Immediate implant placement with Straumann TLC™ implants in maxillary esthetic zone
Introduction
Implant therapy in the maxillary aesthetic zone presents significant biological and prosthetic challenges, particularly when immediate placement protocols are adopted. Maintaining peri-implant soft tissue stability, emergence profile control, and long-term aesthetic outcomes remains critical. Tissue Level implants have not traditionally been used in aesthetic sites; however, their hybrid design may offer advantages in soft tissue preservation by maintaining a stable transmucosal interface. Evidence supporting their use in immediate placement protocols in the aesthetic zone remains limited.
Initial situation
A 73-year-old female patient was referred for assessment of failing maxillary anterior restorations. Her chief complaint was compromised aesthetics and function due to fractured fixed dental prostheses. A three-unit bridge spanning #21, 22, 23 had failed following fracture of the abutment teeth at gingival level (Figs. 1a-c). A second bridge replacing #11, 12, 13 exhibited ceramic fracture and questionable abutment prognosis (Figs. 2a-c). The patient had been provided with a removable acrylic partial denture as an interim solution.
Figs. 1 a-c: Preoperative clinical situation.
Figs. 2 a-c: Preoperative radiographic situation of the maxillary anterior teeth.
The patient was a non-smoker with a history of well-controlled hypertension and hypothyroidism. Periodontal assessment revealed stable health with no active inflammation. Remaining teeth were moderately restored without significant pathology. The gingival phenotype was thick, and the maxillary central incisors displayed a length-to-width ratio exceeding 80%, resulting in short, wide clinical crowns.
Radiographic evaluation, including CBCT (Figs. 3 a–c), showed Class IV root positioning of the maxillary anterior teeth with buccal bone thickness < 1 mm. No periapical pathology was present. Based on clinical and radiographic findings, the prognosis for the maxillary anterior abutment teeth was poor.
Figs. 3a-c: Preoperative CBCT #13, 11, 23.
Diagnoses
- Acquired tooth loss
- Failed maxillary anterior fixed dental prostheses (#11, 12, 13 - #21, 22, 23)
- Root fractures of #21, 22, 23
- Failing maxillary bridge (#11, 12, 13 with ceramic fracture of #11)
Treatment planning
The patient expressed a strong preference for a fixed, implant-supported solution prioritizing aesthetics and function. A prosthetically driven treatment plan was formulated.
Surgical Plan: Immediate implant placement with early loading (Type 1B protocol).
Restorative Plan: A screw-retained provisional PMMA bridge for soft tissue conditioning followed by a screw-retained definitive monolithic zirconia bridge supported by titanium base abutments.
Implant planning
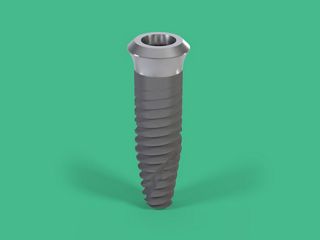
Virtual implant planning was performed using coDiagnostiX implant planning software. Intra-oral scan data (.stl) were merged with CBCT (.dicom) files. The four maxillary teeth were virtually extracted, (Figs. 4 a-b) and three Straumann TLC™ SP Ø 4.5mm RT, SLActive® 12mm, Roxolid® implants were planned in sites #13, 11 and 23 (Figs. 5a-h).
To improve crown proportions, implants were positioned approximately 4 mm apical to the existing gingival margins, allowing for 1-2mm increase in clinical crown length. Osteotomies were planned palatally, maintaining a minimum distance of 2mm from the buccal bone crest. A fully guided surgical approach and a screw-retained prosthetic design were selected.
“RT” type (collar diameter 4.8mm) was selected for the implants to allow for optimal emergence of the missing teeth.
Figs. 4 a, b.
Fig. 5 a-c: Preoperative CBCT with implant plan.
Fig. 5 d-e: Preoperative CBCT plan – IO Scan and with the existing denture.
Fig. 5 f-h: Preoperative CBCT with implant plan – #13, 11, 23.
This maxillary aesthetic zone case highlights the application of tissue‑level hybrid design implants, featuring a polished transmucosal collar and rough body design, for use in immediate placement protocols.
Surgical procedure
Following local anaesthesia, a minimally traumatic extraction of the failing teeth was performed using root sectioning and elevation. Socket integrity was confirmed, and thorough debridement was carried out (Fig. 6).
Fig. 6: Teeth extracted.
A fully guided, flapless osteotomy preparation was undertaken, and the implants (Straumann TLC™ SP Ø 4.5mm RT, SLActive® 12mm, Roxolid® implants) were placed through the surgical guide (Figs. 7a, b) achieving primary stability exceeding 80 Ncm.
Figs. 7 a, b: Fully guided flapless implant placement surgery.
Healing abutments (3 mm height) were connected immediately. The peri-implant gaps were grafted with deproteinised bovine bone mineral with collagen to support soft tissue contours up to the level of the healing abutments (Fig. 8). The #21 socket was additionally grafted and stabilised with a cross suture using 6-0 monofilament nylon.
Fig. 8: 3mm tall healing abutments with DBBM Collagen in buccal bone gap and socket #21.
Post-operative management included ibuprofen 400 mg three times daily for five days, amoxicillin 500 mg three times daily for five days, and chlorhexidine 0.2% mouth rinse for 60 seconds, five times daily. Healing was uneventful, with early evidence of coronal soft tissue migration observed at one-week review (Fig. 9).
Fig. 9: 1w post placement healing.
Prosthetic procedure
Four weeks post-surgery, prosthetic treatment commenced (Figs. 10 a,b).
Figs. 10 a,b: occlusal and facial view showing 4w post placement healing abutments. Excellent height of soft tissue is maintained during early phase of healing.
An intra-oral digital impression was obtained, and a screw-retained provisional PMMA bridge was fabricated and inserted to initiate soft tissue conditioning (Figs. 11 a,b). The provisional restoration was progressively modified to create ovate pontic contours and guide peri-implant mucosal shaping.
Figs. 11 a,b: Provisional milled PMMA bridge inserted.
A key advantage of the tissue level implant design is the ability to remove and replace provisional restorations without disrupting the peri-implant soft tissue seal, which remains stable at the machined collar interface.
After 4 months follow-up visit, optimal soft tissue architecture was achieved (Figs. 12 a-d) and a definitive intra-oral scan was performed.
Figs. 12 a-d: After the modification of the provisional bridge and prior to the definitive IO Scan.
A 3D-printed resin verification jig was fabricated to confirm the accuracy of the digital impressions prior to final prosthesis design (Figs. 13a-c).
Figs. 12 a-d: After the modification of the provisional bridge and prior to the definitive IO Scan.
The definitive restoration consisted of a screw-retained monolithic zirconia bridge supported by titanium base abutments (Straumann Variobase®) (Figs. 14 a,b).
Figs. 14 a,b: Definitive monolithic zirconia on titanium base abutments.
Excellent aesthetics were achieved with monolithic zirconia and modern staining techniques (Figs. 15 a-d). The alveolar root convexity in implants is well maintained (Fig. 16).
Figs. 15 a: Definitive prosthesis – facial view.
Figs. 15 b-d: Definitive prosthesis – facial views.
Fig. 16: Definitive prosthesis – occlusal view.
Baseline periapical radiographs (Figs. 17a-c) obtained at prosthesis delivery demonstrated stable marginal bone levels.
Figs. 17 a-c: Radiographs taken at the time of fit of definitive prosthesis.
Follow up
At one-year review, favourable soft tissue contours and aesthetic outcomes were observed (Figs. 18 a-d). A discrepancy in the mucosal zenith of #23 compared with the contralateral canine was identified (Fig. 18 a) and attributed to an over-contoured prosthetic emergence profile, which could have been corrected at the time of bridge fitting. It had been accepted in the belief that the mucosa might migrate coronally in the fullness of time.
Figs. 18 a-d: 1 year outcome.
To correct it, the bridge was removed. The black highlighted area shows the convex over-contoured emergence that would have pushed the mucosa apically (Figs. 19 a, b).
Figs. 19 a, b: The black highlighted area shows over-contoured emergence pushing the mucosal zenith more apically than desired.
The submucosal contour was modified chairside to create a more concave emergence profile (Fig. 20), and the bridge was returned to the patient (Fig. 21).
Figs. 20: Submucosal emergence modified and made more concave.
Fig. 21: Modified bridge replaced.
One week following reinsertion, coronal migration of the mucosal zenith was observed (Fig. 22), resulting in improved symmetry. This correction remained stable at the two-year follow-up (Fig 23). Radiographic assessment at two years confirmed continued marginal bone stability around all implants.
Fig. 23: A two-year review shows continuing stability of clinical and radiographic parameters.
Figs. 24 a-c: Radiographs taken at 2y follow up.
Treatment outcomes
This case demonstrates that excellent pink and white aesthetic outcomes can be achieved using Straumann TLC™ implants in immediate placement protocols within the maxillary aesthetic zone. Stable peri-implant soft tissue architecture and marginal bone levels were maintained over two years without the need for adjunctive connective tissue grafting (Figs. 13 a-e).
The key take-aways
- Tissue-level implants can be effectively utilised in immediate placement protocols within the maxillary aesthetic zone.
- Prosthetically driven digital planning is critical for precise control of emergence profiles and mucosal zeniths.
- Long-term stability of peri-implant soft tissue and marginal bone can be achieved in Tissue-level implants without adjunctive soft tissue grafting.