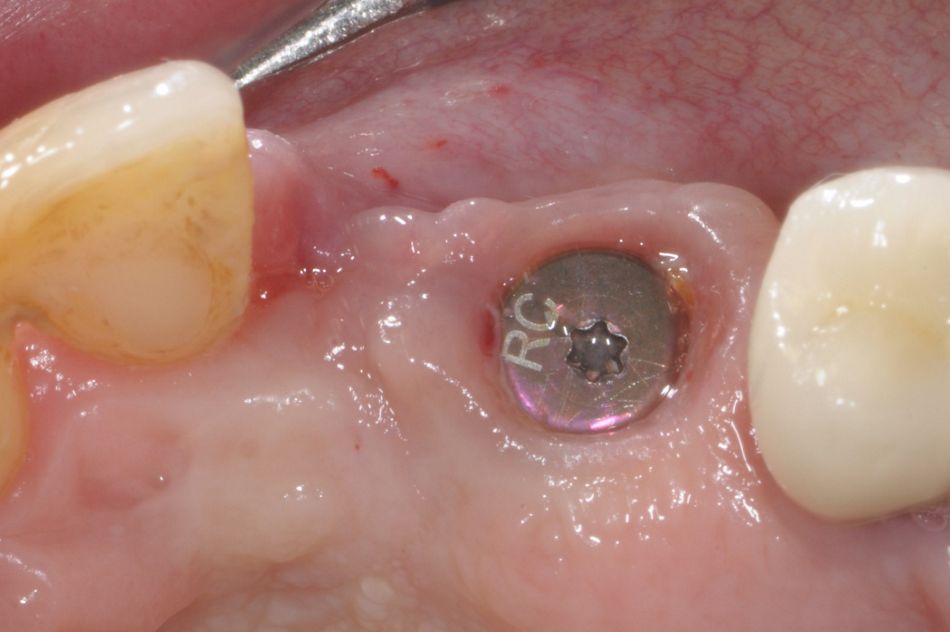
This case describes a prosthetic restoration in the area of the lateral maxillary incisor by means of the Straumann® Bone Level/Bone Level Tapered implants with SLActive® surface. Furthermore, bone and connecting tissue grafting procedures were applied to ensure an appropriate implant performance and to achieve an excellent esthetic result.
Initial situation
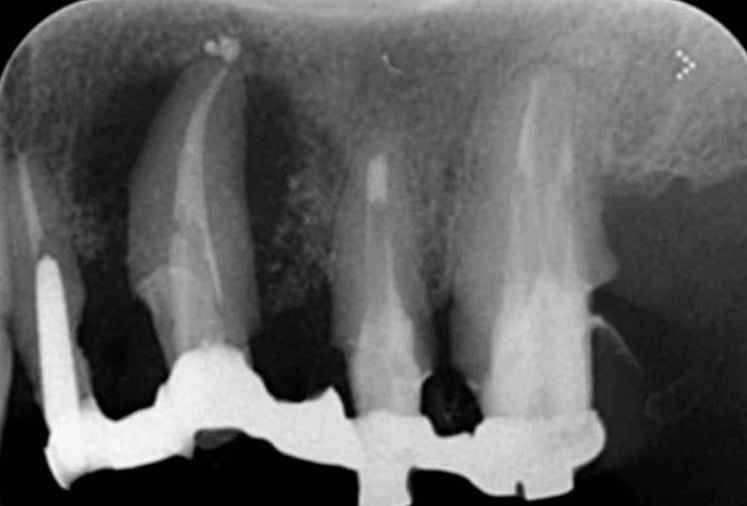
In July 2012, a 52-year-old, non-smoking female patient came for a consultation regarding her periodontal status of her left maxillary area (Fig. 1). She reported pain and frequent abscesses and expressed the desire to improve her esthetics and function. The patient presented several periodontal problems, including multiple gingival recessions and a non-plaque-related mucosal disorder. A thorough analysis was carried out and, following the initial periodontal treatment, the patient gave her informed consent for the extraction of 2.2 and 2.3, which were considered not worth treating.
Treatment planning
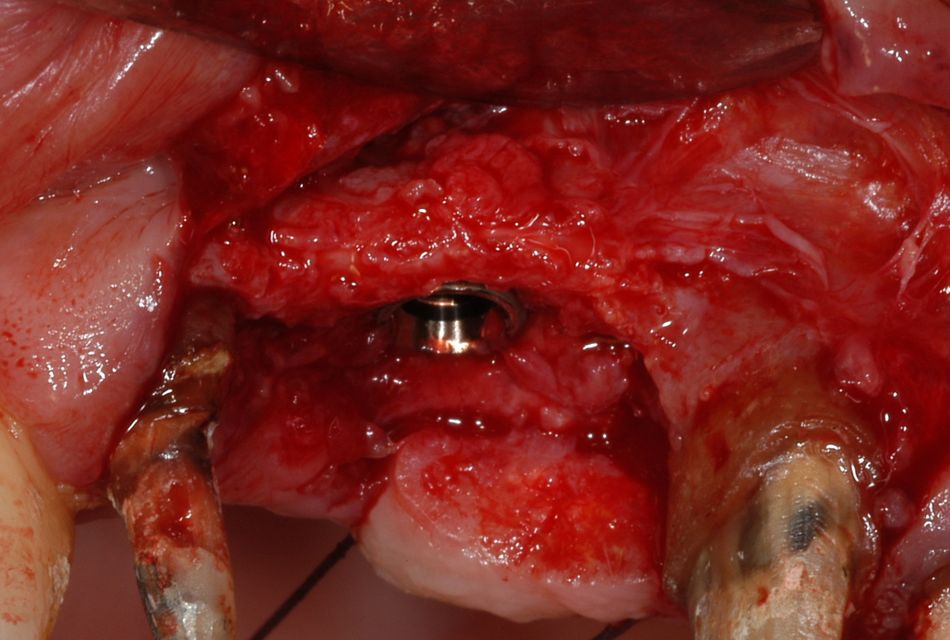
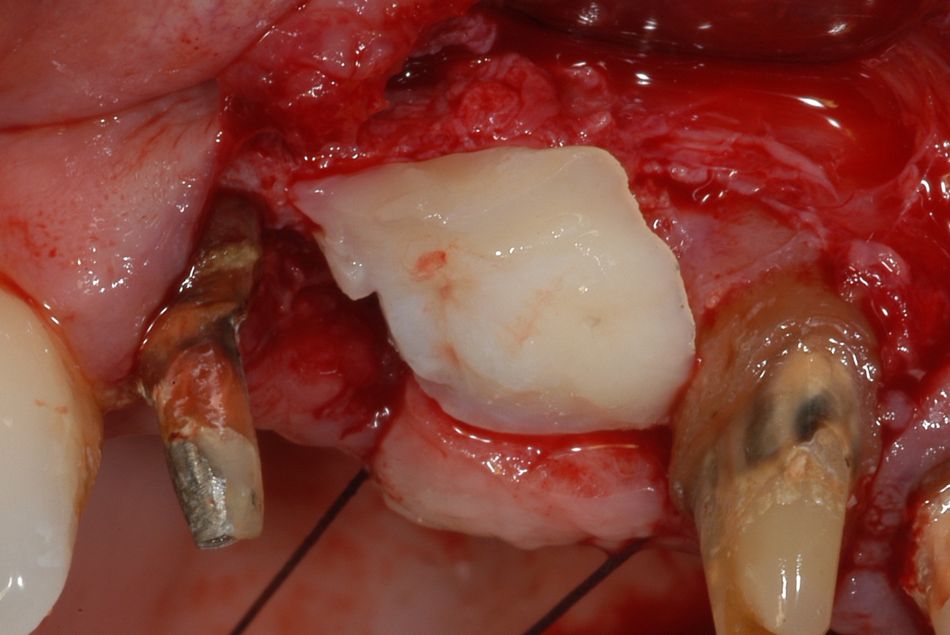
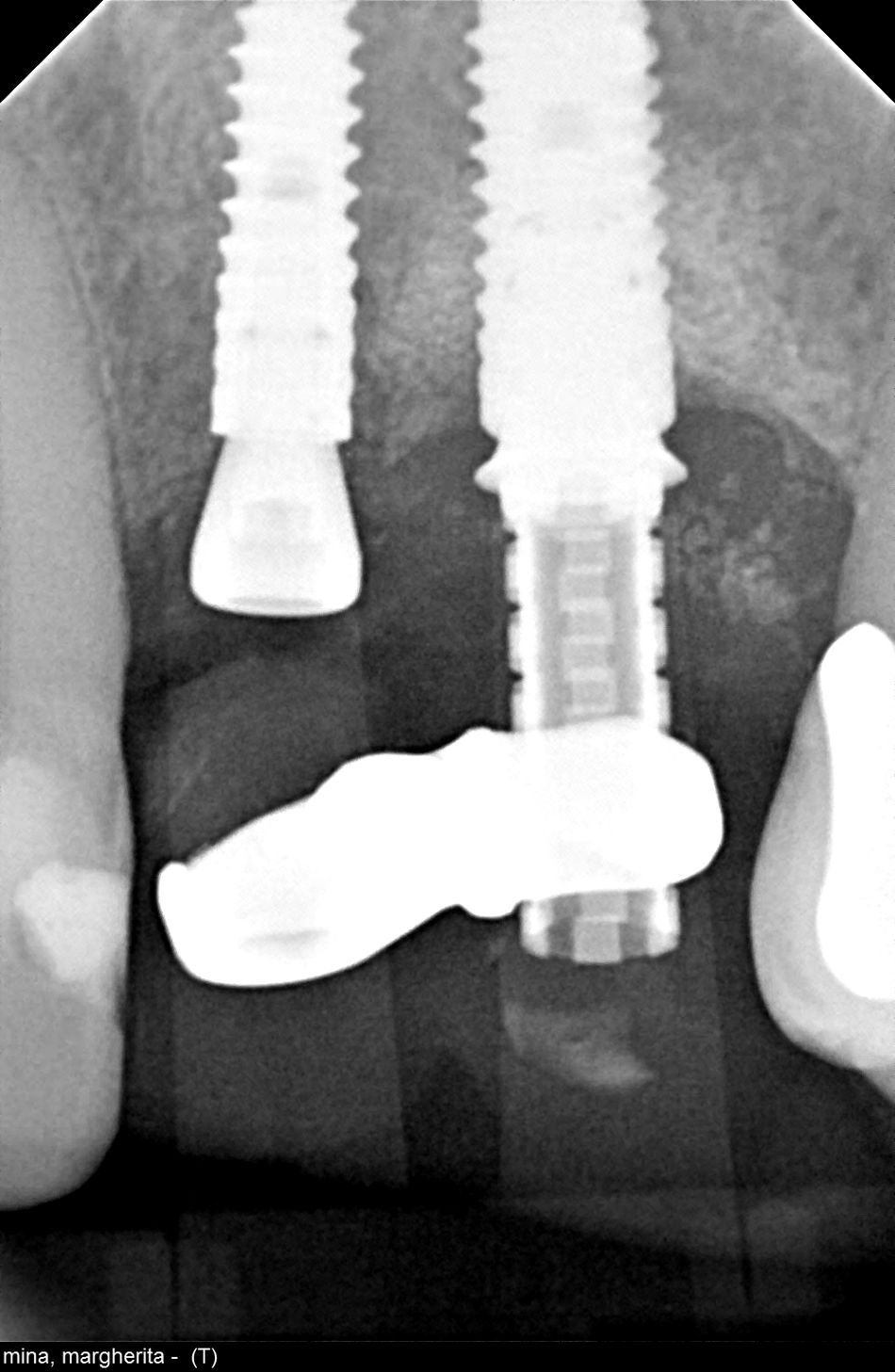
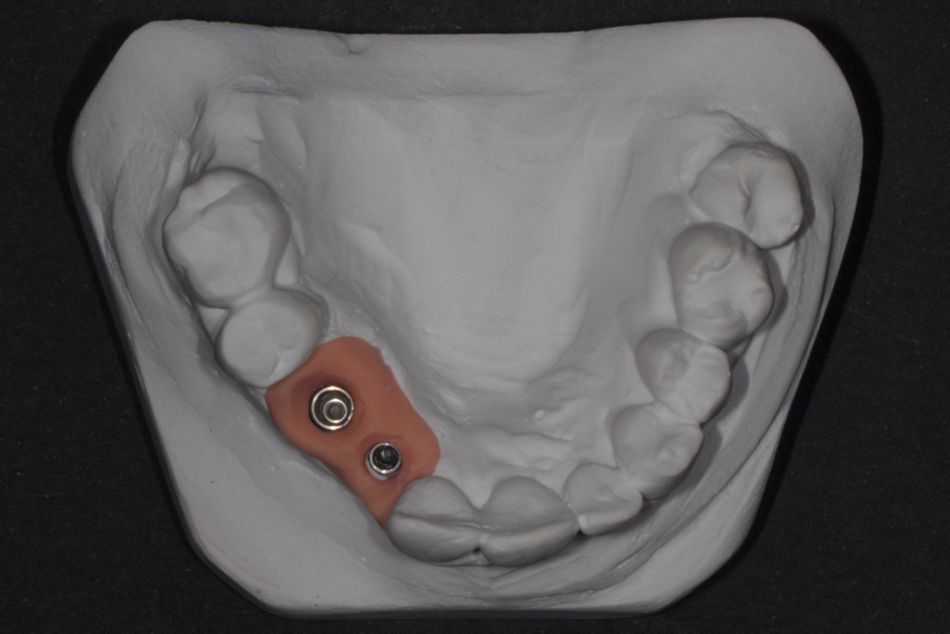
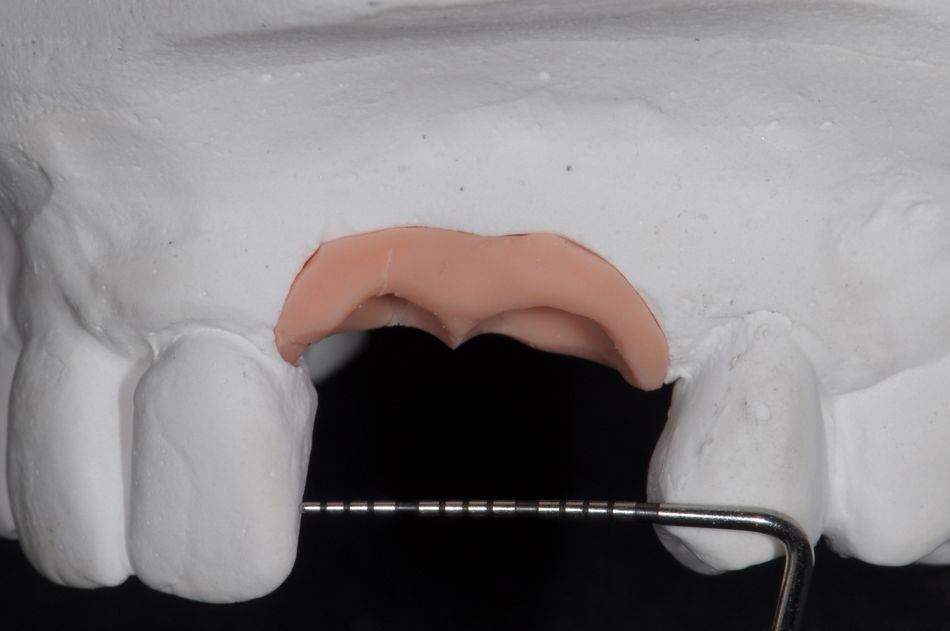
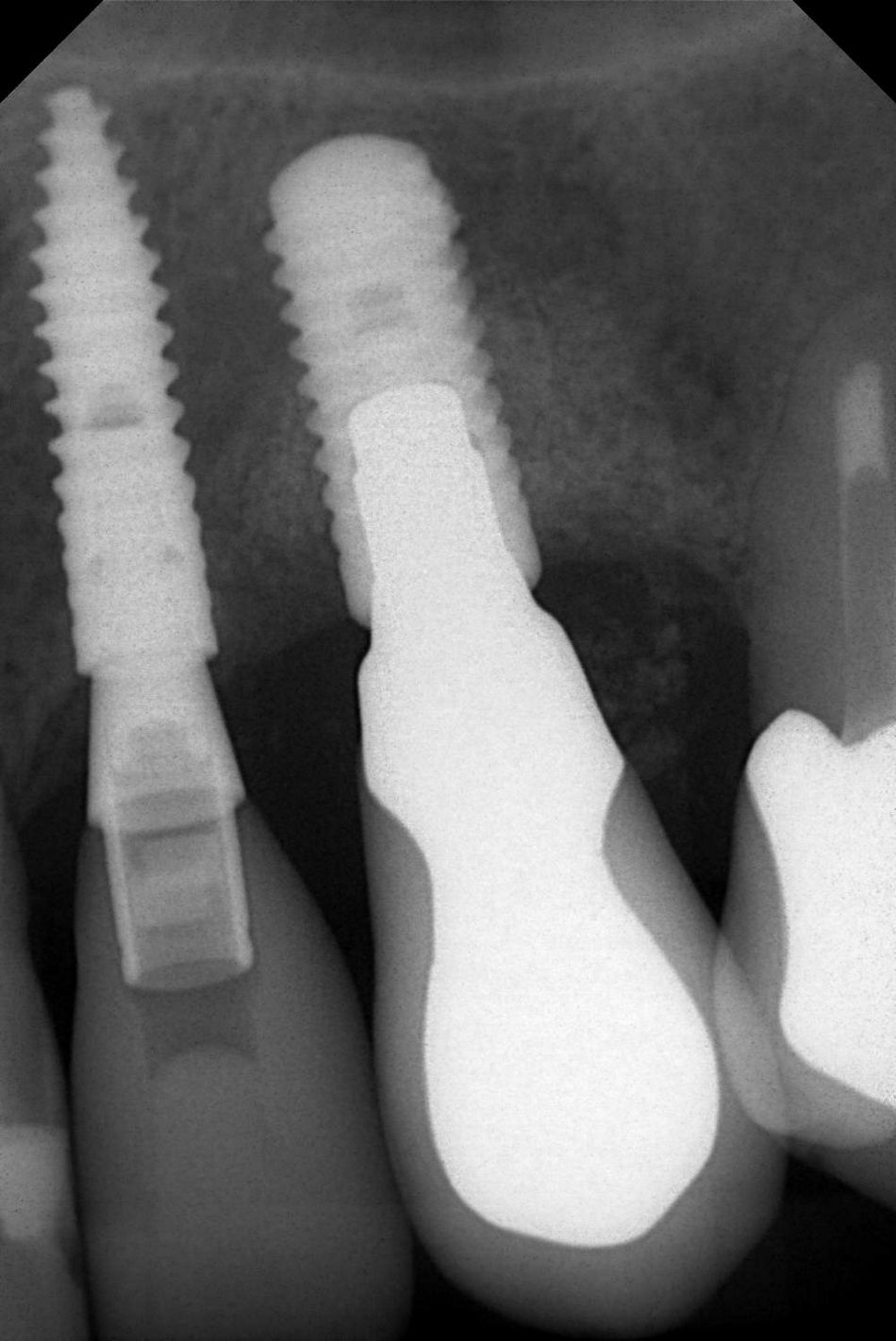
In order to minimize the discomfort during treatment, a step-by-step treatment was requested. The first task was to extract the canine, which was surrounded by a large radiolucent area (Fig. 2). Twelve weeks later, a substantial reduction in the horizontal and vertical dimensions of the crest was evident. The upper left lateral incisor was temporarily left in place to facilitate the positioning of a fixed provisional restoration (Fig. 3).
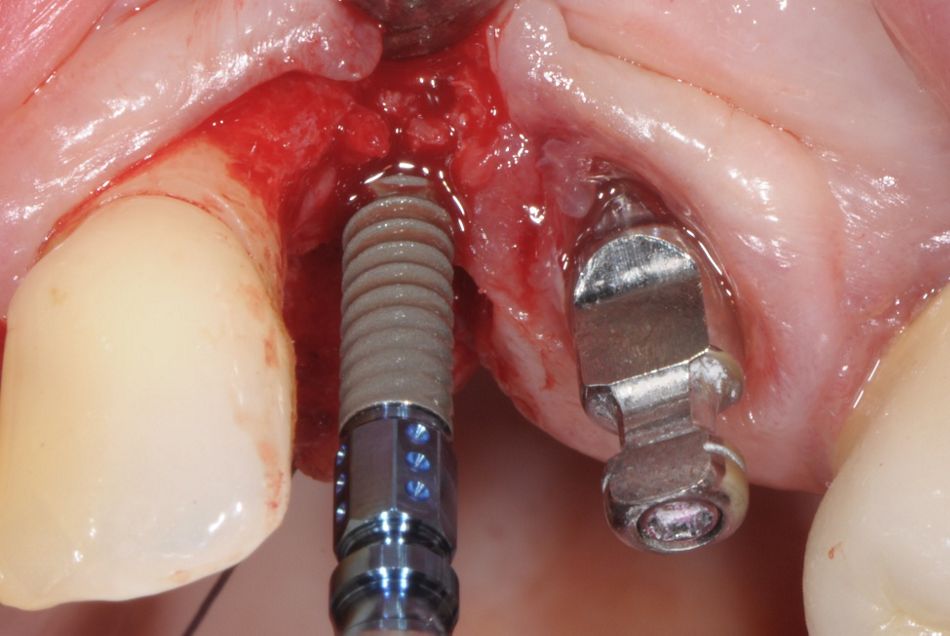
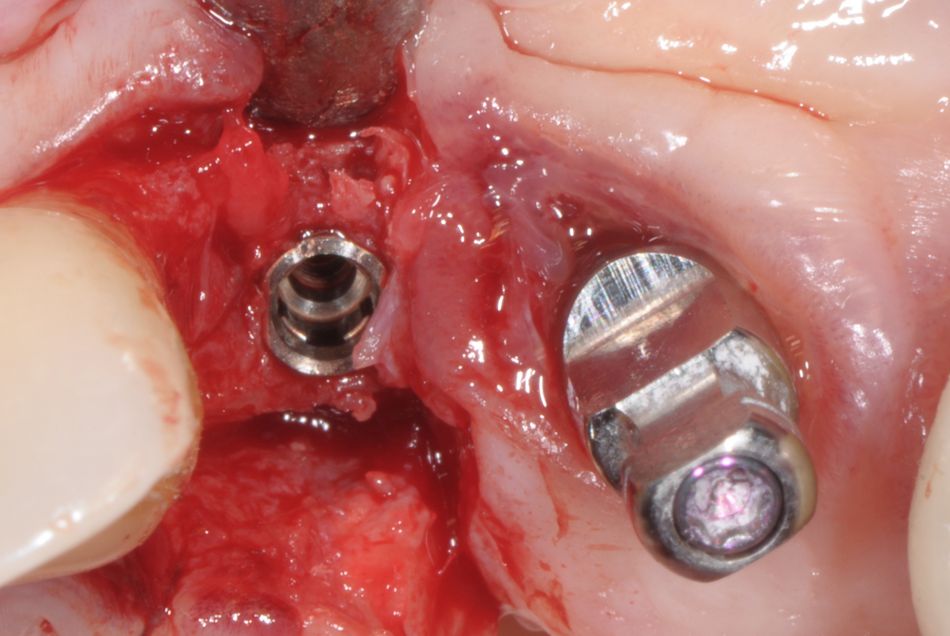
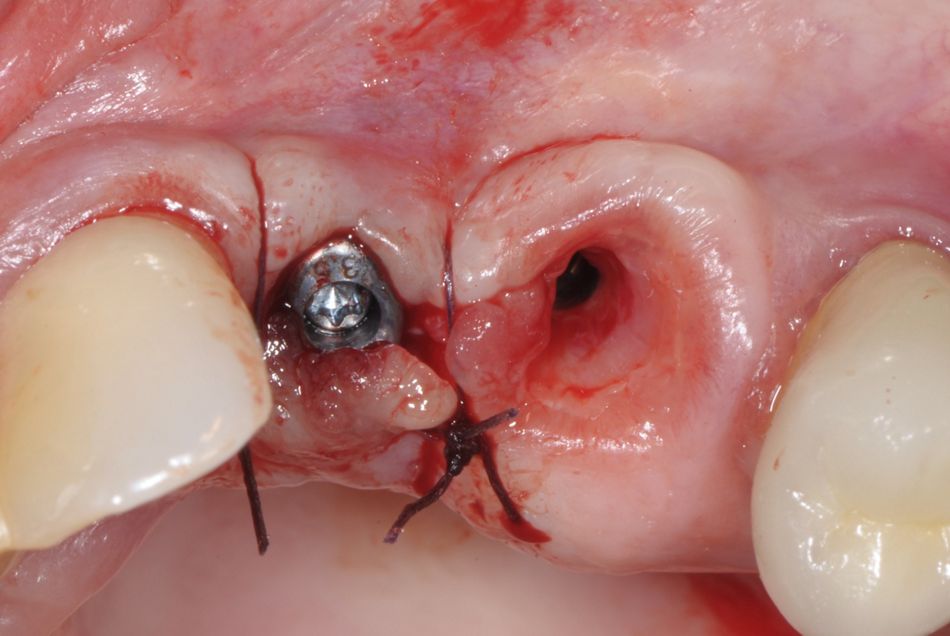
Surgical procedure