≥35 Ncm).
- Final monolithic zirconia bridge (6 months).
4. Mandible
- Atraumatic extraction of teeth 44, 45, 33, 35.
- Guided placement of four BLX implants:
- 34 – Ø4.0 × 10 mm
- 36 – Ø4.5 × 10 mm
- 44 – Ø4.5 × 14 mm
- 46 – Ø4.5 × 8 mm
- Soft-tissue conditioning, followed by zirconia bridges and ceramic veneers for anterior teeth.
Surgical procedure
coDiagnostiX® was used for treatment planning and designing a stackable surgical guide. (Figs. 8-17).
Under intravenous conscious sedation (propofol and nitrous oxide) and local infiltration (articaine 4 % and epinephrine 1:100,000), the stackable guide system was sequentially used. (Fig. 18)
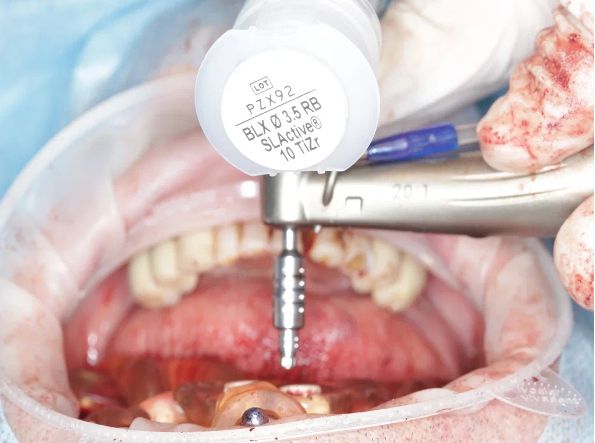
Fig. 18
A stackable surgical guide was fabricated, consisting of a tooth-borne positioner, a bone reduction guide, and two implant placement guides (one specifically for distal implants). (Figs. 19-24), (Video 1).
Surgical stage: Maxilla
Precisely seat the tooth-borne positioner with lateral pins (Fig. 25), (Video 2).
Remove failed teeth. Drill and place implants fully guided (except 2 mm for wide implants exceeding the sleeve diameter).

Fig. 25
Graft local defects with autogenous tuberosity blocks and particulate B2B, secured with fixation pins (Figs. 26,27)
Fully guided surgery was performed using the second guide. Implants were placed at sites
14 - Straumann BLX 4.0 x 12 mm
12 - Straumann BLX 3.5 x 10 mm
22 - Straumann BLX 3.75 x 10 mm
24 - Straumann BLX 3.5 x 12 mm
All implants were torqued to ≥35 Ncm (Figs. 28-30), (Video 3).
The third guide was fixed for the placement of short BLX implants (Ø 6.5 mm) at sites 16 and 26.
16 -Straumann BLX 5.5 x 8 mm
26 - Straumann BLX 5.5 x 6 mm
Short implants at 16, 26 were seated at 15 Ncm.
The implants beds were underprepared. Initial implant placement (first 1-2 mm) was performed without the guide, as the implants were wider than the 5 mm sleeves. The guide was then repositioned. Closure screws were placed (Figs. 31,32), (Video 4).
Bone profilers were used for coronal preparation to facilitate abutment placement (Fig. 33)

Fig. 33
At site 23, bone grafting was performed using a layer graft from the maxillary tuberosity, which was then secured with pins (Figs. 34,35), (Video 5).
Sutured with U-interrupted stitches to widen the band of keratinized mucosa.
Prosthetic procedure: Maxilla
Abutment-level scan bodies and the bone-reduction guide were scanned intraorally to cross-reference pre- and postoperative datasets.
Protective caps were mounted (Fig. 36), (Video 6).
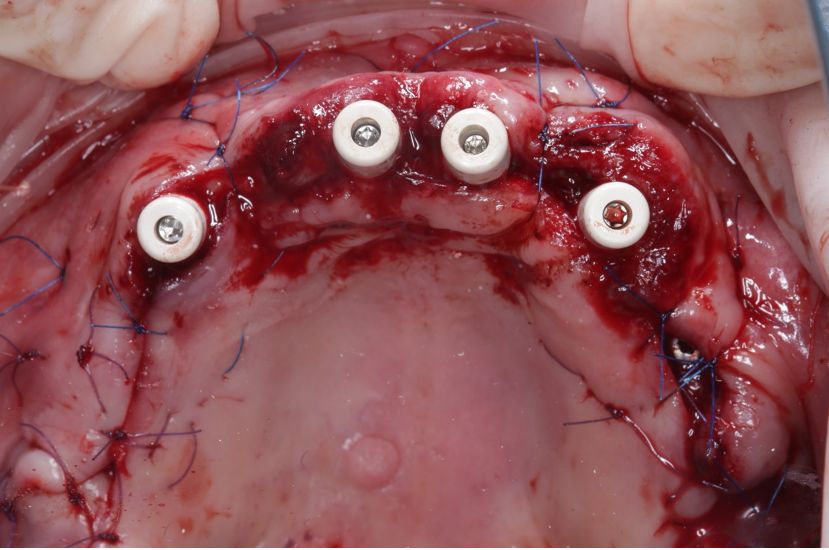
Fig. 36
A CAD/CAM PMMA bridge was milled, intraorally relined, and torqued to 15 Ncm 24h after surgery. (Figs. 37-42).
After 6 months, a try-in prototype verified occlusion, phonetics, and esthetics.
The definitive monolithic zirconia bridge was fabricated, Variobase® caps were bonded and torqued to 15 Ncm on the SRA abutments (Figs. 43-46)
Surgical procedure: Mandible
Guided implant placement and GBR performed under the same anesthetic protocol. All four implants achieved primary stability >35 Ncm. Wounds were closed with Monosyn® 5/0 sutures. The postoperative regimen included azithromycin 500 mg q.d. for 6 days, omeprazole 20 mg q.d. for 6 days, cold therapy, and chlorhexidine mouth rinses.
BLX implants:
- 34 Straumann® BLX SLActive® Roxolid® 4.0 х 10 mm.
- 36 Straumann® BLX SLActive® Roxolid® 4.5 х 10 mm.
- 44 Straumann® BLX SLActive® Roxolid® 4.5 х 14 mm.
- 46 Straumann® BLX SLActive® Roxolid® 4.5 х 8 mm.
(Figs. 47-51).
Prosthetic procedure: Mandible
After osseointegration, screw-retained zirconia bridges were delivered (Figs. 52-55).
The anterior segment received ceramic veneers for optimal smile esthetics (Figs. 56-66).
Treatment outcomes
The patient attends maintenance visits every six months. Clinical and radiographic evaluations show stable peri-implant bone levels and healthy peri-mucosal tissues 18 months post-loading. The patient reports high satisfaction with function, esthetics, and phonetics.
Conclusion
Digitally driven, immediately loaded full-arch rehabilitation with the Straumann® Pro Arch concept and BLX implants proved predictable even in severely resorbed arches. Key success factors included:
- Comprehensive digital planning integrating prosthetic requirements with anatomic limitations.
- High primary stability afforded by BLX macro-design and SLActive® surface, enabling immediate function.
- Stackable surgical guides that reduced chair time and ensured the accuracy of both bone reduction and implant placement.
- Minimally invasive grafting using short Roxolid® implants to avoid sinus augmentation and extensive bone grafts.
- Prosthetic passivity obtained by CAD/CAM monolithic zirconia frameworks and Variobase® interfaces.
Long-term success remains contingent on strict supportive care and reinforcement of smoking cessation.


