
Dr. Steve Eckert
An interview with Steve Eckert
“It's the clinician's personal responsibility to select the appropriate implant to be used in the specific situation”
Steve Eckert, Full Professor Emeritus in Dentistry at the Mayo Clinic College of Medicine, Adjunct Professor at the University of Minnesota School of Dentistry and Director of Research for ClearChoice, has recently published 1 year follow up results from a randomized trial addressing immediately loaded fixed full-arch implant-retained prosthesis with Straumann® Bone Level Tapered implants used according to the Straumann® Pro Arch treatment protocol.
Prof. Eckert, could you please tell us more about the study setup and important findings?
I think it is important to understand that this study was a non-interventional assessment of the clinical performance of an immediately placed and loaded fixed full arch prosthesis supported by dental implants.(1) The study began when the practice shifted to a different type of implant than had been used for the previous six years. The study itself was conducted from August 1, 2015 and the last implant prosthesis that was followed in this study was placed on or before December 31, 2016. Our goal was to determine that a different type of implant may be as effective to demonstrate improved effectiveness in a clinical setting. The implant used in the study was the Straumann® Bone Level Tapered (BLT) implant (Roxolid®, SLActive®). We have followed the Straumann® Pro Arch treatment protocol involving immediate full arch restoration in edentulous patients.
“It was a non-interventional assessment of the clinical performance of an immediately loaded implant supported and retained prosthesis.”
It was a non-interventional assessment of the clinical performance of an immediately loaded implant supported and retained prosthesis. It is important to understand that this study was not a randomized controlled clinical trial. I think that it would be unrealistic to perform a study of this size as a randomized controlled clinical trial in dentistry. Perhaps it is possible in medicine but to create a randomized controlled clinical trial for this number of subjects for this length of time with an equal sized control group the cost of such a study would be prohibitive in excess of twenty million dollars.
The patient population was consecutively treated patients who consented to participate in this study by having their de-identified data analyzed for clinical performance. This represented every patient who was treated in the office during the time frames described above for full arch prostheses using bone level tapered implants. The number of implants that were placed and restored was 1903 and the mean follow-up time in the study was 484 days with a maximum of 972 days. This study was conducted with all but one of the fixed implant supported prosthesis succeeding in the intent to treat 440 out of 441 planned prostheses were restored with immediately loaded fixed dental prostheses. It is also important to understand that the implants were not only placed but also restored in that same office. Consider this carefully, in a little more than 15 months, dental implants were placed and restored provisionally with our primary intention to treat being done with the intention of performing immediate loading.
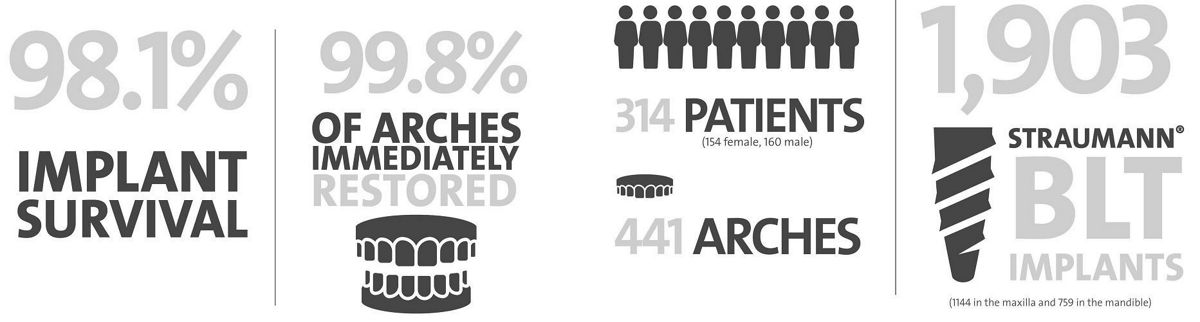
Figure: Key figures of the NIS conducted by Steve Eckert et al. (Int J Oral Maxillofac Implants. 2019 May/June; 34(3):737-744)
Apart of high survival rate, you have demonstrated that insertion torque appeared to have no effect on implant survival. Why, in your opinion, the insertion torque seemed to not be critical?
The study really was not conducted in an effort to prove whether insertion torque was or was not responsible for implant survival. When you look at the study however you will notice that the confidence intervals for survival of implants for the three groups, based on insertion torque, all overlap. These data demonstrate no significant differences among insertion torque for the three groups that were evaluated. On the other hand, if we would ask why the insertion torque seemed to not be critical, my answer would be that I believe there is splinting of the implants with a rigid, fixed prosthesis. This rigid prosthesis appears to prevent the implants from exhibiting microscopic motion that could interfere with the achievement of osseointegration.
“Certainly, the tapered implant design will facilitate achieving higher insertion torque and today the idea of higher insertion torque seems to be winning the battle.”
In your study, almost 90% of implants achieved insertion torque of 35Ncm and higher. In your opinion, could the implant type you have used contribute to this value and facilitate insertion torque?
Implant design is going to have a lot to do with the performance of the implant. In our study, we have used bone level tapered implants. Certainly, the tapered implant design will facilitate achieving higher insertion torque and today the idea of higher insertion torque seems to be winning the battle. Obviously, the other way to increase insertion torque is using a smaller osteotomy. How small can the osteotomy become before the insertion of the implant creates a traumatic event? How much trauma can the bone respond to? We certainly understand some factors but not all.
How can implant material and surface topography facilitate the healing time, hence osseointegration?
Implant materials are certainly important. It is critical that the material that is used to fabricate an implant must be biocompatible. It would be nice to have the material that is used in implant fabrication to be chemically active but at the same time it should not be chemically active towards all biologic environments. It is well recognized that the micro- and nano-topography of the implant surface as well as its chemical modifications (e.g. hydrophilicity) will substantially contribute to the recruitment of cellular activity near or perhaps adjacent to the implant surface, hence facilitate osseointegration. The question is how long surface technology would contribute to the osseointegration process – is it important for a few days or few weeks or forever? My impression is that it would contribute towards the biologic integration over the period from a few weeks to, perhaps, two months. Personally I doubt that we have reached the point of absolute confidence towards every bit of knowledge relative to implant dentistry. Realistically, it is unlikely that this will ever be reached.
“It is well recognized that the micro- and nano-topography of the implant surface as well as its chemical modifications (e.g. hydrophilicity) will substantially contribute to the recruitment of cellular activity near or perhaps adjacent to the implant surface, hence facilitate osseointegration.”
How can you explain the low complication rate of monolithic zirconia prostheses vs. titanium frame and acrylic ones?
Ceramic materials are a lot harder than acrylic. Zirconia appears to be near the top of the current list of ceramic materials relative to hardness. Over the years we have used acrylic wrapped around titanium frames and we did so with very little understanding of what it is that we were doing. With experience we learned. We learned that we could not use a flexible titanium material especially when a cantilever was to be created so we used alloys or different grades of Titanium frame material. By the time that we arrived at the use of Zirconia we had already made mistakes. Repeating those mistakes with a different material seem like a silly idea so instead we took our cumulative knowledge and applied it to another material, Zirconia. So far it has been successful. Will it last indefinitely? I doubt that anyone has a confident answer to that question.
What is your decision making concerning the choice of number, type and position of implants?
The first thing to decide is whether or not you're talking about a full arch of replacement teeth. Secondarily, the question to addresses is whether or not this is a discussion of a fixed, definitive full arch prosthesis?
If those two caveats are agreed upon, it is pretty easy to say that the minimum number of implants per arch for the routine treatment of the maxilla or the mandible would be four implants. Depending upon the configuration of the maxillary sinus or the inferior alveolar canal, the posterior-most implant may be vertical, if the sinus and the canal are not interfering, or the posterior implant may be tipped bodily towards the distal in an effort to avoid these two structures. The four implant supported fixed prosthesis in the fully edentulous situation has been demonstrated so many times that I think it is patently ridiculous to suggest that this is not the minimum number of implants.
“Clinicians decide what brand of implant they use, how well documented their implant of choice has been for similar applications, the alloy that the implant is made from, the type of the definitive restoration or a myriad of other factors all go into the decision-making process.”
This does not mean that you cannot place more than four. Some clinicians like to segment their definitive prosthesis but, if they are segmenting, the additional implants are being placed in an effort to ensure against a complication, implant loss, which occurs about 5% of the time or less (remember that the article that this was based upon had an implant survival rate of over 98%). If segmenting is preferred then the question of how many implants are necessary to fully mitigate risk? I think that last provision, accepting no complications under any circumstances, is impossible to fulfill. To absolutely minimize that amount you would need three implants in each posterior sextant and four implants across the anterior sextant. Although it is still possible that a patient with these 10 implants could still experience a complication the likelihood of this would be quite low. The question comes down to whether an individual wishes to place four implants with a small risk or 7 to 10 implants with a smaller risk.
Of course the comments above refer to standard diameter implants. The observations with narrow diameter implants have been favorable however one risk that is rarely discussed is the risk of implant fracture. The risk of implant fracture with narrow diameter implants is certainly greater than the risk would be with standard or wide diameter implants. The risk of implant fracture, in my experience, is 0.2% in the full arch situation. (2)
The clinician is responsible for making appropriate decisions. Clinicians decide what brand of implant they use, how well documented their implant of choice has been for similar applications, the alloy that the implant is made from, the type of the definitive restoration or a myriad of other factors all go into the decision-making process. (3) I think it's the clinician's personal responsibility to select the appropriate implant to be used in the specific situation. Who else would be better able to make this decision?
In your opinion, which factors that may facilitate the success of immediate loading?
Branemark told us years ago that osseointegration depended upon the host, the biomaterial, the surgery and the prosthesis. These factors have never changed. The clinician must still consider each of these factors. Other things need to be considered. When considering immediate loading, the micromotion of the implant within bone is critical. There is an amount of motion that is to be considered as sacrosanct. Unfortunately there is no specific way to identify the amount of micro-motion that would be allowed for any dental implant in any different patient. The less micro-motion that is present will likely be better but in the absence of any micro-motion there will be no stimulus to the implants within the bone and this lack of stimulation may present a different risk. One way to reduce micro-motion is by providing rigid splinting of implants, this may be done with the fixed, full arch implant retained prosthesis.(1)
Are there any questions regarding immediate full arch restoration that remain unanswered for you after completing the study?
Of course there are unanswered questions. Sadly it would take years to identify them all.