Initial situation
A non-smoker 25-year-old female patient with no remarkable medical issues presented to our office for a consultation regarding food impaction in the right lower jaw. Her chief complaint was food getting stuck between her teeth, giving her bad breath despite her efforts to maintain good oral hygiene. She also stated that the tooth concerned had changed color over time and that she was very dissatisfied with its esthetic appearance.
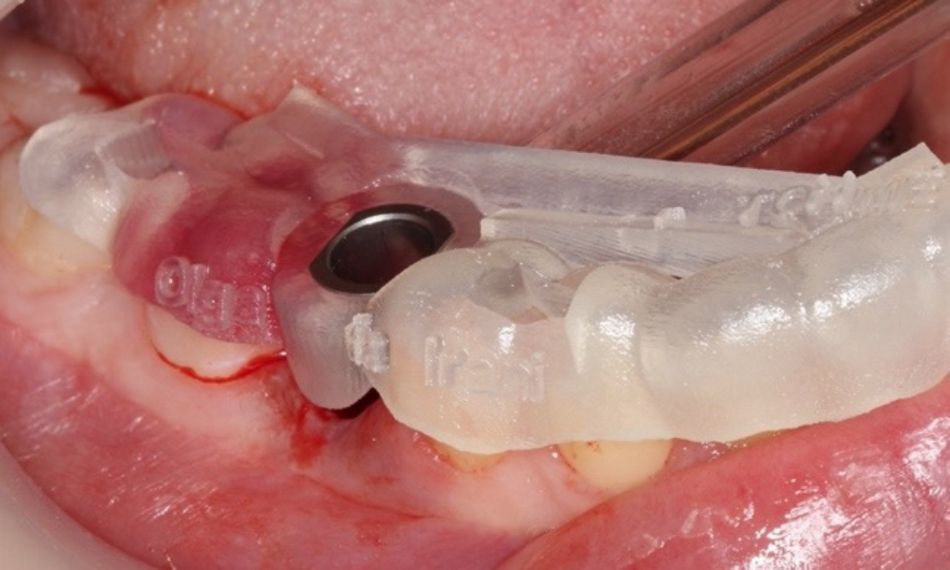
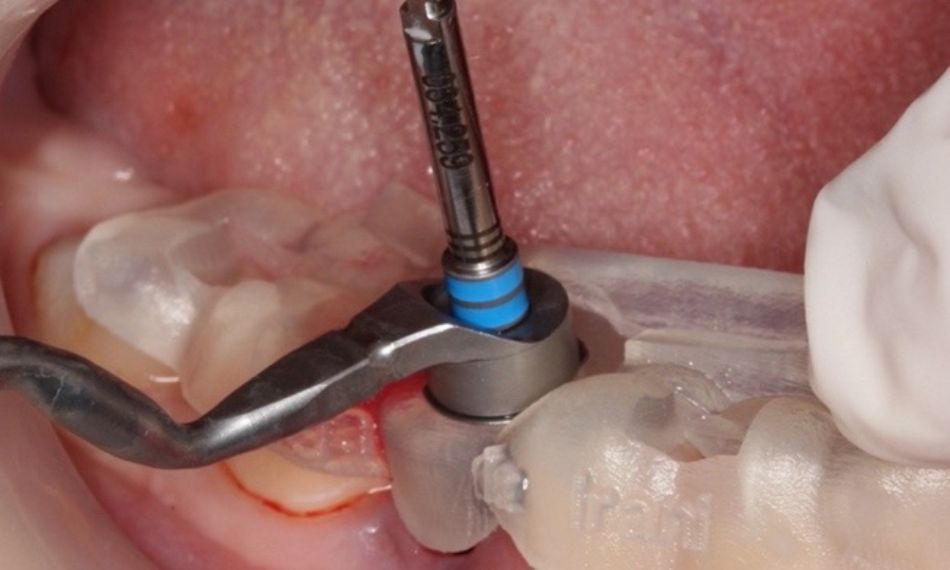
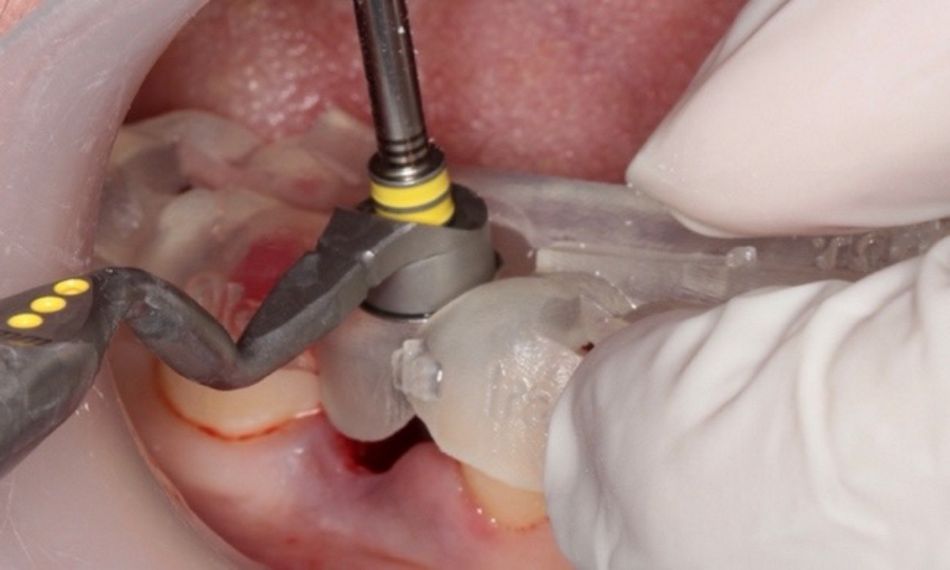
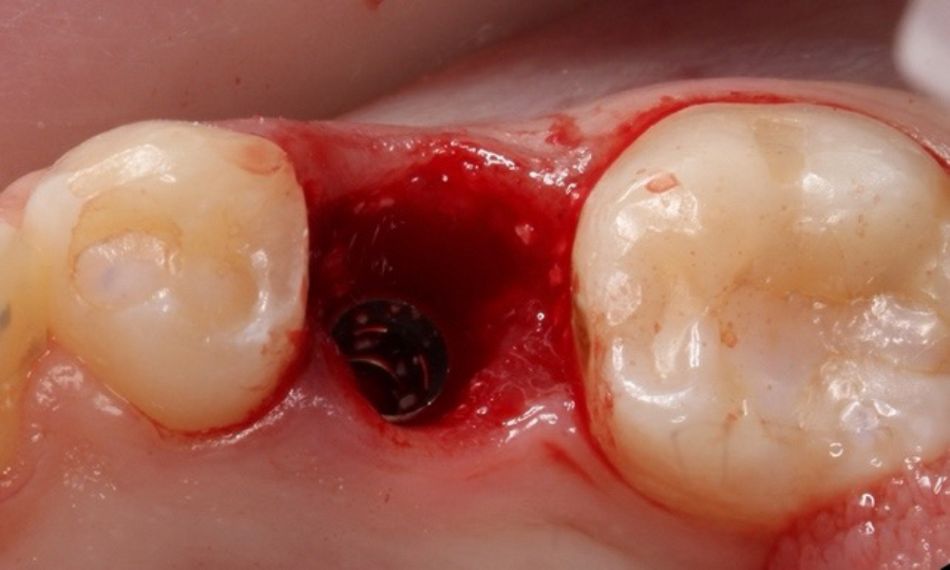
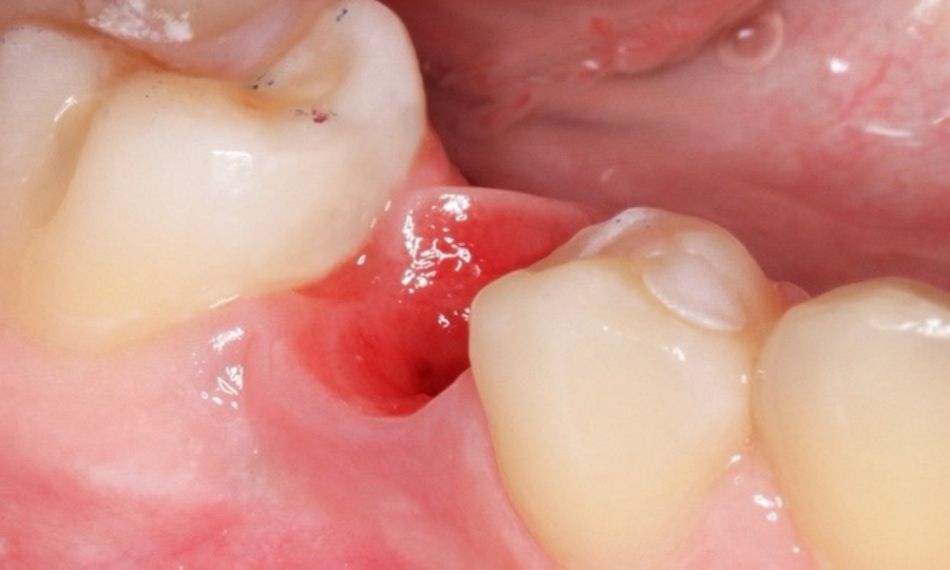
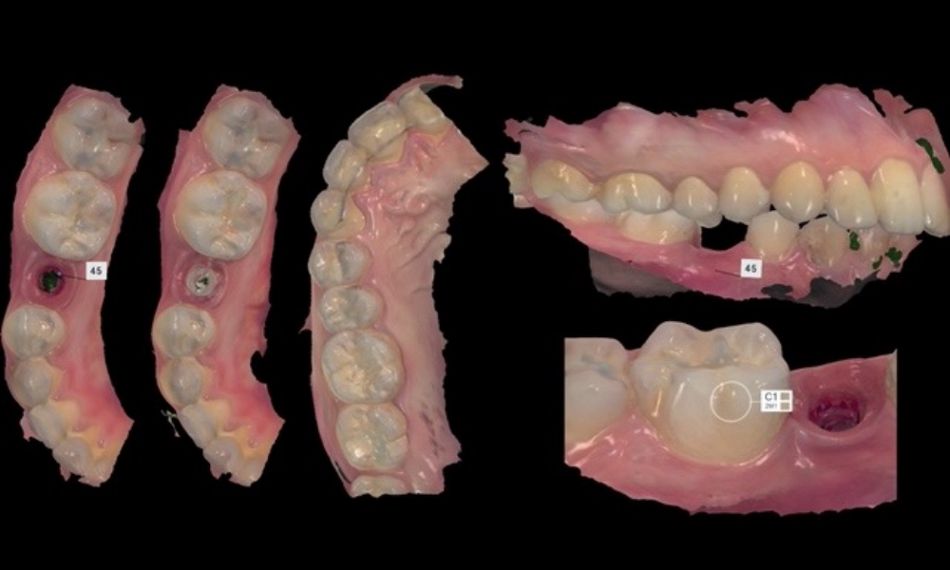
The intraoral examination revealed tooth #45 with a failing distal occlusal provisional restoration and a greyish color compared to the adjacent teeth. Furthermore, the gingival tissues around the tooth were inflamed and presented BoP+ in all locations.
Given these clinical characteristics, a vitality test was carried out. The cold test was negative, but the percussion test was positive (Figs. 1,2).
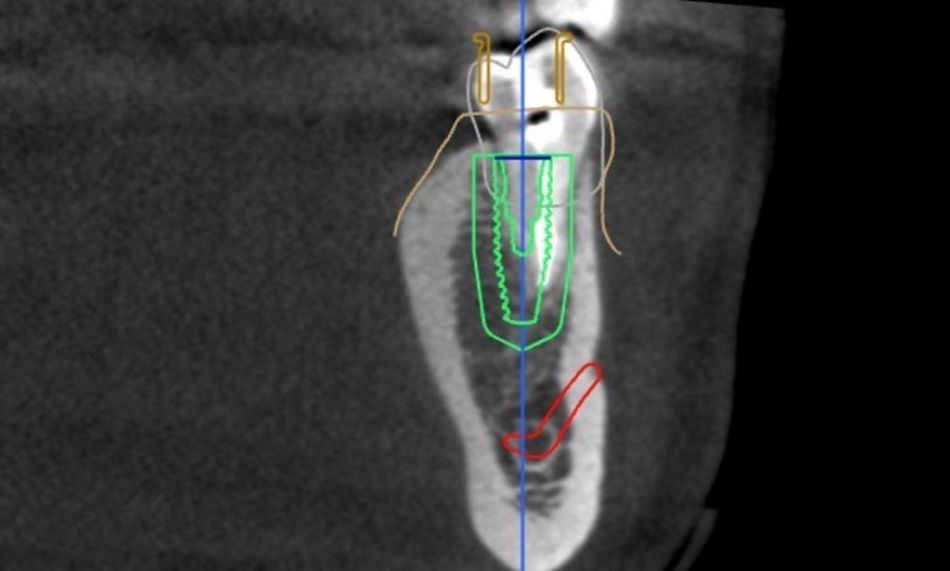
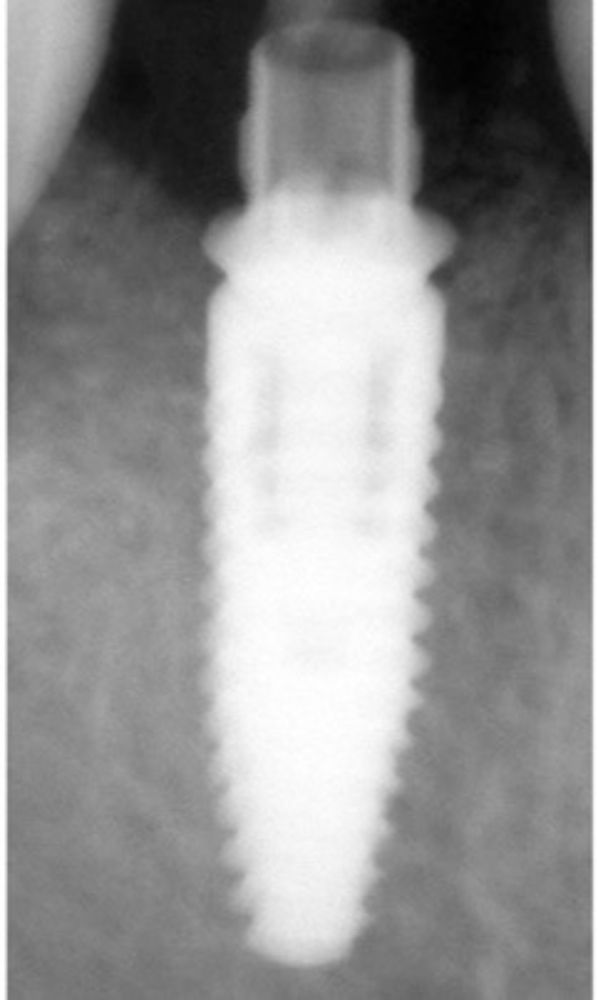
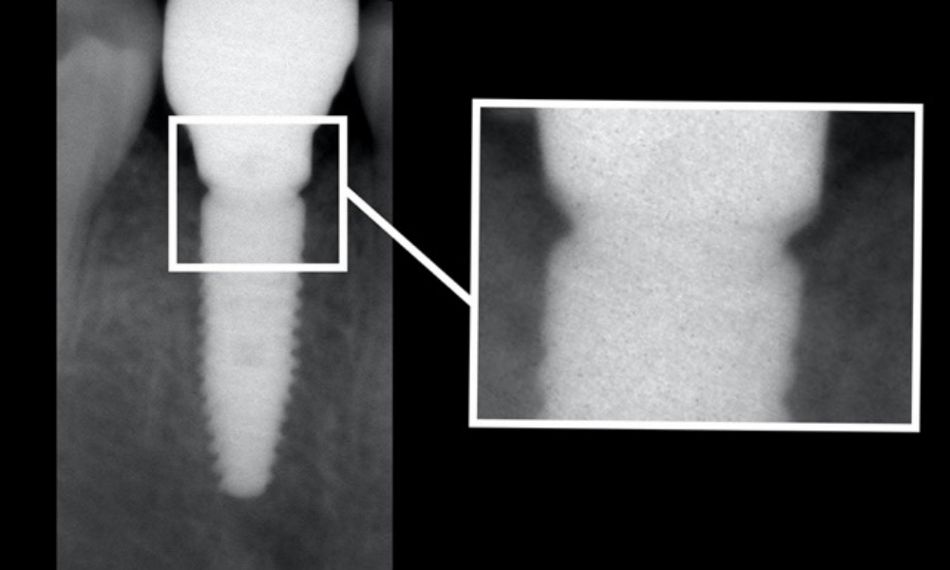
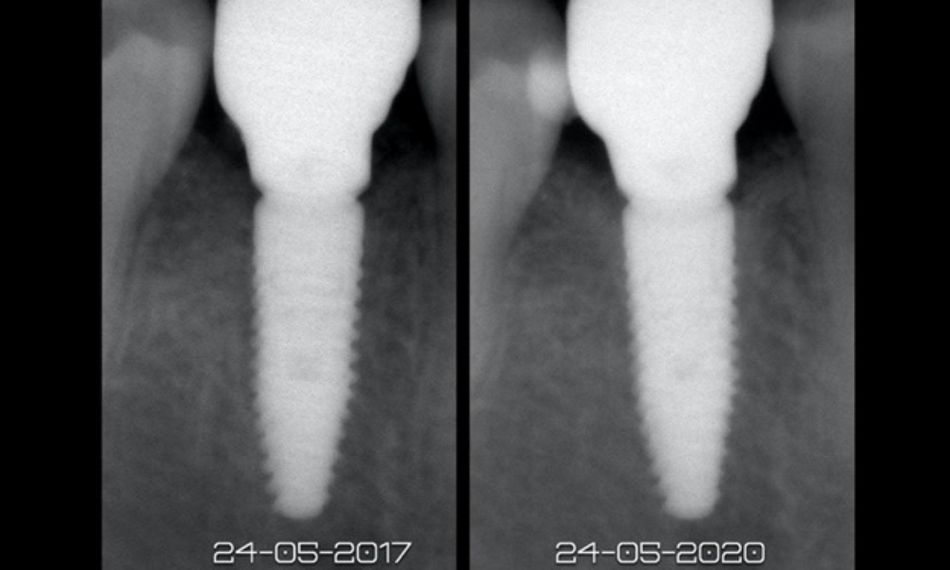
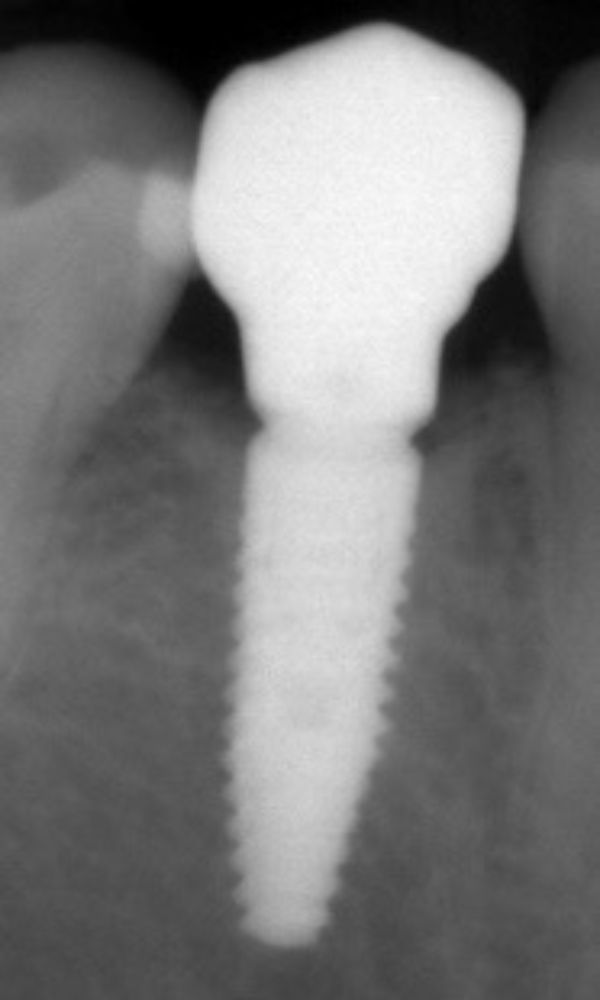
The radiographic examination showed a crown fracture of tooth 45 extending to the root (Fig. 3).
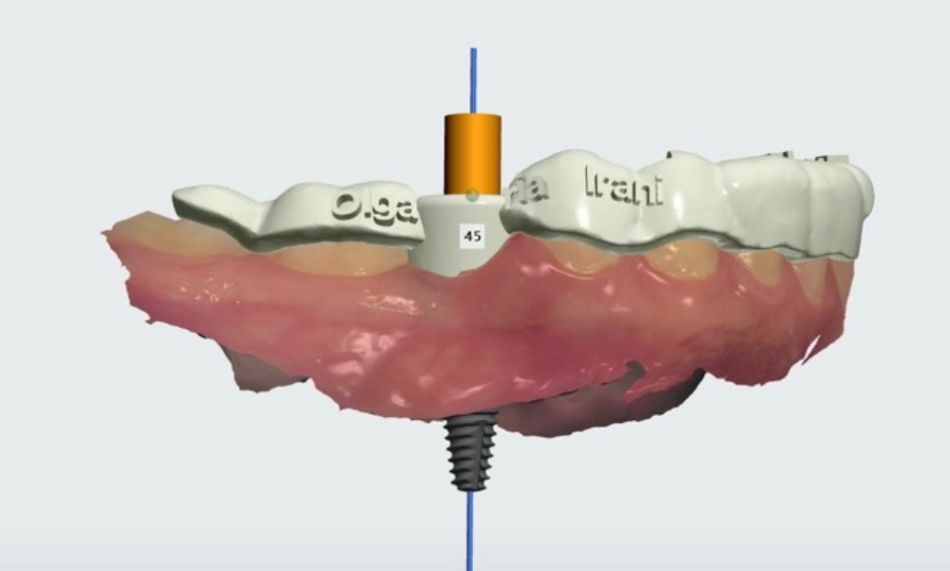
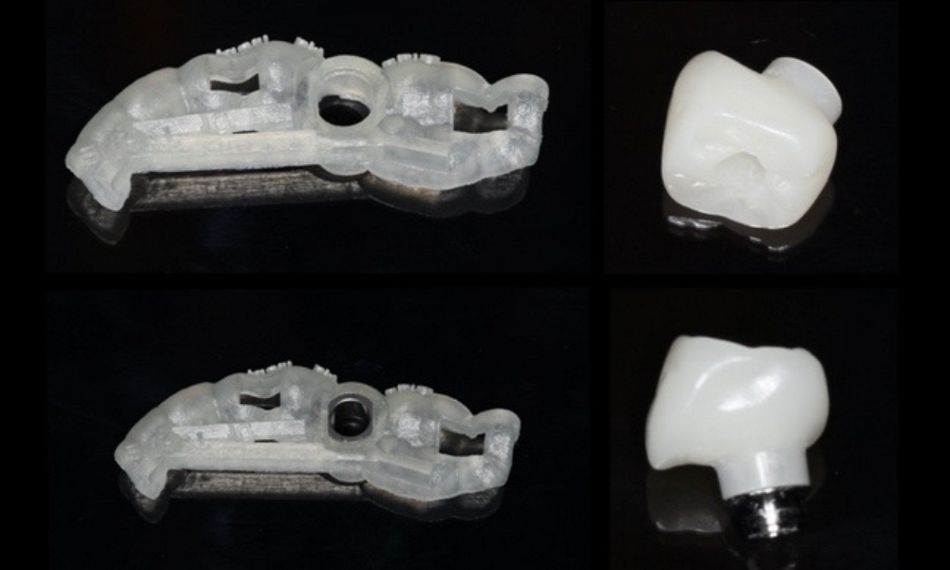
Treatment planning