Patient Nº1
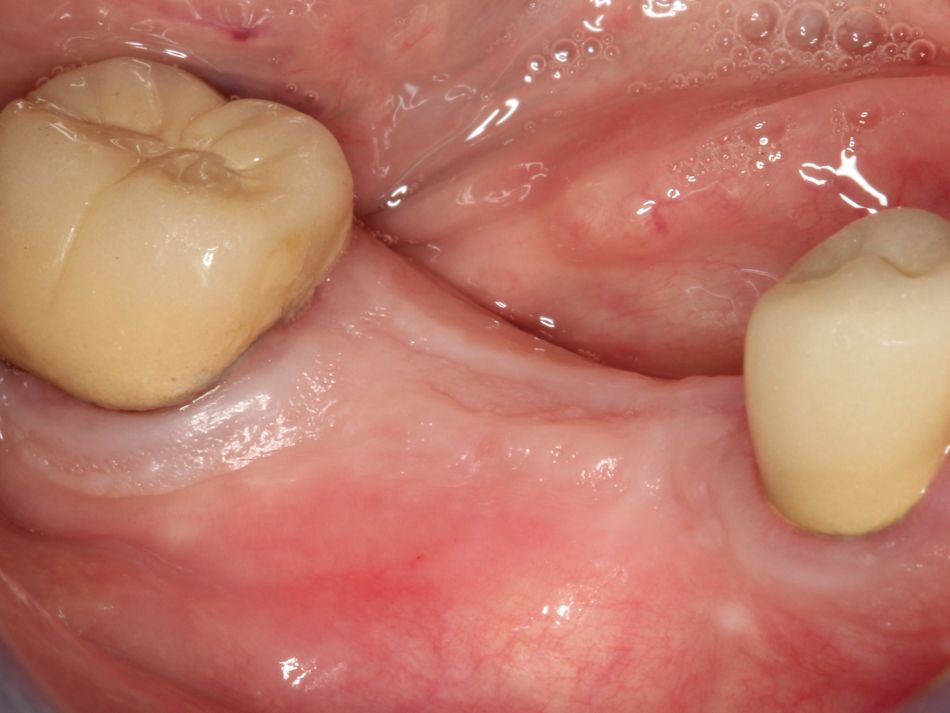
Initial Situation
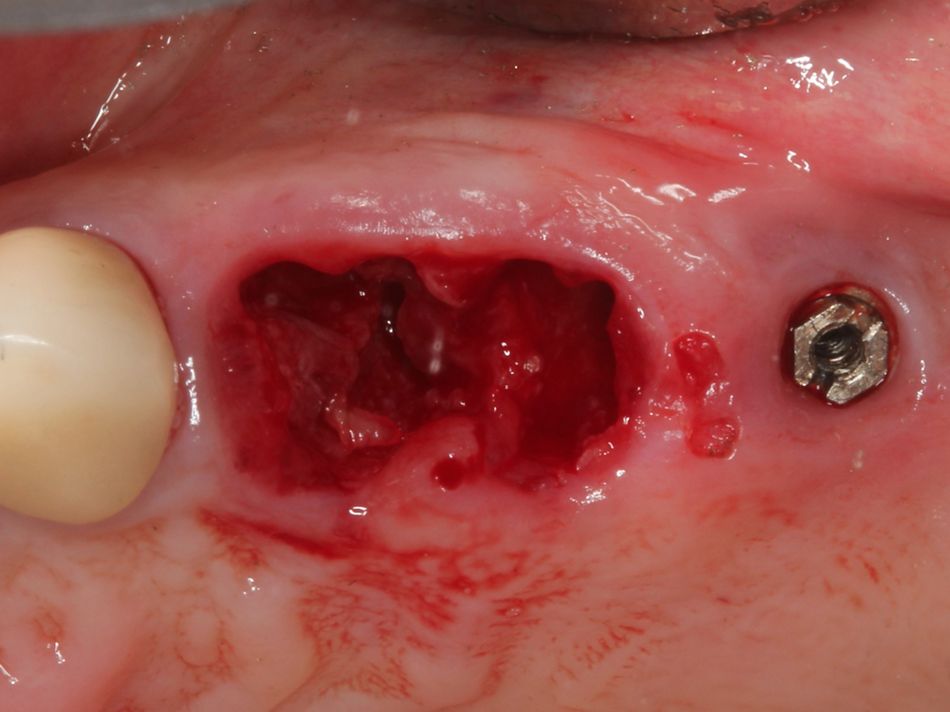
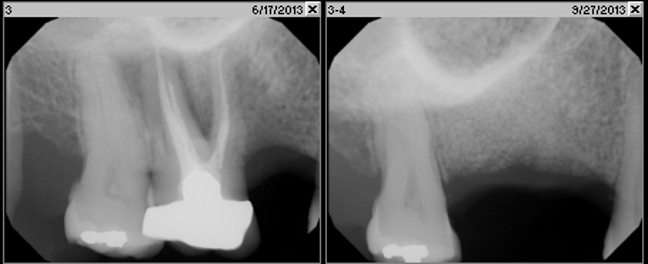
A 68-year-old female patient with unremarkable medical history presented in March 2013 with a failing maxillary implant prosthesis in the upper left posterior sextant. She reports that the upper left posterior sextant had become symptomatic over the last six months and believes that the TPS press fit implant was placed in the late 1990’s. Pressure to biting and swelling have convinced her to seek treatment although she has been advised of a deteriorating situation in the past.
Treatment planning
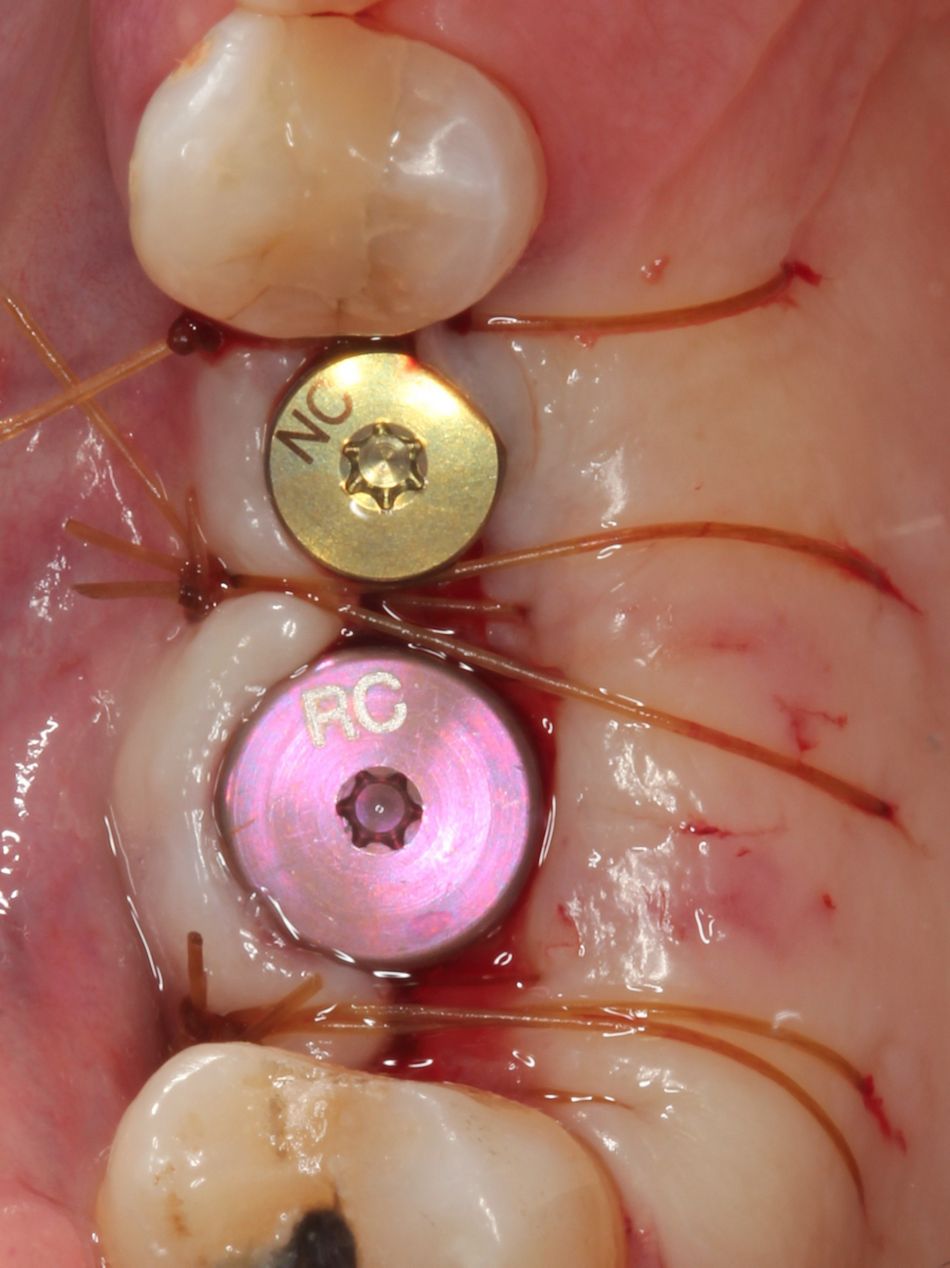
The patient understood that tooth #24, #25, and the implant in position #26 had a hopeless prognosis and would be lost. Her restorative options included either a fixed implant solution or removable prosthesis. However, the patient would only consider an implant supported fixed bridge.
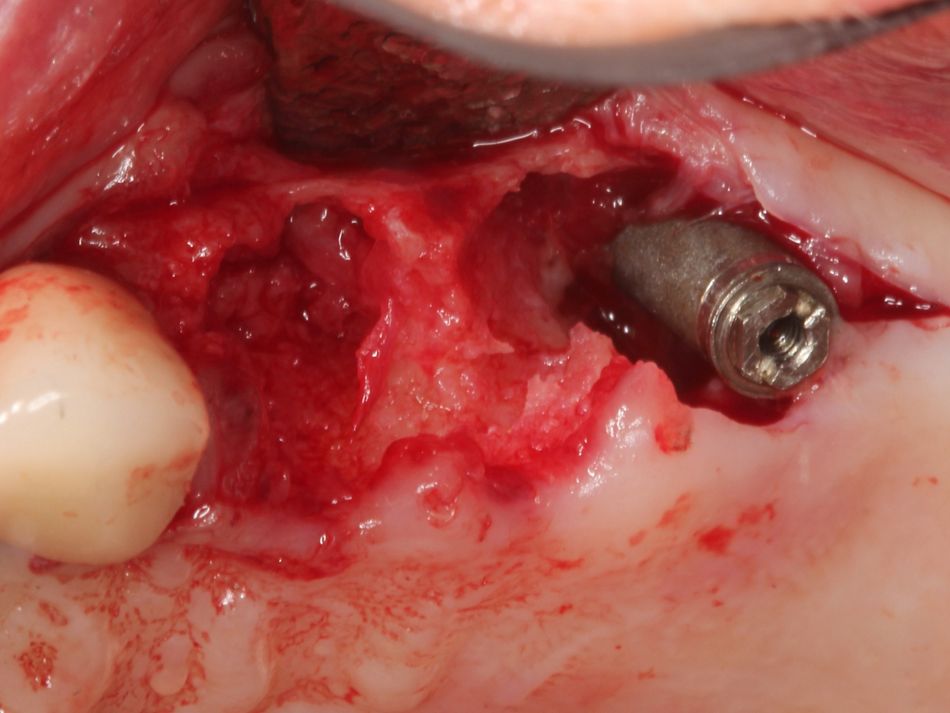
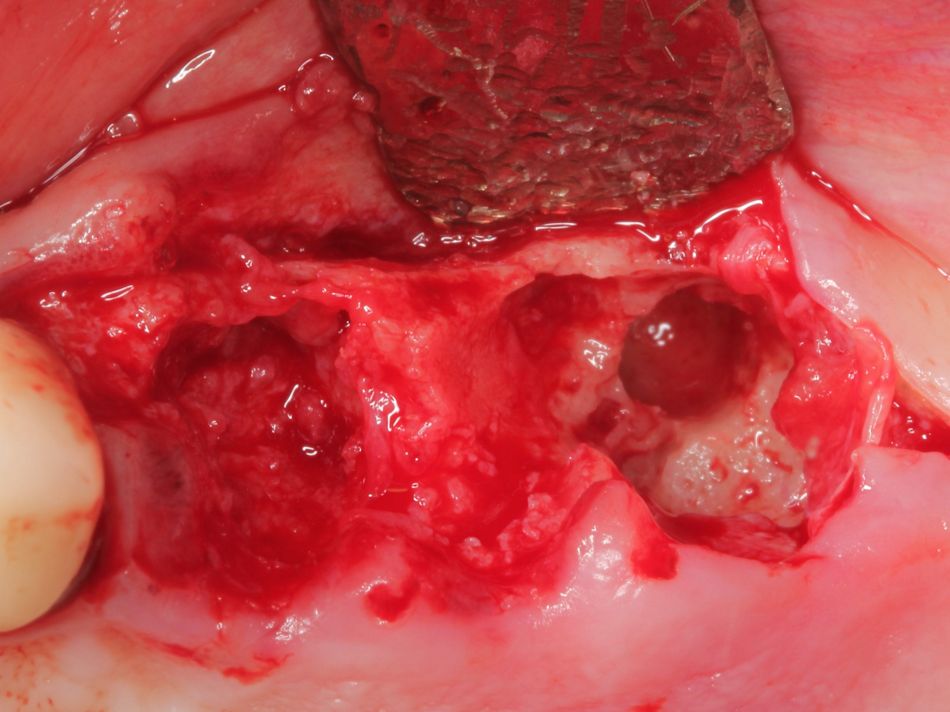
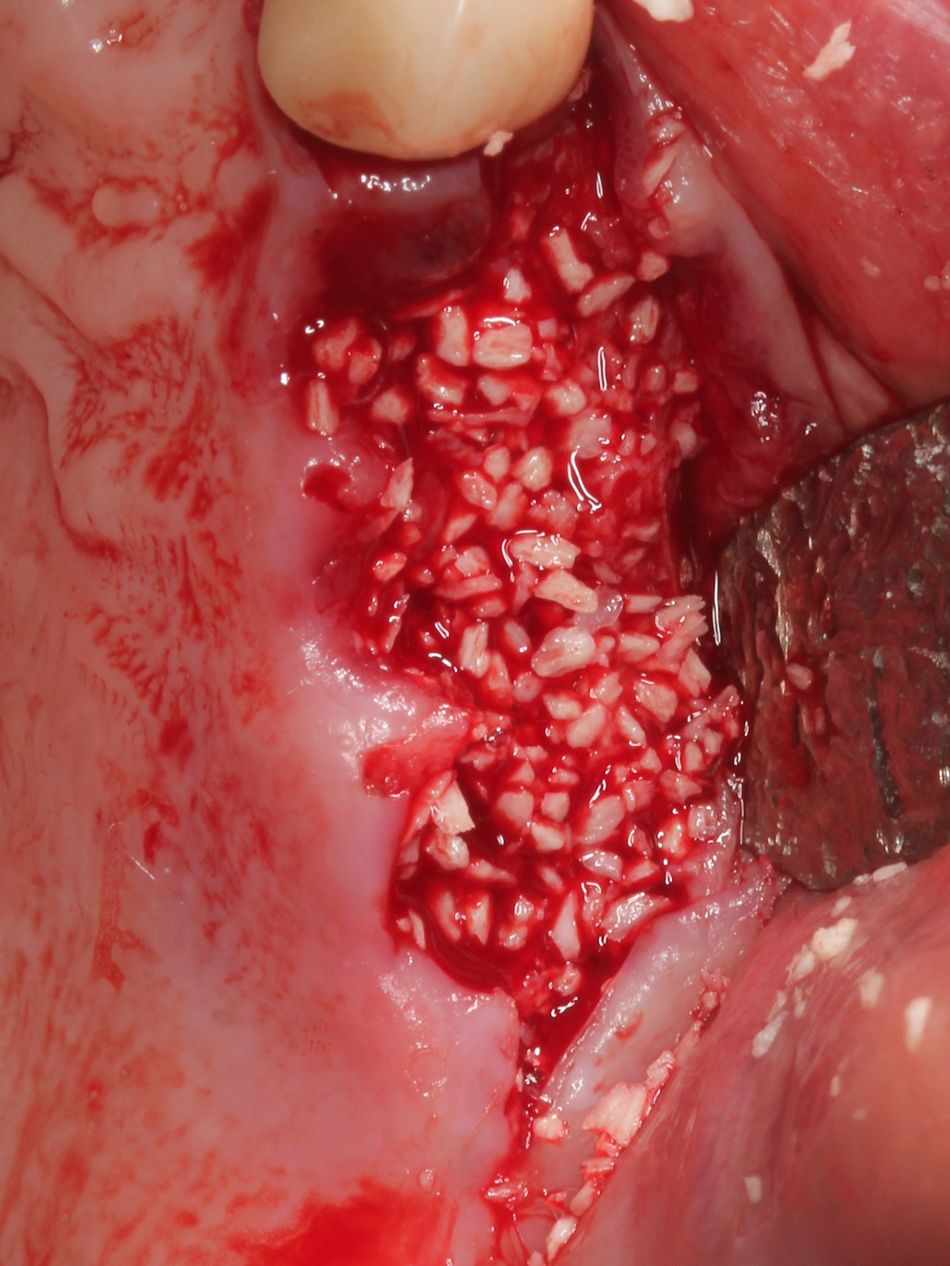
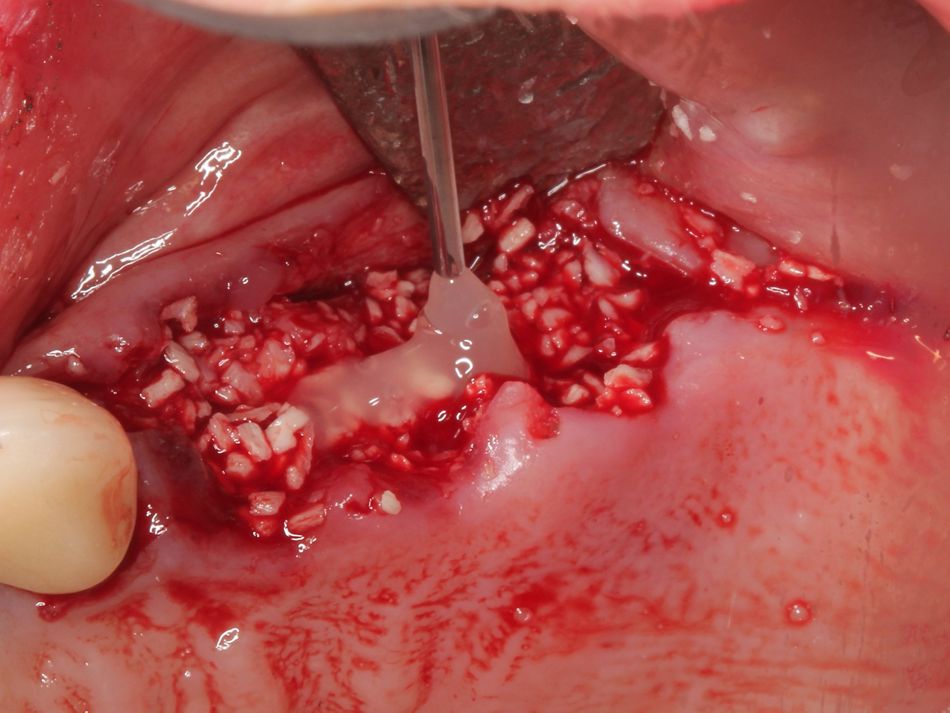
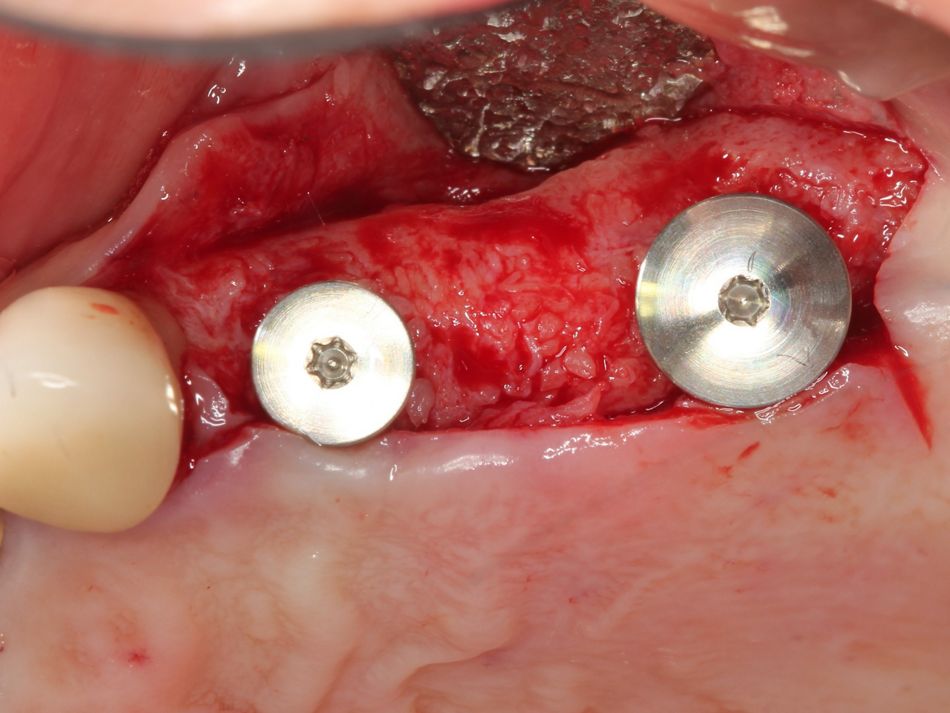
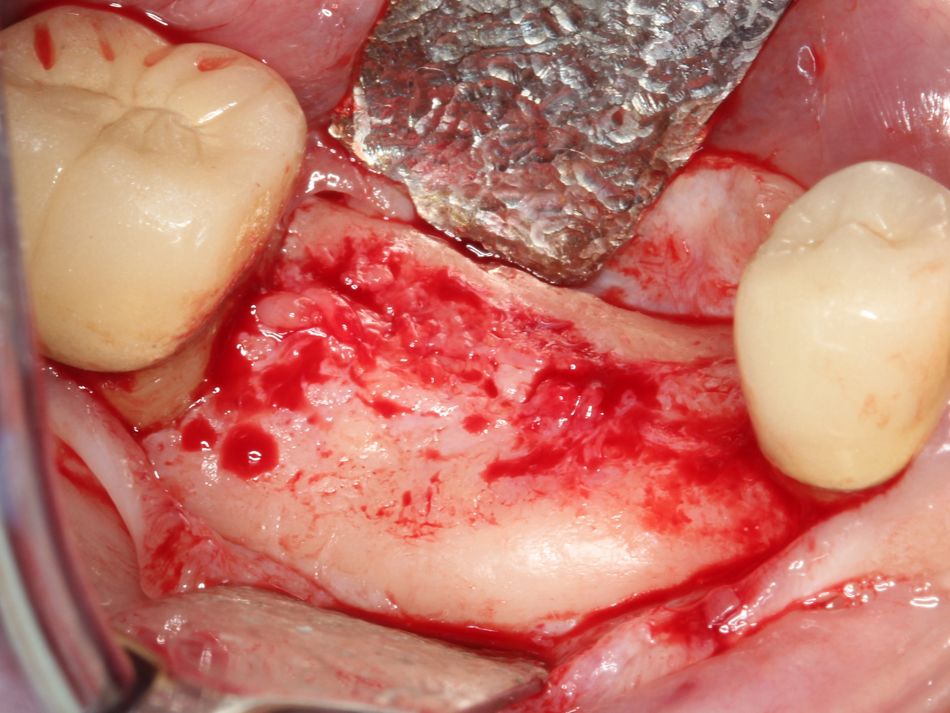
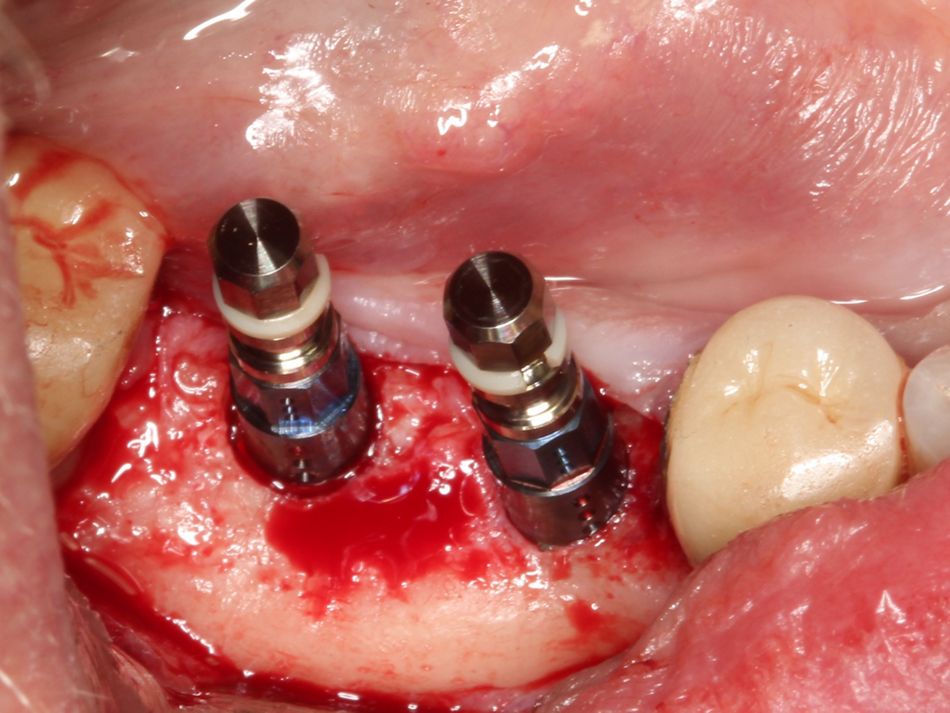
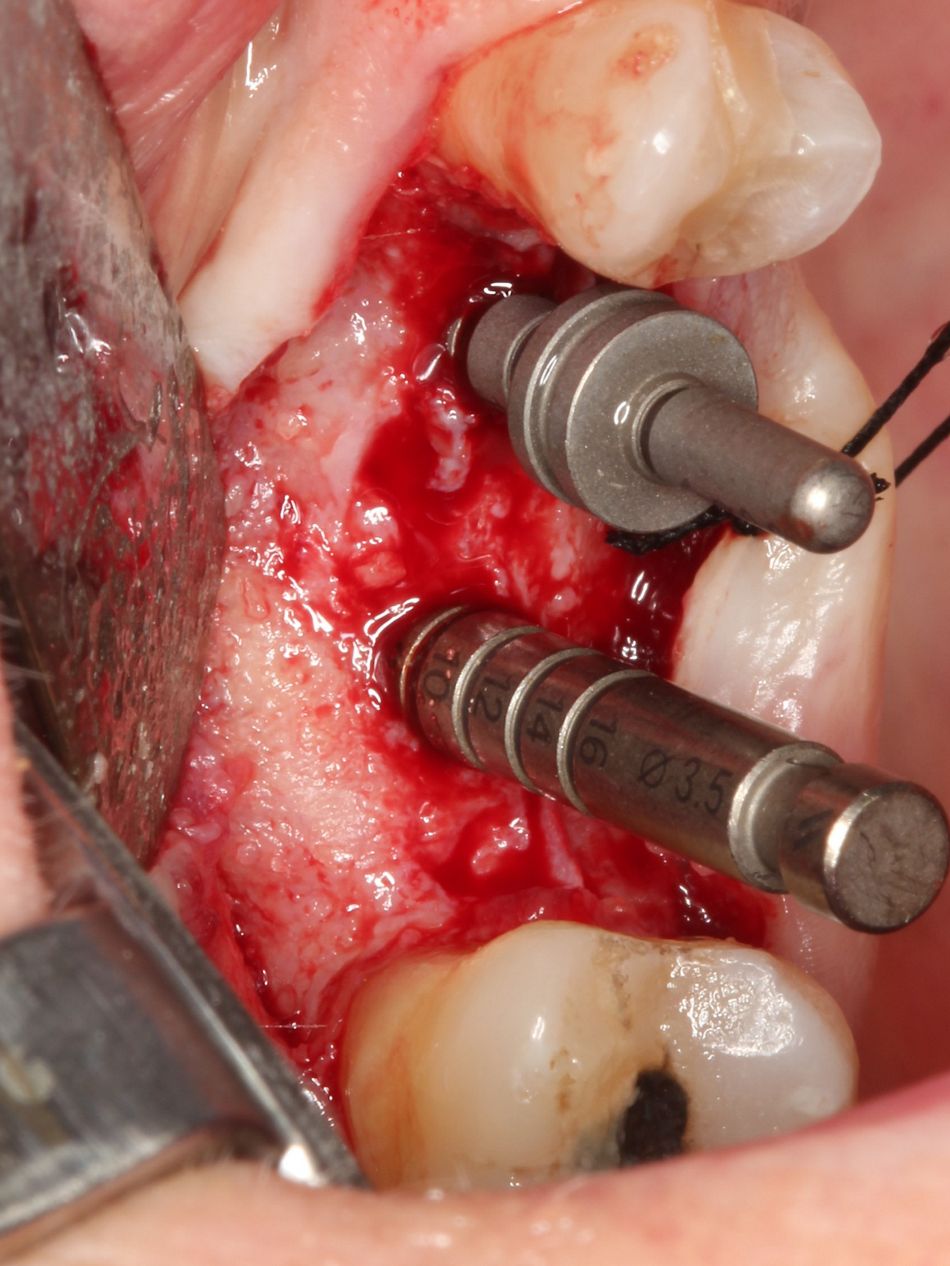
The plan was to remove #24, #25, and #26 and regenerate the ridge prior to placing dental implants. Due to the size of the defect, and quantity and quality of bone which we would need to successfully place and restore the dental implants, it became clear that a two-stage procedure using a combination of Straumann® Emdogain® and Straumann® allograft was the treatment of choice.
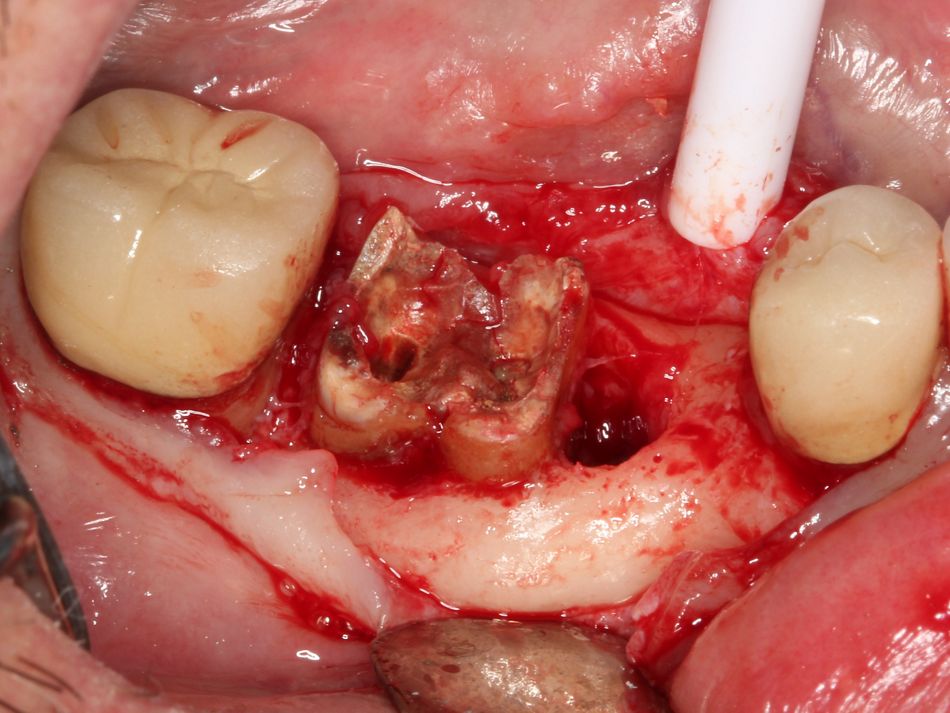
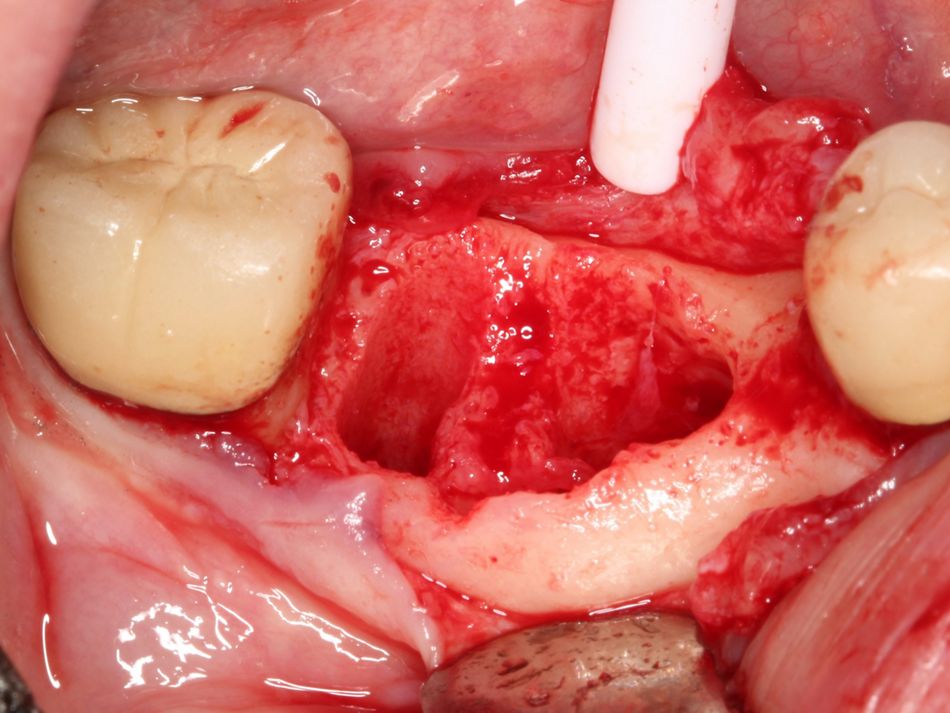
Surgical procedure
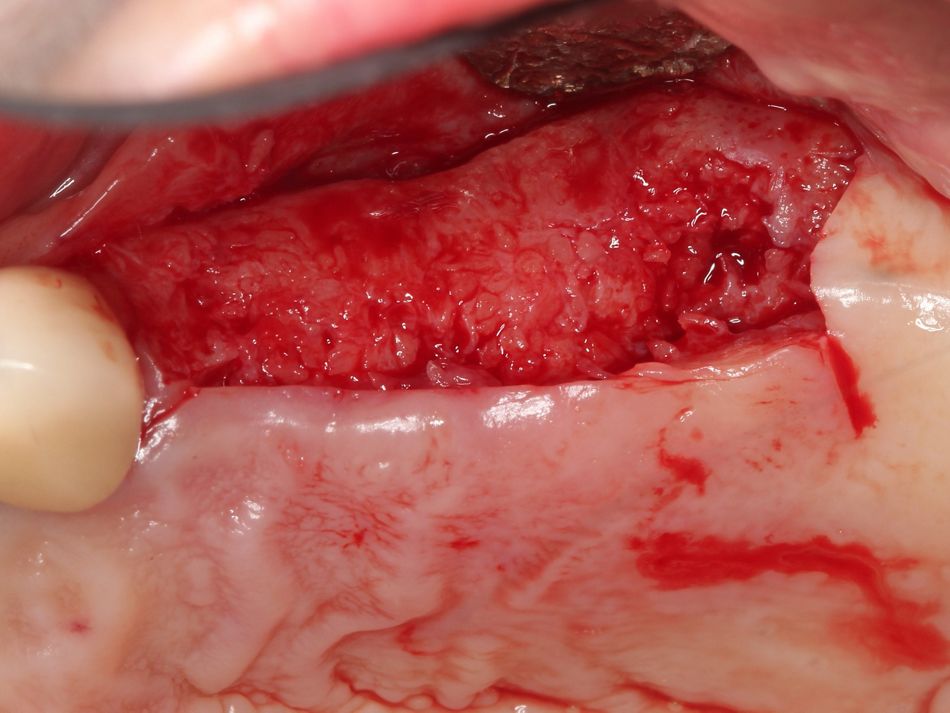
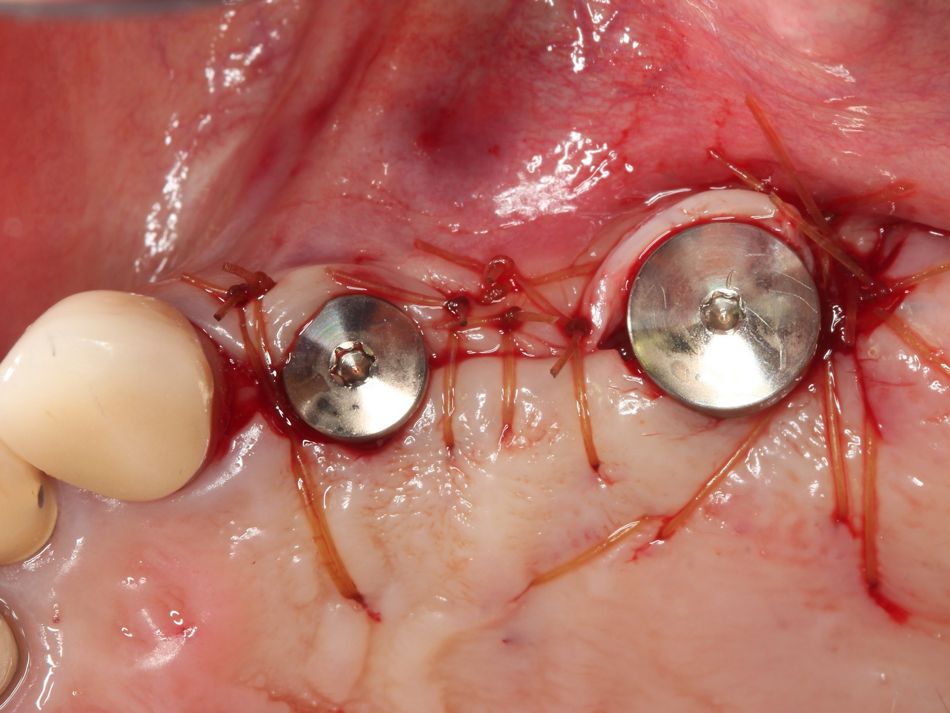
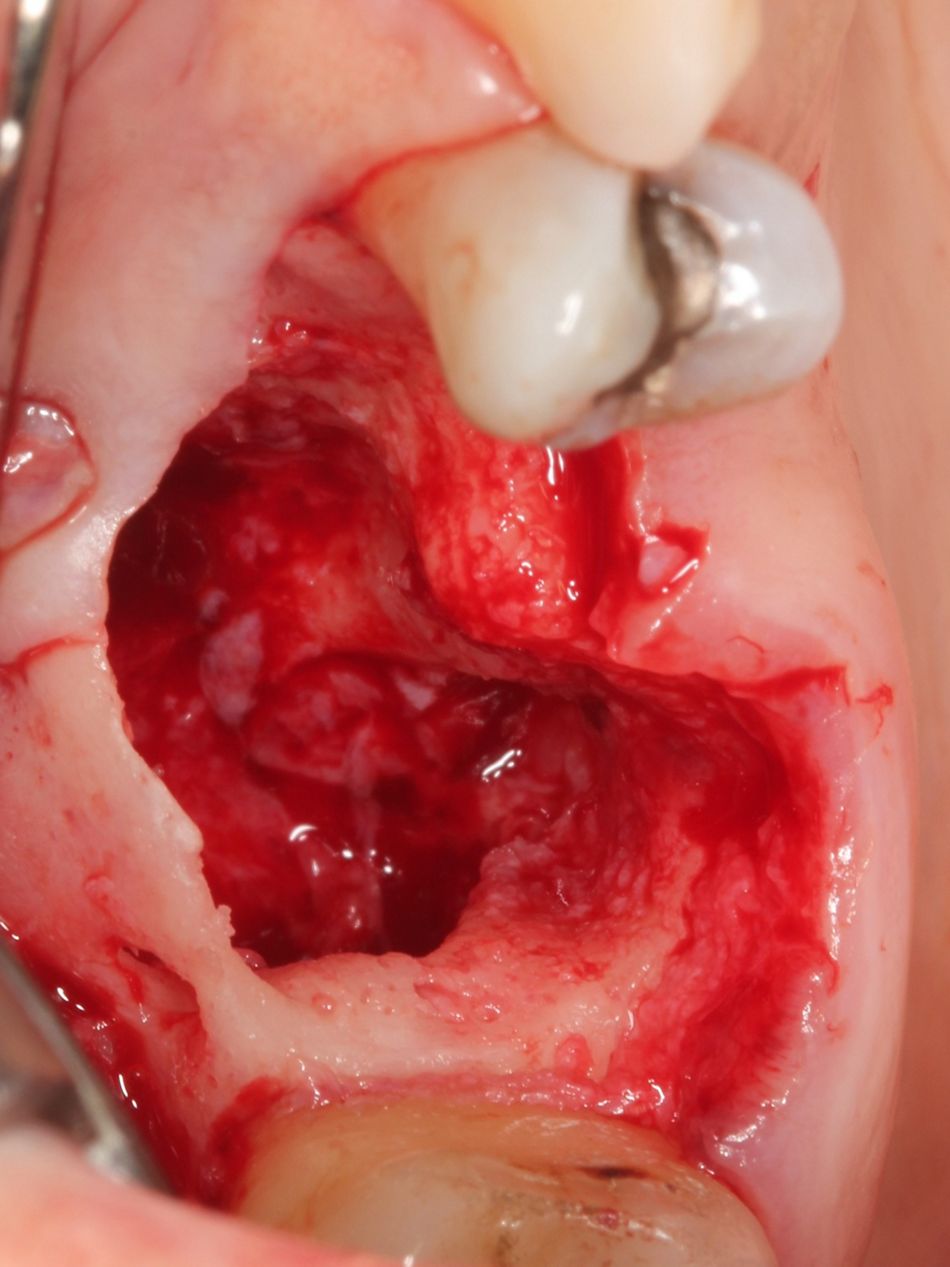
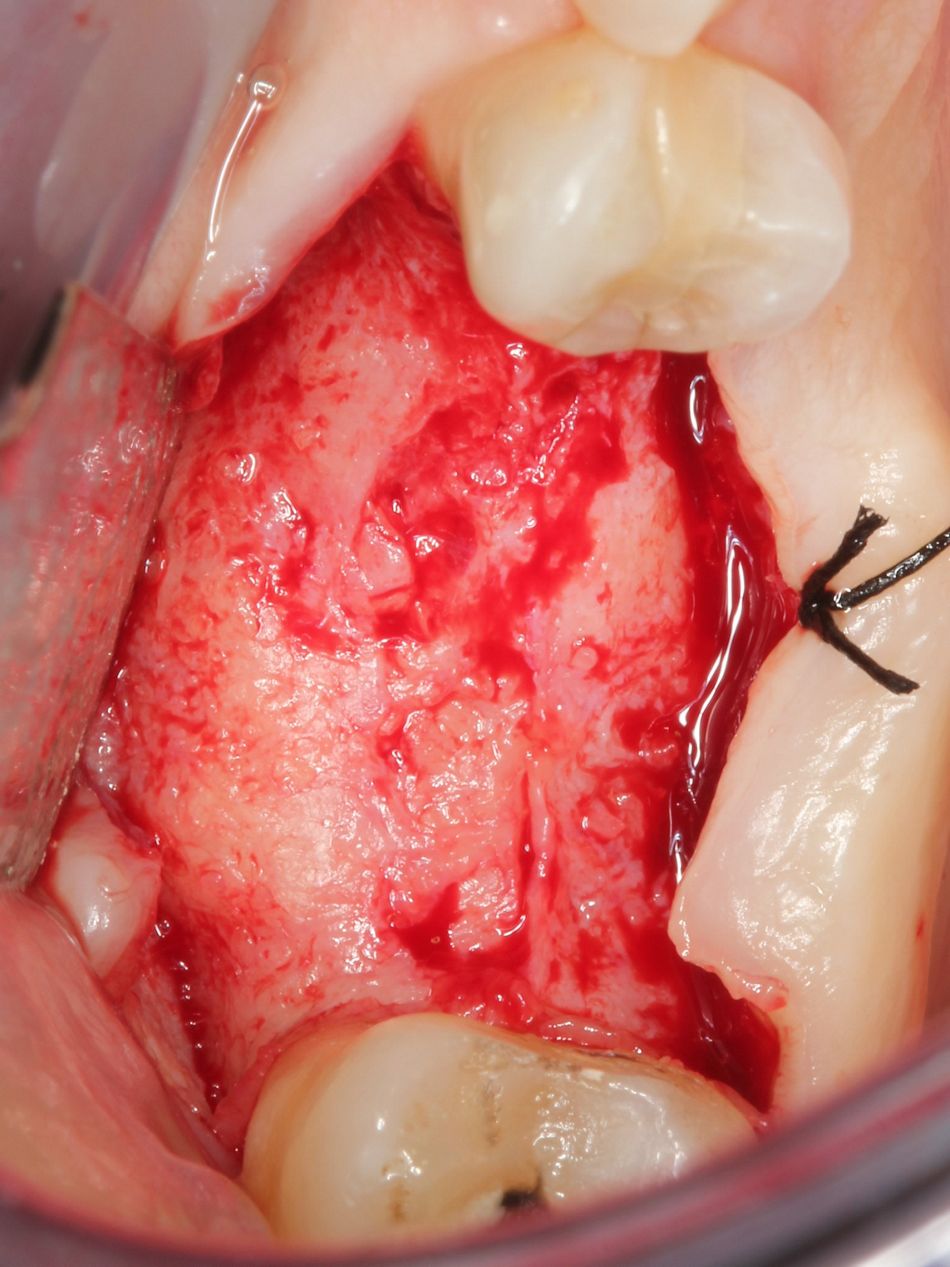
Standard surgical protocol was followed. The patient rinsed with chlorhexidine gluconate 0.12% prior to the surgery and was anesthetized with Lidocaine Hydrochloride 2%. After the restorations were removed, the teeth and implants were extracted with elevators and forceps. The area was thoroughly debrided of any soft tissue remnants and rinsed with chlorhexidine Hydrochloride 0.12%.
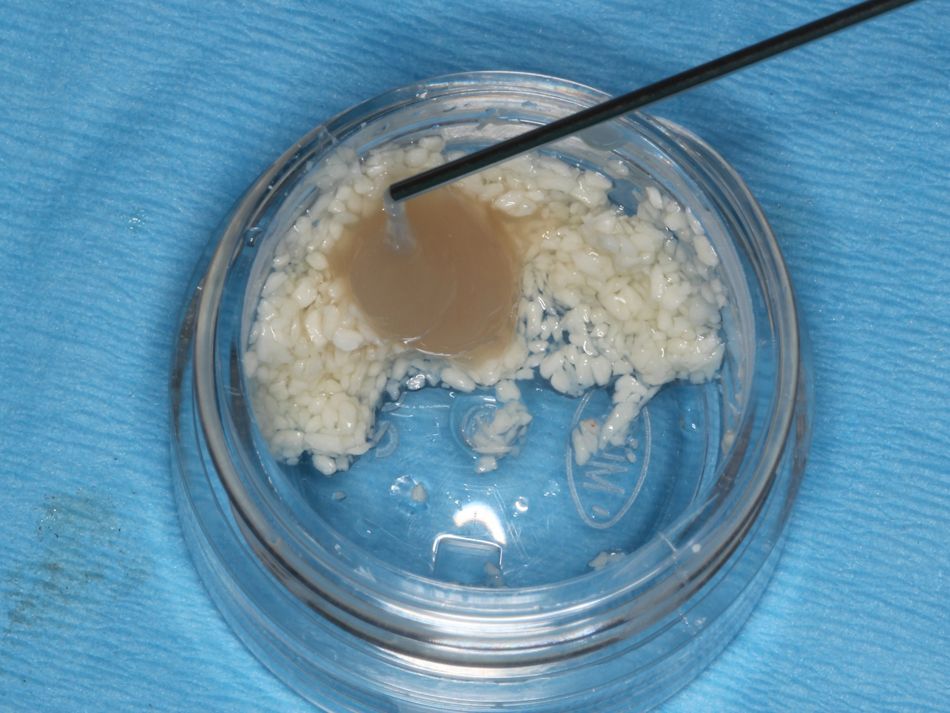
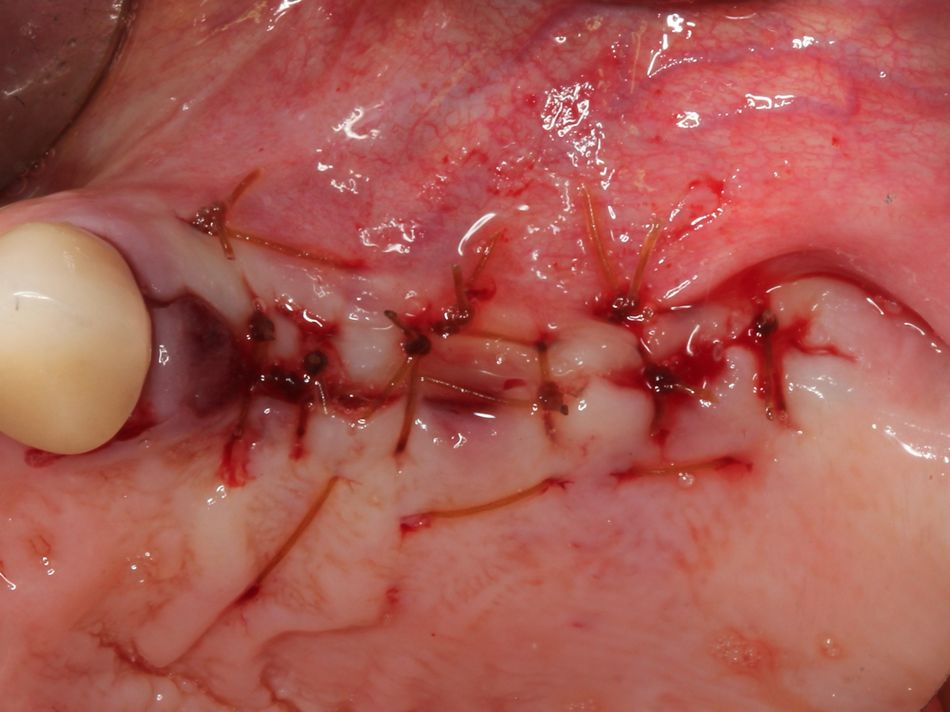
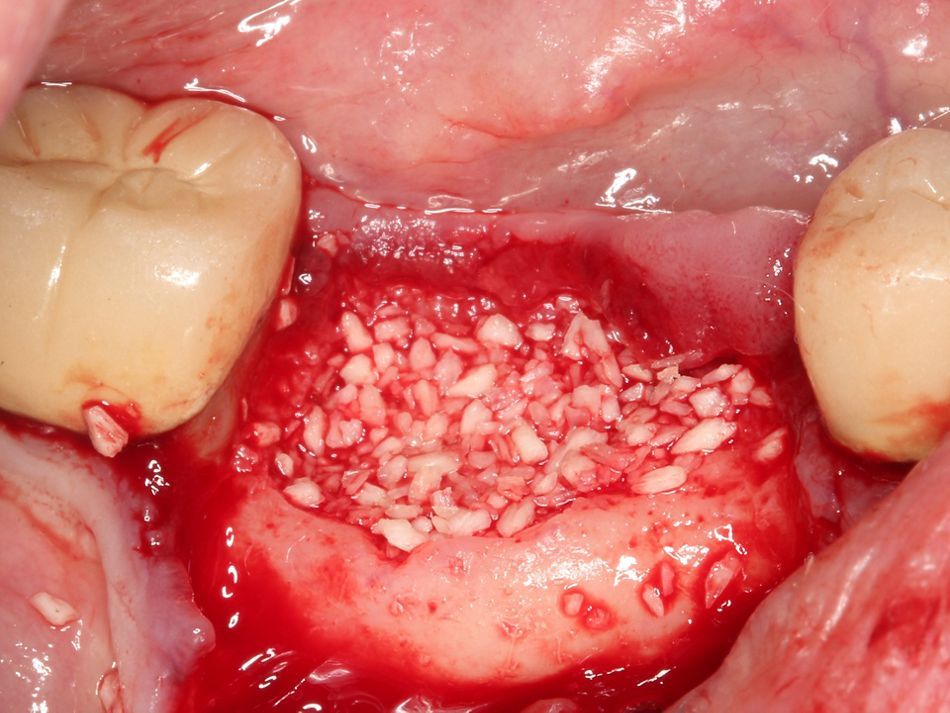
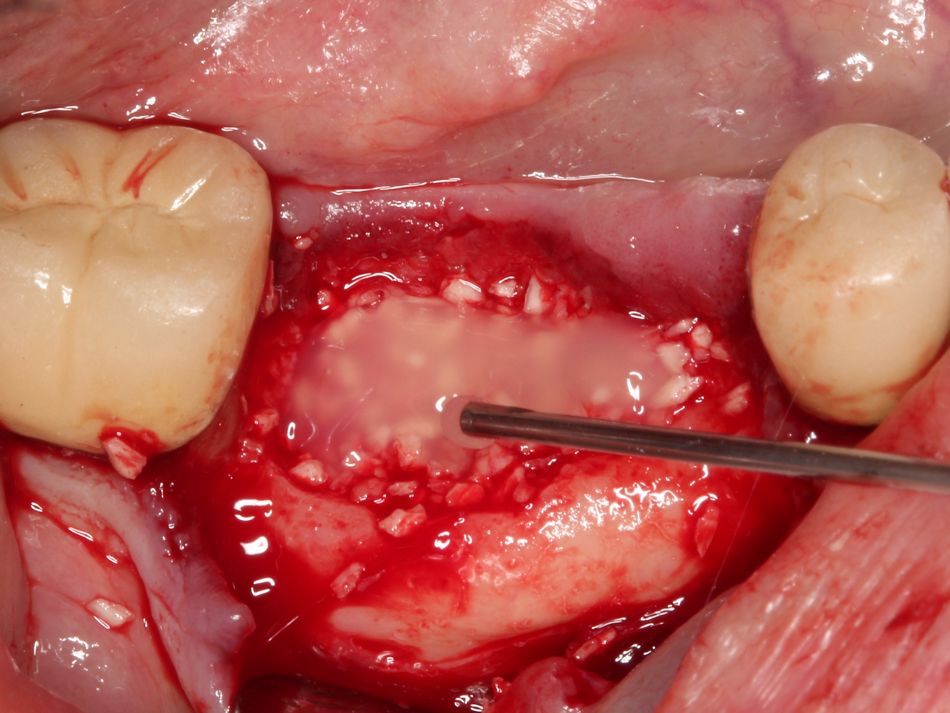
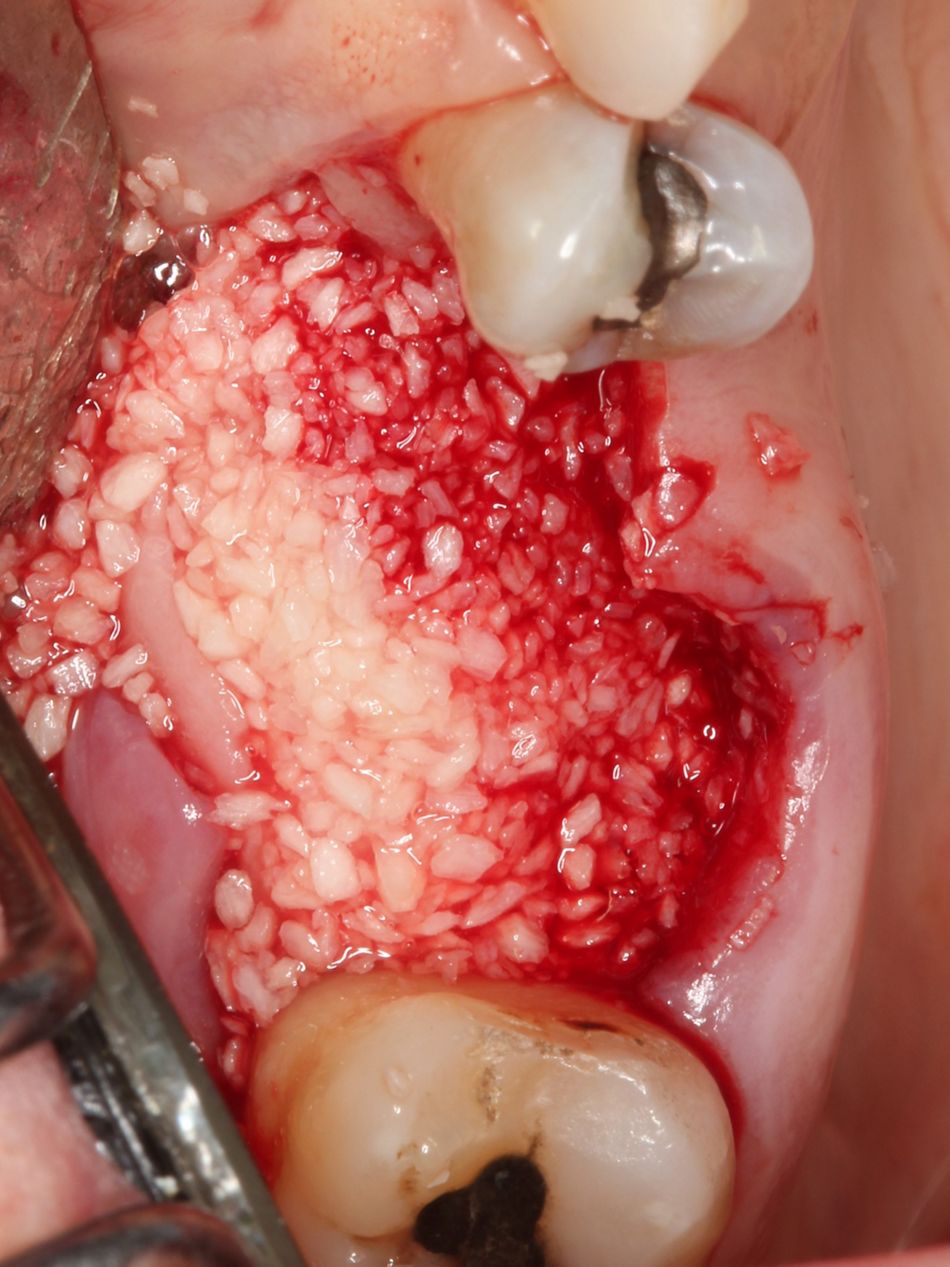
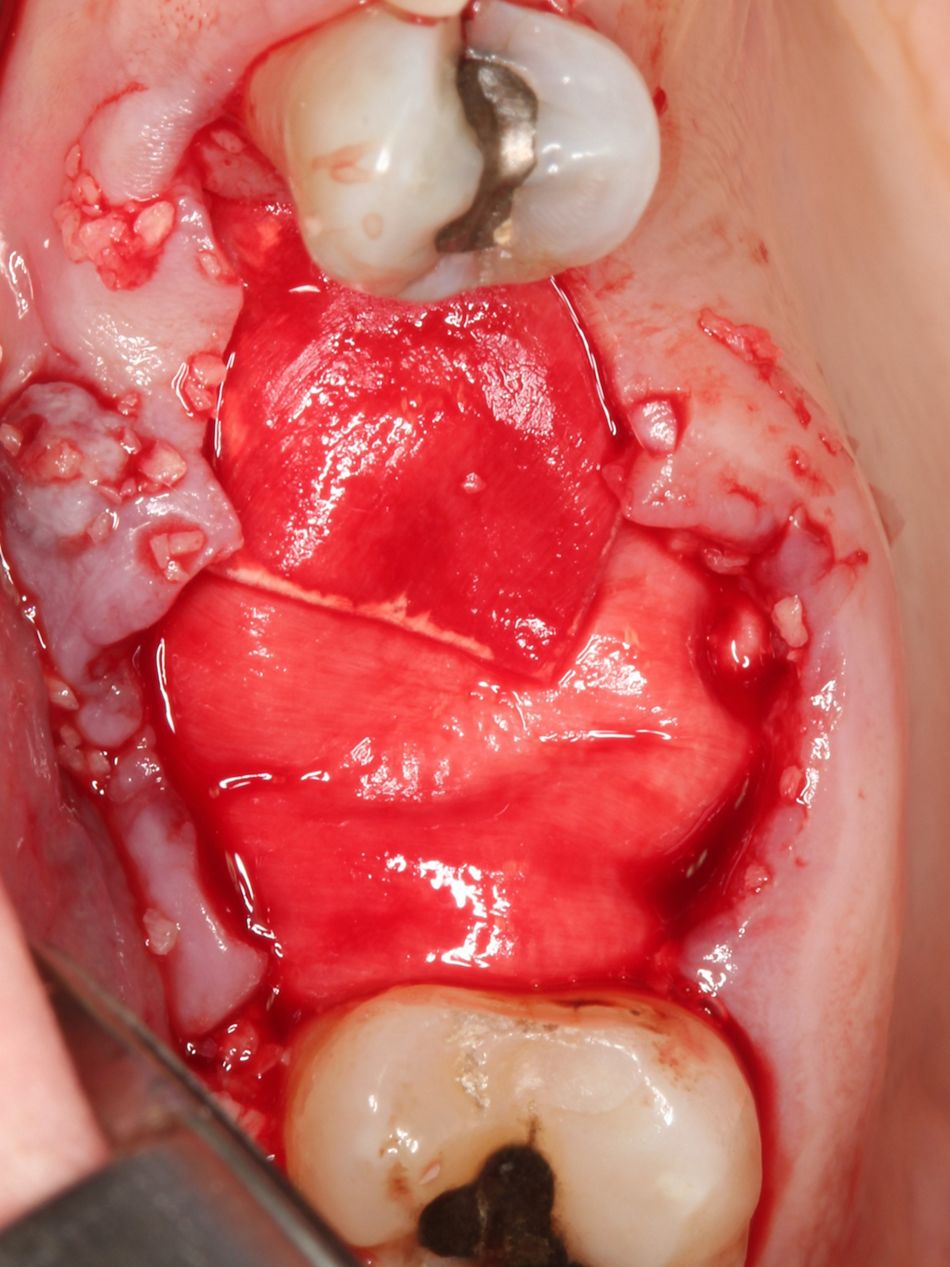
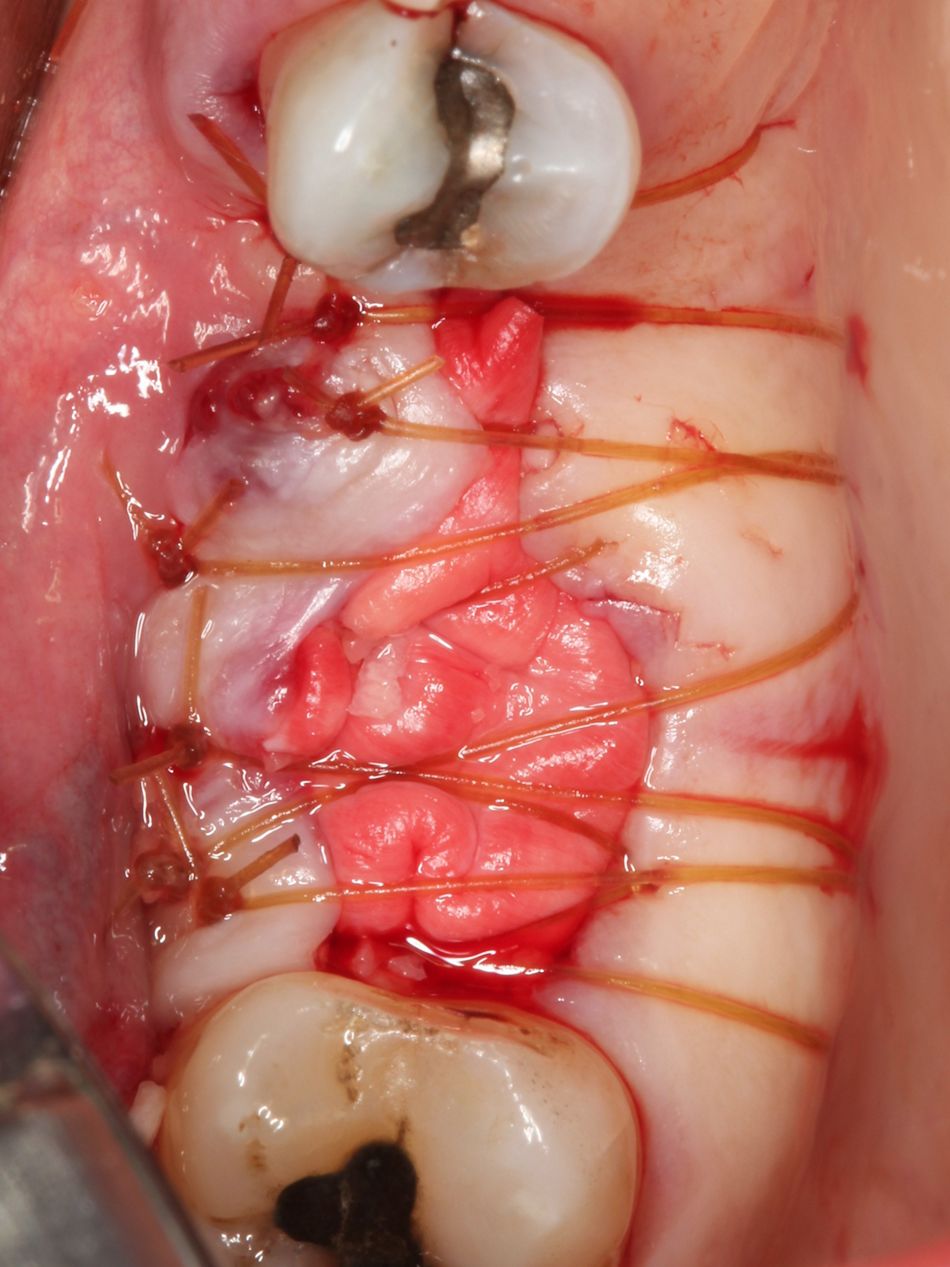
The decision to use Straumann® Allograft, 1.0 cc (250 – 1000 microns) - a mineralized freeze-dried bone allograft - was based on its resorption / turnover time and the fact that we had a 4-wall contained defect. The graft was hydrated with sterile water and mixed with Straumann® Emdogain® 0.15 ml prior to being packed in the defect. Straumann® Emdogain® was also placed at the suture line to aid in the soft tissue healing.
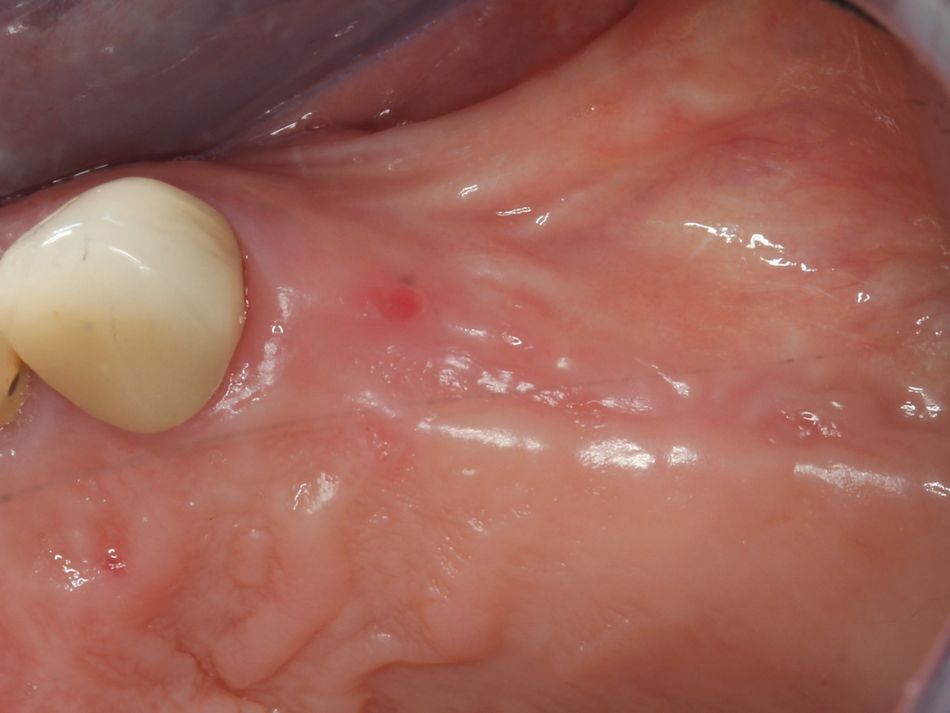
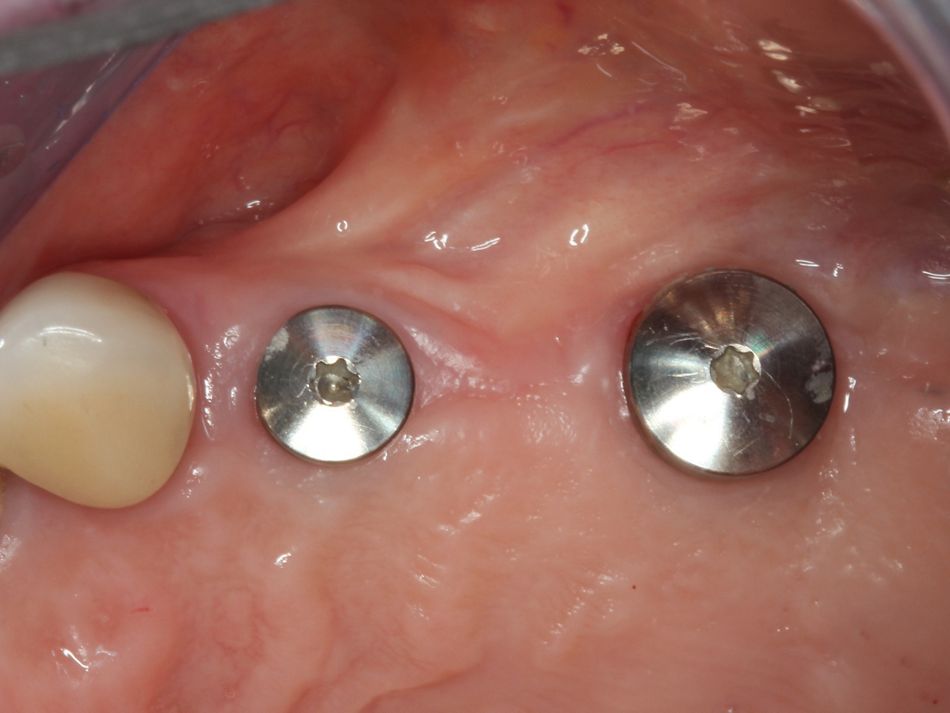
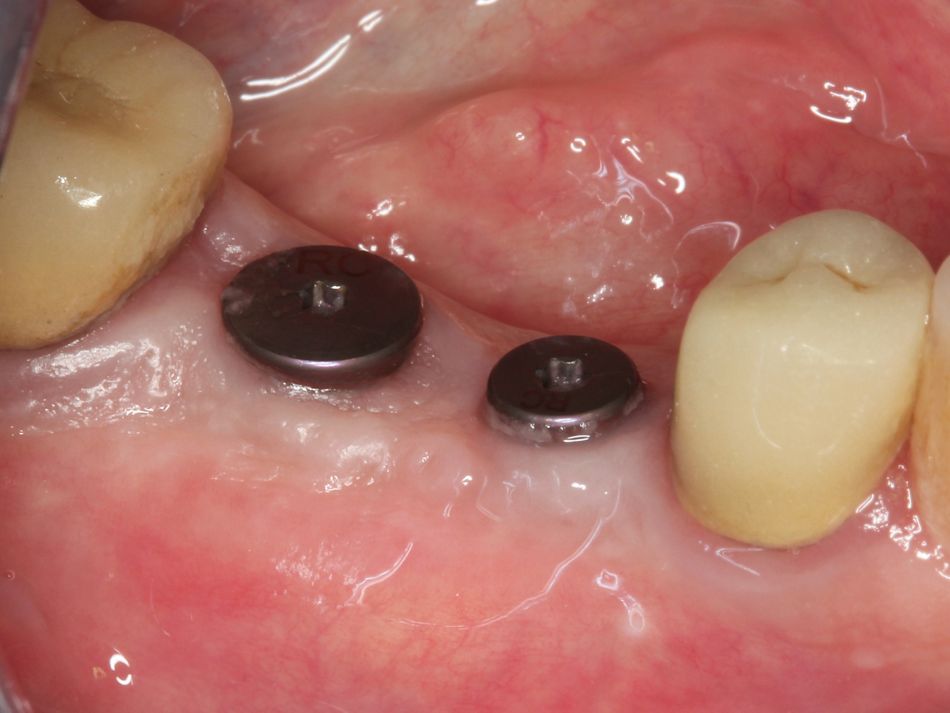
Treatment outcomes




.JPG?wid=236)
.JPG?wid=230)
.jpg?wid=393)




.JPG?wid=200)
.JPG?wid=197)
.JPG?wid=197)
.JPG?wid=345)


.png?fmt=png-alpha&wid=277)
.png?fmt=png-alpha&wid=280)


.png?fmt=png-alpha&wid=283)
).png?fmt=png-alpha&wid=272)