Predictable GBR procedures in sites with high esthetic compromise
A clinical case report by Jorge M. Galante, Argentina
The patient, a 45 year-old female in good general systemic health, had undergone some unsuccessful dental treatments, with failed restorations resulting in the loss of multiple maxillary teeth. Teeth 1.2 to 2.2 were extracted after failed endodontic treatments and periapical complications. The aim of the patient was to replace the removable partial prosthesis with a fixed implant supported restoration.
Treatment planning
The clinical examination showed a significant horizontal deficiency of the anterior(Figs. 1, 2). Panorex Rx (Fig. 3). Study models mounted on a semi-adjustable articulator were taken and a diagnostic wax-up of the four incisors was made with a modeled gingiva (Fig. 4) to provide an idea of the amount of tissue to be regenerated. In the axial slices and the 3D reformatted CT images, the lack of bone in the horizontal and vertical dimensions could be evaluated precisely. A stepwise surgical approach was planned: in a first step, a GBR procedure would be performed. In a second step, two submerged implants should be inserted and, if necessary, an additional GBR procedure performed. In a third step, implants should be uncovered together with a soft tissue augmentation. The initiation of the prosthetic phase was planned 30 days after the implant activation surgery.
Surgical procedure
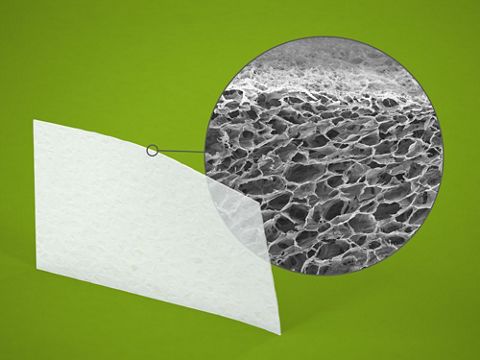
Under local infiltrative anesthesia, a full thickness horizontal incision was made at the keratinized tissue, on the buccal 2.5 mm apical to the most coronal aspect of the residual ridge, extending intrasulcular to the distal papilla of teeth 13 and 23. Two vertical releasing incisions were performed distally to 13 and 23. A full thickness flap was elevated to expose the alveolar ridge. At the inner aspect of the flap, a split thickness incision was made to allow a complete mobilization of the flap in order to achieve a tension-free closure of the flap by primary intention. Two mini osteosynthesis plates were placed at the projection of the crestal peak of bone, corresponding to the interdental papilla between 12/11 and 21/22 (Fig. 5). These mini plates were used as tent poles and support to avoid the collapse of the collagen membrane. Each mini plate was fixed with two self-tapping micro screws (Walter Lorenz, 1.2×4 mm). The mini plates were shaped to reproduce the ideal anatomic profile of the ridge, creating a space underneath for the biomaterial and preventing collapse of the overlaying membrane (Fig. 6). The space under the mini plates was filled with Straumann® BoneCeramic. After that, the augmentation site was covered with two pericardium membranes (Jason® membrane, 20×30) placed at each side and fixed mesially and distally with 2 mini titanium pins (Figs. 7, 8). A suture was performed with a nylon monofilament 5.0 (Ethicon). The first suture was at the vertical incisions distal of 13 and 23, replacing the papilla with a vertical mattress suture. Another three vertical mattress sutures were placed mesially of both teeth and at the midline. Two horizontal mattress sutures were performed at each side. Both vertical and horizontal mattress sutures cause eversion of the flaps to face connective tissue at each side of the wound. The closure was completed with an interrupted simple suture along the horizontal and vertical incisions (Fig. 9). The healing process was uneventful; sutures were removed three weeks post-op. Six months post-op, the clinical evaluation demonstrated a nice macroscopic contour of the regenerated area (Fig. 10). Images of paraxial slices and 3D reformatted CT (Fig. 11) showed very good integration of the biomaterial, adopting the shape predetermined by the mini plates. The second surgical approach consisted of a horizontal incision and two verticals, the same as in the first surgery. The full thickness flap elevation revealed homogeneous, well-vascularized hard tissue. The mini plates were partially covered by newly formed bone (Figs. 12, 13). Once the plates were retired, two Straumann® Bone Level, implants (4.1/14) were installed in region 12 and 21 with the help of a surgical stent (Figs. 14, 15). Biomaterial and a Jason® membrane were added in the midline with the intention of gaining extra volume for esthetic reasons.Wound closure was performed according to the first surgical intervention. Again, the healing was uneventful and sutures were removed three weeks post-op. Three months later, uncovering of the implants was performed with a soft tissue management to improve the peri-implant esthetics (Fig. 16). Healing screws were installed at implants. A ramp suture was made to promote coronal advance of the entire flap (Fig. 17).
Prosthetic procedure
Two weeks later, sutures were removed, and the temporary fixed screw-retained partial prosthesis was placed (Fig. 18). Teeth 13 and 23 were prepared for full crowns (Fig. 19). As the patient was under orthodontic treatment, it was decided to make a new resin fixed screw-retained prosthesis in order to have ideal conditions for the placement of the two implants to replace teeth 24/25, and to delay the definitive porcelain restorations once the case was completed (Fig. 20).
Final result
The treatment planning of complex cases like this one, with a young patient and high esthetic expectations, is challenging. Although the total treatment time is longer, the results obtained by this stepwise approach allow the interdisciplinary team to interact in a more secure and precise way(Figs. 21, 22).
Findings
A remarkable finding was the extent of the regenerated tissue, taking into consideration the extended three-dimensional horizontal and vertical defect. The other significant aspect is that only synthetic biomaterial was used with no need for autologous bone. The fact that the mini plates prevent a collapse of the membrane may be favorable for regeneration. In addition, the pericardium membrane provides a long-term barrier function, giving the biomaterial sufficient time to integrate. Further investigation should be made in the field to encourage this kind of method to be applied as a valid procedure in the treatment of three-dimensional defects.