This case report describes the predictable coverage of multiple adjacent maxillary gingival recessions using the modified coronally advanced flap (MCAF) technique and modified coronally advanced tunnel technique (MCAT) in conjunction with an acellular porcine-derived collagen matrix (mucoderm®) combined with enamel matrix derivative (Straumann® Emdogain®). The author states: "In my opinion, this case can be viewed as satisfactory both for the patient and the operator, effectively demonstrating the benefits of the combination of mucoderm® and Emdogain® as regards time and pain."
Initial situation
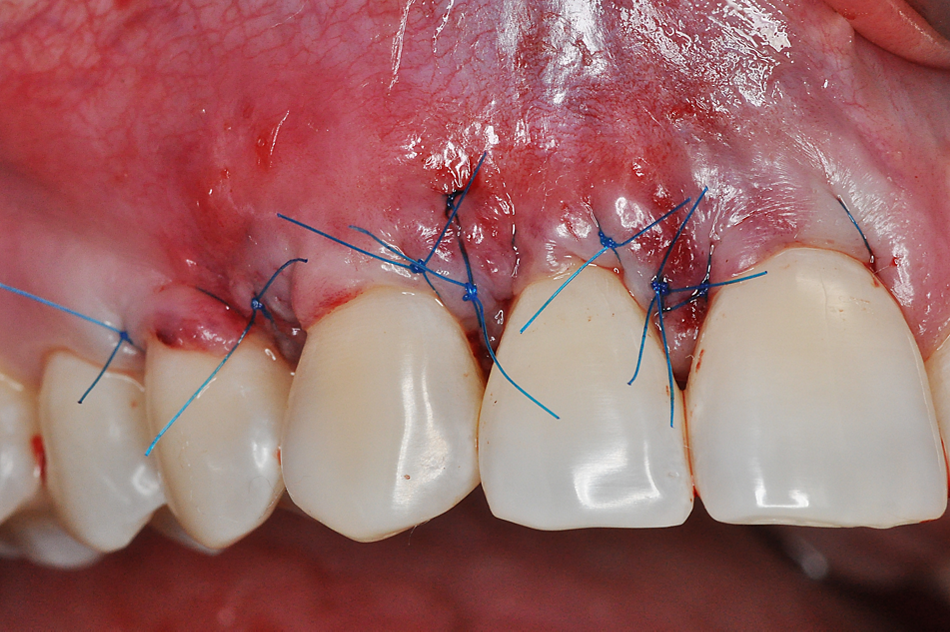
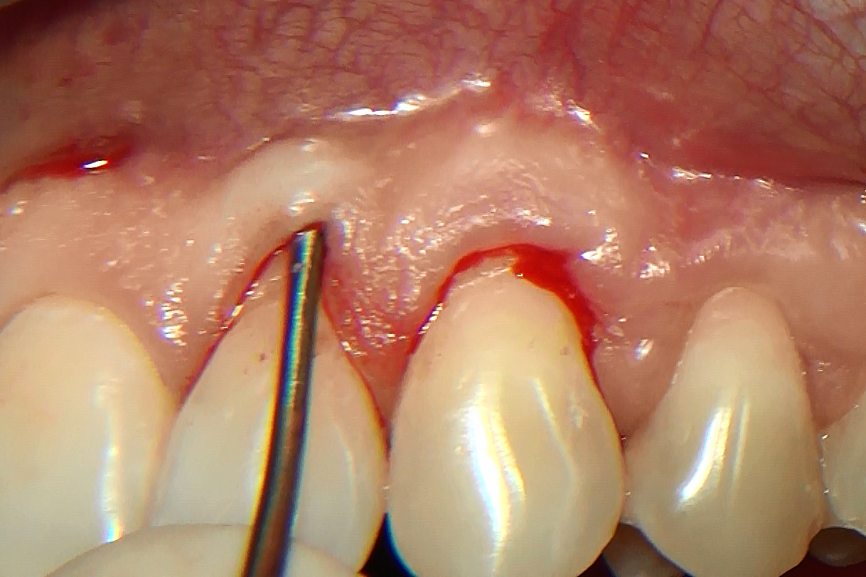
A 30-year old female patient in good general health conditions presented with Miller Class I gingival recessions in the upper jaw affecting the teeth #12, #13 and #14 and teeth #22, #23 and #24 (Figs. 1-3), and was referred to our office by an orthodontist colleague (Enikő Szívos, DMD, orthodontist). The patient sought a minimally invasive approach to improve ther aesthetic appearance and to facilitate brushing.
Treatment planning
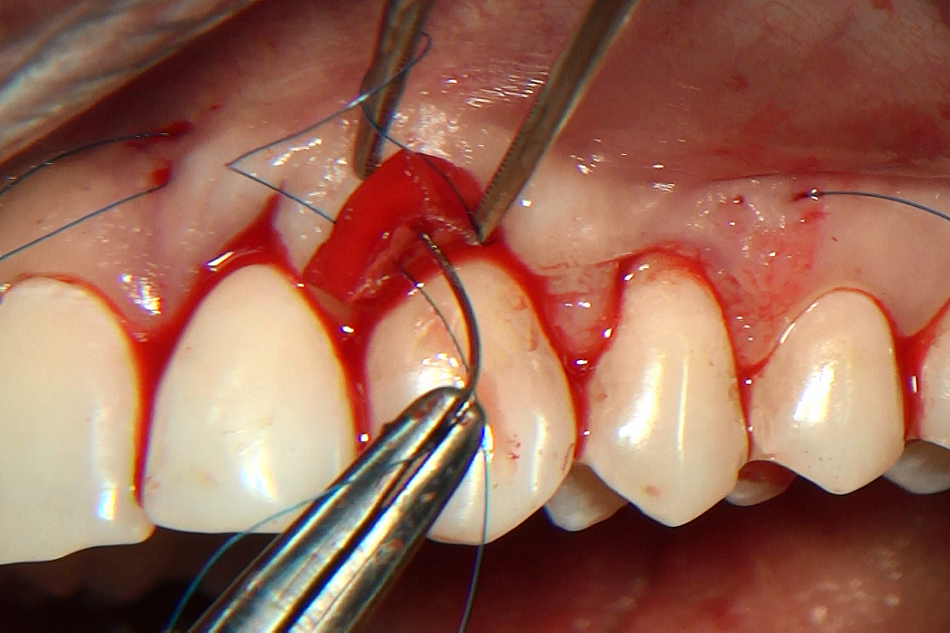
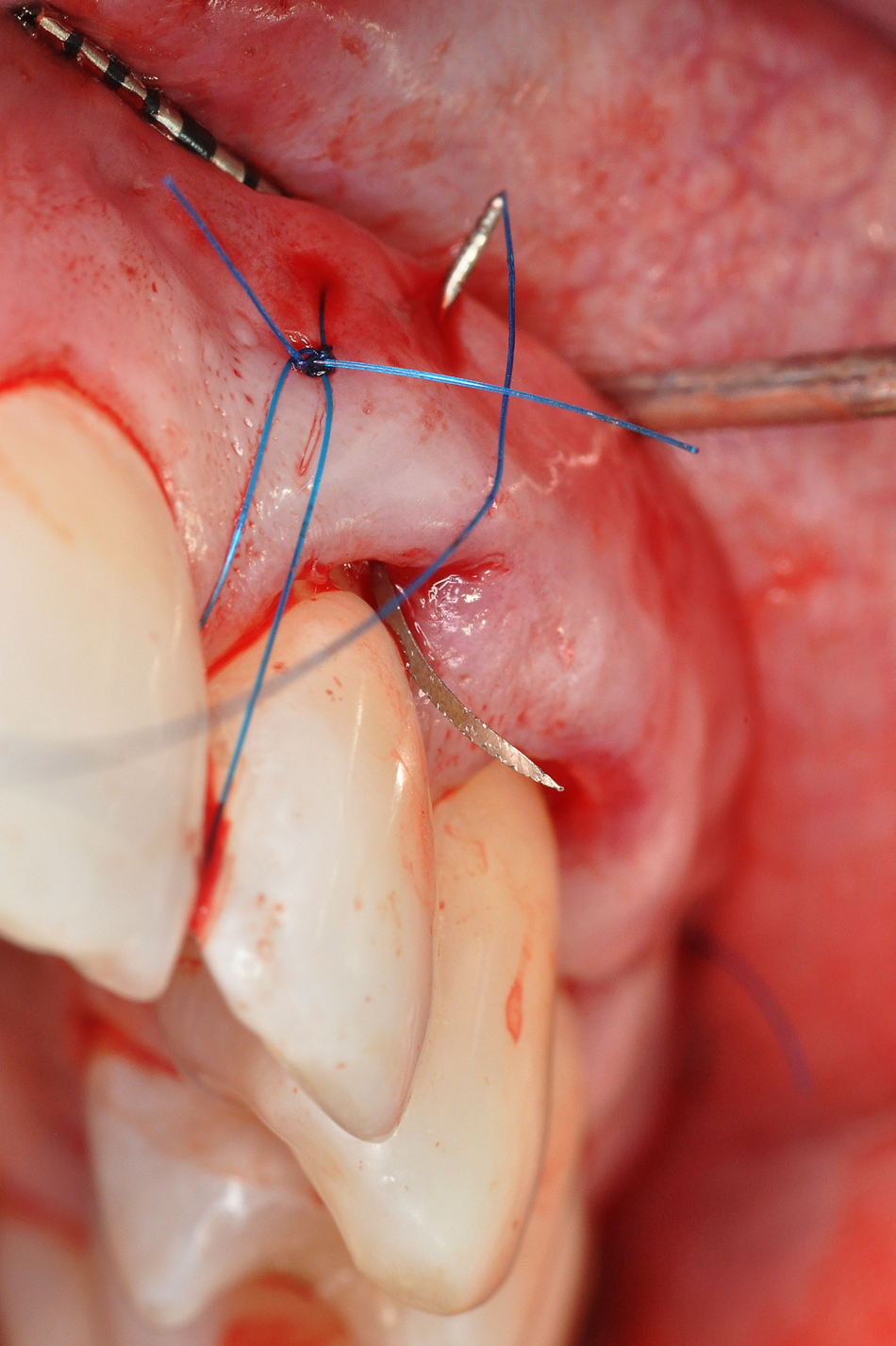
To achieve a satisfactory aesthetic result with, at the same time, minimal traumatization of the soft tissues, a minimally invasive approach was chosen to cover the exposed roots. Professional oral hygiene was implemented prior to the scheduling of regenerative therapy with mucoderm® and Emdogain®. We decided to perform the coverage before the orthodontic therapy, and we also decided to use different surgical procedures and biomaterials depending on the local clinical situation.
As we wanted to improve the quality of attachment, we decided to use PrefGel®/Emdogain®. In some places the thickness of keratinized gingiva was not adequate. To thicken the gingival tissues and produce more keratinized gingiva, we planned to apply mucoderm®.
Surgical procedure