
- Immediate implant protocols: Dr. Algirdas Puišys specializes in immediate implant placement, particularly in complex cases like molar extractions and posterior mandibles. Techniques include atraumatic tooth extraction, 3D implant positioning, and use of individualized healing abutments alongside biomaterials such as maxgraft® and PRF for optimal integration and esthetics.
- Implant system innovation: Dr. Puišys actively integrates cutting-edge implant systems like the Straumann® BLX and TLX, emphasizing their biomechanical advantages for immediate loading and their role in maintaining bone levels. His approach leverages CAD/CAM technologies and patient-specific planning to ensure precise surgical and prosthetic outcomes.
- Soft and hard tissue management: Dr. Puišys employs advanced techniques for mucosal tissue thickening using botiss mucoderm®, a porcine-derived collagen matrix, to improve crestal bone stability around implants without the need for autografts. He combines this with guided bone regeneration and implant surface cleaning (GalvoSurge®) for treating peri-implantitis and enhancing implant longevity.
A leader in periodontology and implantology
Dr. Algirdas Puišys, D.D.S. Spec in periodontology and PhD, is a renowned Lithuanian dental specialist whose work in periodontology and implantology has earned him international acclaim. He currently leads the Vilnius Implantology Center (VIC Clinic), one of Lithuania’s most advanced dental facilities. With over 20,000 dental implants placed and more than 40 scientific publications to his name, Dr. Puišys has established himself as a pioneer in modern dental surgery. He is also the recipient of numerous prestigious awards, including the ITI’s André Schroeder Research Prize and multiple wins at the European Association for Osseointegration (EAO) Clinical Research Competition. He is also a member of the CoDE network, a group of independent dental centers all over the world that offer excellence in oral healthcare by providing the most advanced treatment procedures based on the best available literature and the latest technology.
Academic excellence and global influence
Dr. Puišys holds a PhD in Medical Sciences from Vilnius University, where he focused on the stability of crestal bone around implants. His academic journey began at Vilnius University and continued through Kaunas Medical University, where he specialized in periodontology. His expertise has led him to co-author the book “Zero Bone Loss Concepts” (by Prof. Tomas Linkevičius) and collaborate on research with leading institutions, including a partnership with the Harvard School of Dental Medicine. He is also a long-standing member and fellow of the International Team for Implantology (ITI), and serves on the board of the Baltic Osseointegration Academy.
Education, innovation, and mentorship
Dedicated to advancing dental education, Dr. Puišys offers both online and in-person training programs covering topics such as bone and soft tissue augmentation, immediate implant placement, and full-mouth rehabilitation. His mentorship initiatives provide personalized guidance to dental professionals through structured programs involving treatment planning and case discussions. As both a clinician and educator, Dr. Puišys bridges the gap between academic theory and clinical practice, shaping the future of implant dentistry not just in Lithuania, but around the world.
Academic education
- 2016: PhD from University of Vilnius, Lithuania (PhD)
- 2003 – 2006: Post-graduate studies in Periodontology at Kaunas Medical University (Dip perio)
- 1997 – 2002: General practice dentistry studies at University of Vilnius
Memberships
- EAO (member since 2008)
- Baltic Ossoeintegration Academy (Member of the Board)
- Lithuanian Periodontal Association (Member since 2010)
- Scientific partnership with Harvard School of Dental Medicine (since 2023)
Awards
- 2025: André Schroeder Research Prize (First place)
- 2023: EAO (European Association for Osseointegration) Clinical Research (First place)
- 2012: EAO (European Association for Osseointegration) Clinical Research (First place)
Dr. Puišys’ contributions to youTooth
This case addresses the challenge of crestal bone loss around dental implants associated with thin peri-implant mucosa. To mitigate this, he utilizes botiss mucoderm®, a porcine-derived collagen matrix, as an alternative to autogenous grafts for soft tissue thickening. The procedure involves placing a Straumann® Bone Level Implant, followed by the application of the rehydrated mucoderm® matrix over the implant site. This approach enhances mucosal thickness, promoting better crestal bone stability and esthetic outcomes. The case underscores the efficacy of mucoderm® in augmenting soft tissue, thereby contributing to the long-term success of dental implants.
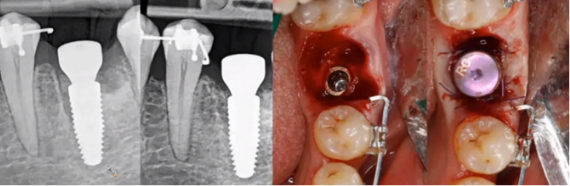
This case report shows the successful treatment of peri-implantitis using the GalvoSurge® Dental Implant Cleaning System combined with guided bone regeneration (GBR). A 66-year-old patient presented with peri-implantitis around implant #37, characterized by bleeding on probing, increased probing depths, and circumferential bone loss. Initial non-surgical interventions included prosthesis removal, installation of healing abutments, mechanical debridement, and antimicrobial irrigation. Subsequently, surgical treatment involved electrolytic cleaning with GalvoSurge®, application of a Straumann® Membrane Flex, and grafting with autogenous bone chips mixed with botiss maxgraft® granules. Over a two-year follow-up, the patient exhibited stable peri-implant conditions with no signs of inflammation or bone loss, underscoring the efficacy of this combined approach in managing peri-implantitis.
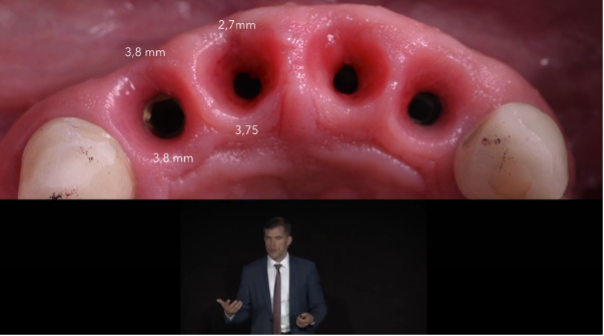
In this EAO 2019 Corporate Forum lecture, Dr. Puišys shares insights from over 15 years of experience in immediate implant placement, focusing on achieving predictable esthetic outcomes in the anterior region. He highlights the challenges of early techniques and the turning point brought by clinical trials and updated evidence. Central to his approach is the “four-millimeter rule,” emphasizing the need for sufficient buccal soft tissue thickness to maintain crestal bone stability. Through careful implant positioning, use of small-diameter implants, and tailored grafting strategies, Dr. Puišys demonstrates how to minimize complications and ensure long-term success. He also discusses the evolving role of grafting materials, including xenografts and dermal substitutes, and underscores the importance of individualized treatment planning based on anatomical conditions.
(With Dr. Viktorija Auzbikavičiūtė). The immediate placement of a Straumann® BLX implant in the posterior mandible of a 40-year-old patient is shown. The patient presented with secondary caries and subgingival destruction in tooth #36, rendering it non-restorable. Following atraumatic extraction and preservation of the interradicular septum, a 5.5 x 8 mm BLX implant was placed. The surgical site was augmented with allogenic bone graft (maxgraft®) and platelet-rich fibrin (PRF) to support healing. After four months, the implant demonstrated stable soft tissue integration, and a final zirconia ceramic crown was successfully installed, resulting in satisfactory functional and esthetic outcomes.
The use of botiss mucoderm®, a porcine-derived collagen matrix, to increase mucosal tissue thickness around Straumann® Bone Level Implants. The goal was to improve crestal bone stability and esthetic outcomes, particularly in cases with thin peri-implant mucosa. The procedure involved placing the implant and covering it with rehydrated mucoderm® to promote soft tissue thickening without the need for harvesting autogenous grafts. Results showed enhanced mucosal volume and stable bone levels, supporting the matrix's effectiveness in improving long-term implant success.
The strategies to enhance crestal bone stability following immediate implant placement in molar regions are explored and the complexities of achieving optimal outcomes in such procedures, particularly due to the anatomical challenges presented by molar extraction sites are explored. The importance of several key factors in ensuring successful implant integration and bone preservation is highlighted. These include performing atraumatic tooth extractions to minimize tissue damage, precise three-dimensional positioning of the implant to align with the patient's anatomy, and the use of individualized healing abutments tailored to the specific surgical site. Additionally, the role of implant design in influencing bone stability and the benefits of incorporating CAD/CAM technology and bone augmentation techniques to support the implant site is discussed. The webinar provides valuable insights into the complexities of immediate implant placement in molar areas and underscored the necessity of a comprehensive approach that considers surgical precision, prosthetic planning, and biological factors to achieve long-term success.

The Straumann® TLX Implant System combines the neck design of the iconic Straumann® Tissue Level (TL) implant with the innovative endosteal design of the Straumann® BLX Implant System, perfected for immediate protocols. In this episode of 60 SECONDS, Dr. Algirdas Puisys shares his personal experience about the benefits it brings to his clinic.

On-demand webinar by Algirdas Puisys. Missed the live surgery webinar? Watch it on-demand and experience a fully commented, step-by-step surgery. Get expert insights, practical tips, and in-depth commentary directly from the clinician.
