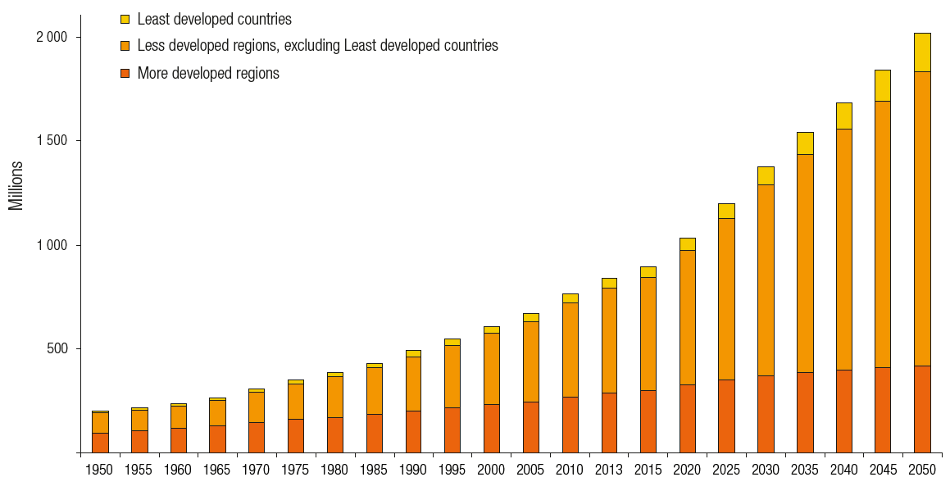
Current demographic prognoses show that the proportion of elderly (population of 60 and above) will increase strongly in all developed and underdeveloped countries worldwide by 2050 (Fig. 1). This naturally results in an increasing stress on the global health system. One of the stressors that dentists can focus on is dental health, specifically regarding implants (Table 1). Millions of dental implants made from titanium are inserted annually worldwide. They are especially used for the elderly, in order to rebuild the functional and aesthetic purposes of teeth after partial or total loss. Implant therapy has therefore developed into a procedure which allows very demanding dentures in faster and cheaper ways.
Implantological developments
With the development of titanium implants from 1965 to 1990 there was a wave of excitement and hope among both dental practitioners and patients in need. This technology was new, fascinating, and incredibly profitable. Unfortunately, in the excitement to apply this new technology the much needed research on the still unknown side effects began to diminish and the focus quickly turned to treatment diversification and profit.
Fast forward 52 years to present day and we now see that implants can lead to some form of bodily reaction presented as infection. These infections are described as mucositis and peri-implantitis. It can be observed that the implant disease starts with mucositis and progresses towards a status of peri-implantitis and can even progress as far as to result in complete implant loss.
Recently it has been shown, that these problems of inflammation increase especially with titanium implants that have been inserted over a longer period of time.1 The majority of respondent US implantologists reported that the prevalence of peri-implant mucositis and peri-implantitis in their practices is as high as 25 per cent. They estimated that there is an even higher proportion within the general US population.
Regarding this study and the fact that there is no proven therapy for this detrimental process, when consulting the published success rates it becomes obvious that more often than would be expected it results in implant loss. According to relevant literature, we can take 10 per cent as a minimum value for implant losses over the years.
Even though aetiology is multifactorial and could not be clarified acceptably, there is a lot of evidence pointing towards titanium intolerance playing a decisive role in patient condition.8 As studies were able to show, zirconium dioxide reduces that risk because ceramic, unlike titanium particles, do not provoke significant secretion of messenger substances for osteolytic processes.

Table 1. Overview of inserted implants by nation. (Source: Süddeutsche Zeitung [Uhlmann 2016], Press office DGI, KZBV, dental industry)
Could ceramic implants be the (new) “next best thing”?
After a rough beginning, with frequent material breakages and very limited numbers of suppliers, ceramic implants are becoming increasingly more present in the field of dental solutions. More and more, informed consumers are demanding treatment options which are holistic and thus considering the body as a whole. To date, there is very little data of known implant disease regarding ceramic implants—not a bad start but will this data change? And if so, when, how, and by how much?
The now realised success with two-piece and specifically the new bone-level ceramic implants will lead to much greater use of ceramic implants, as a wide range of indications can be covered, that were until now reserved to titanium implants.
Conclusion
In summary there could be a change of focus turning from peri-implant disease to implant disease. Bringing more focus to the implant disease in general medicine will give us a chance to investigate this phenomenon more seriously. This is a task for all participants in the field of implantology because knowledge about implant disease could lead to widespread uncertainty in our patients and we need to be well informed in order to properly advise them.