Plastic periodontal surgery combining mucoderm® and Emdogain®
A clinical case report by Dávid Botond Hangyási, Hungary
This case report describes the predictable coverage of multiple adjacent maxillary gingival recessions using the modified coronally advanced flap (MCAF) technique and modified coronally advanced tunnel technique (MCAT) in conjunction with an acellular porcine-derived collagen matrix (mucoderm®) combined with enamel matrix derivative (Straumann® Emdogain®). The author states: "In my opinion, this case can be viewed as satisfactory both for the patient and the operator, effectively demonstrating the benefits of the combination of mucoderm® and Emdogain® as regards time and pain."
Initial situation
A 30-year old female patient in good general health conditions presented with Miller Class I gingival recessions in the upper jaw affecting the teeth #12, #13 and #14 and teeth #22, #23 and #24 (Figs. 1-3), and was referred to our office by an orthodontist colleague (Enikő Szívos, DMD, orthodontist). The patient sought a minimally invasive approach to improve ther aesthetic appearance and to facilitate brushing.
Treatment planning
To achieve a satisfactory aesthetic result with, at the same time, minimal traumatization of the soft tissues, a minimally invasive approach was chosen to cover the exposed roots. Professional oral hygiene was implemented prior to the scheduling of regenerative therapy with mucoderm® and Emdogain®. We decided to perform the coverage before the orthodontic therapy, and we also decided to use different surgical procedures and biomaterials depending on the local clinical situation.
As we wanted to improve the quality of attachment, we decided to use PrefGel®/Emdogain®. In some places the thickness of keratinized gingiva was not adequate. To thicken the gingival tissues and produce more keratinized gingiva, we planned to apply mucoderm®.
Surgical procedure
The old cervical fillings were removed. The exposed root surfaces were cleaned with curettes, under local anesthesia, in the region #12 to #14, and split thickness oblique papillary incisions were made according to the modified coronally advanced flap (MCAF) technique (Zucchelli & DeSanctis J Periodontol 2000), thereby creating a new "surgical papilla" and a connective tissue bed (Figs. 4, 5). The anatomical papillae were de-epithelialized to extend the connective tissue bed. Root conditioning was performed with Straumann® PrefGel® for 2 minutes, Straumann® Emdogain® was applied all over the clean, blood-free root surfaces (Fig. 6). mucoderm® was trimmed to the desired size and rehydrated for ten minutes in sterile saline solution. Next, the collagen matrix was placed over those exposed root surfaces exhibiting the most prominent recessions (teeth #12 and #13) and immobilized at the level of the cementoenamel junction with palatal sling sutures (Fig. 7). A periosteal releasing incision was made to allow for coronal positioning and suturing of the elevated flap. Finally, buccal sling sutures and modified sling sutures were used to fix the flap and achieve primary wound closure (Fig. 8). Suturing was performed according to the double-sling technique with 6/0 non-resorbable monofilament suture material. To treat the recessions in the region #22 to #24, the modified coronally advanced tunnel (MCAT) approach (Azzi & Etienne, 1998) was chosen. Before the tunnel was prepared, the exposed root surfaces were mechanically cleaned, Straumann® PrefGel®, followed by Straumann® Emdogain®, were applied all over the root surfaces (Fig. 9). The tunnel was then prepared using tunneling knives, and the collagen matrix was rehydrated for 10-20 minutes. Next, the collagen matrix was pulled into the tunnel with the help of vertical mattress sutures (Figs. 10, 11). The graft and tunnel were positioned by double-sling suturing (6/0 non-resorbable monofilament sutures), the graft being about 2 mm apically from the CEJ. The flap was moved in a coronal direction to cover the mucoderm® matrix completely, and primary wound closure was achieved (Figs. 12-15). Post-operatively, the patient was instructed to rinse with chlorhexidine solution twice a day for 2 weeks, but no other medication was prescribed. The patient refrained from mechanical tooth brushing for the first two post-operative weeks to avoid traumatizing the treated area. The sutures were removed two weeks after the surgery.
Final result
The post-surgical healing was uneventful. At 20 months following regenerative therapy with mucoderm® and Emdogain®, the clinical situation appeared stable (Figs. 16, 17). Previously exposed tooth roots were covered in a satisfactory manner, and significant thickening of the marginal gingiva was visible. This stable clinical outcome was maintained in the long term, as demonstrated at 27 months after the surgery (Fig. 18). The patient expressed a high level of satisfaction, specifically with respect to the healing process and the aesthetic appearance of the treated teeth.
Conclusion
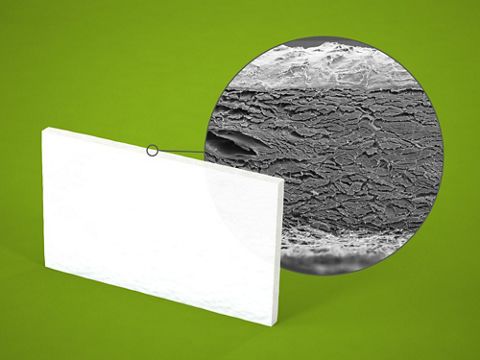
The case presented here illustrates the successful coverage of exposed tooth roots with simultaneous thickening of the marginal tissue using a less invasive approach by applying the collagen matrix mucoderm® in combination with Emdogain®. The post-operative follow-up revealed complication-free healing and a stable clinical situation two years after the surgical intervention. This approach is characterized by a high level of acceptance by the patient, since harvesting of an autologous soft tissue graft is avoided and a satisfactory aesthetic result is achieved. Thus, to cover Miller class I and II multiple recession cases, if a satisfactory amount of keratinized gingiva is available apically to the recession, then MCAF and MCAT represent predictable procedures if used with the combination of mucoderm® and Emdogain®.
In my opinion, this case can be viewed as satisfactory both for the patient and the operator, effectively demonstrating the benefits of the combination of mucoderm® and Emdogain® as regards time and pain.