
Prof. Dr. Dr. Daniel Rothamel
(Bethesda Clinic, Mönchengladbach, and University of Düsseldorf, Germany)
Why have collagen membranes emerged as state-of-the-art for guided bone regeneration?
Collagen membranes have shown both excellent bone formation and success rates. This relates to smaller and larger bone augmentation volumes (1), including dehiscence defects around implants and sinus floor augmentation (2). Collagen membranes provide an excellent scaffold for both nutrition transfer and barrier function. In addition, they permit secondary healing even in case of membrane exposure. Complications in case of exposure is the most significant disadvantage of non-absorbable membranes. Collagen membranes are easy to use – and therefore a valuable tool for daily augmentation procedures.
“The Jason®’s extended barrier function permits bone formation to the outline of the grafted area.” D. Rothamel
What is special about the Jason® membrane? Why does it extend the indication range in comparison with softer and thicker collagen membranes?
The botiss Jason® membrane is a very thin, but tear-resistant membrane derived from porcine pericardium. In the animal, the tissue is exposed to a lot of strain and stress. This has a high impact on the natural morphology and multi-directional orientation of the collagen fibers, which is retained during processing. Just as the more angiogenic membranes derived from porcine dermis (e.g. collprotect® membrane by botiss biomaterials), the Jason® membrane consists of native collagen type I and III (3). It integrates ideally into the tissue and has shown inflammation-free biodegradation (3, 4). This is an important difference to chemically cross-linked collagen membranes: their longer barrier function is based on a biochemical alteration of the collagen matrix, which affects the collagen structure (5).
Last but not least, due to its specific morphology, the Jason® membrane ensures a long barrier function (3). This permits sufficient separation of the cortical and trabecular bone compartments and bone formation extending to the outline of the grafted area. The membrane has a minimal thickness of only approximately 0.15 mm. This makes it easier and less invasive to close the soft tissues after augmentation, especially in comparison to expensive double-layer techniques – which are moreover used with voluminous bilayer membranes.
Histological and clinical pictures

Fig. 1: The Jason® membrane is very thin, while biomechanically strong.
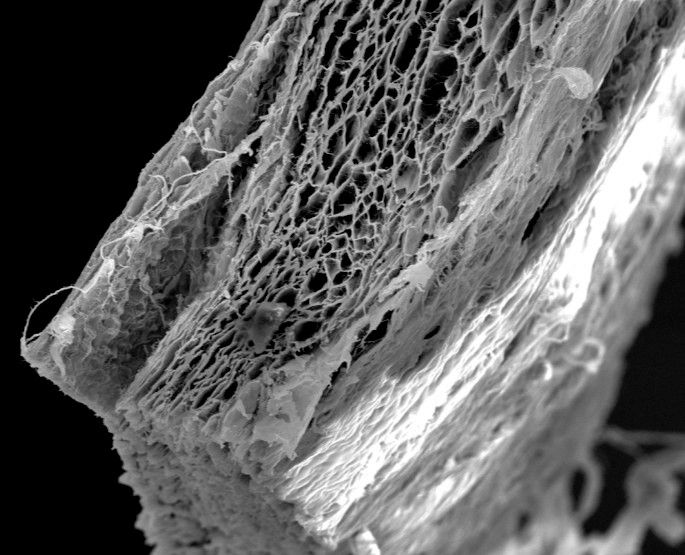
Fig. 2: The Jason® membrane shows a natural porous multi-layered structure, which ensures high biocompatibility.
Sinus augmentation case

Fig. 3: After preparation of the lateral sinus window, a customized portion of the dry Jason® membrane is inserted into the cavity.
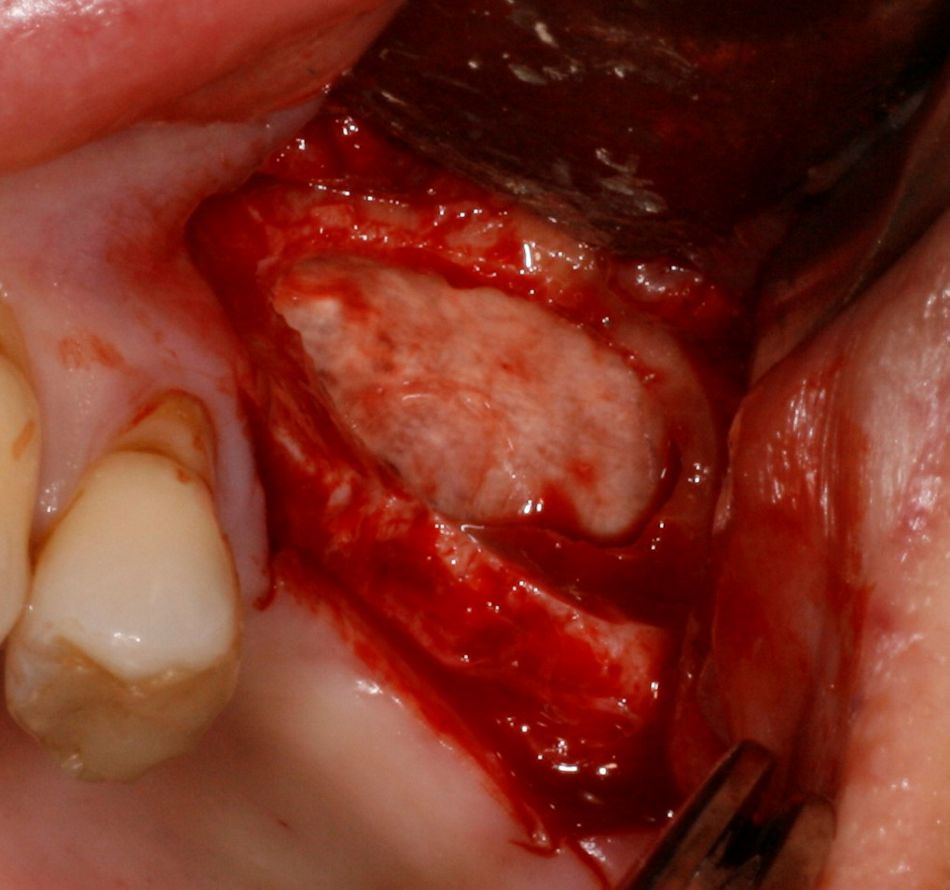
Fig. 4: The re-hydrated membrane protects the Schneiderian membrane prior to the placement of graft material.
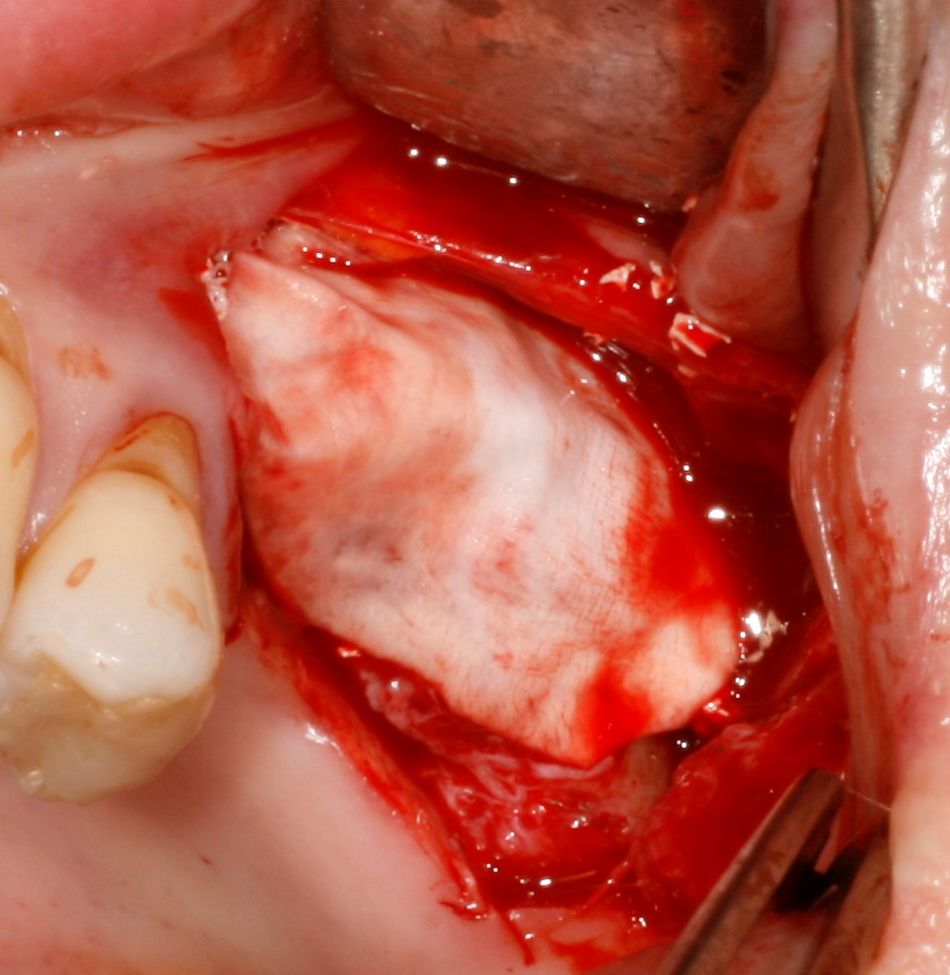
Fig. 5: After application of the bone substitute material for both sinus augmentation and lateral augmentation, a second Jason® membrane is placed on the graft for long-term separation from the soft tissue.

Dr. Michael Kristensen
(Aarhus Tandcenter, Denmark)
You are a confessing user of the Jason® membrane. Why do you prefer this product?
I am a big fan of this membrane: the handling is easy – it can be pinned – it´s stretchable – sizes are good. Most importantly, its slower degradation gives me better bone augmentation results than any other absorbable membrane I know.
For which indications do you use the Jason® membrane in your practice?
I use the Jason® membrane as the only membrane. I use it for every single bone augmentation procedure I do in my practice – which are about one hundred cases a year. First of all, I use it for guided bone regeneration procedures around implants. Another frequent indication are bone augmentations prior to implant placement. This could be in combination with autogenous bone particles or blocks, or with botiss maxgraft® bonebuilder. I also utilize the Jason® membrane for sinus grafting: to close the lateral window, or to repair injuries of the Schneiderian Membrane. In the latter cases, the Jason® membrane attaches to the surrounding tissue and repairs the rupture or perforation very well (6).
“I use the Jason® for every single bone augmentation procedure I do in my practice – which are about one hundred cases a year.” M. Kristensen
Do you prefer to pin or suture the membrane?
I always pin the membrane nowadays – I find it easier and faster than suturing. Pinning, combined with the Jason’s stretchability, allows me to "overfill" the augmented area. This so-called sausage technique leads to a bigger volume, which is also more stable over time. In my experience, if we don't stabilize the membrane by pinning or suturing, the membrane and augmentation can move during healing. This, in turn, can result in a loss of particulate augmentation material, or to fibrous healing.
Clinical pictures, GBR small
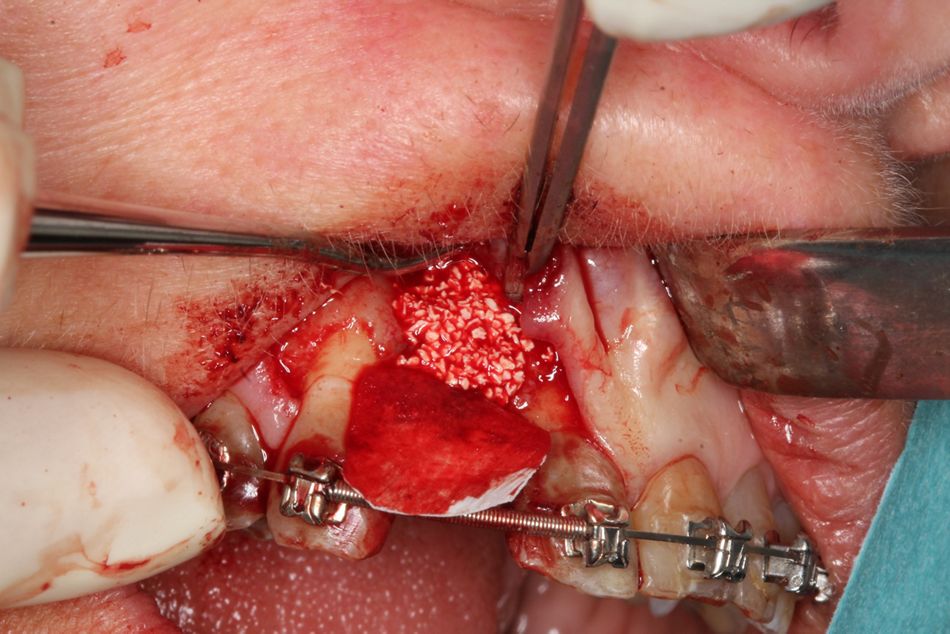
Fig. 6: The Jason® membrane can be used for all augmentations, including small GBR procedures (case by Dr. Michael Kristensen).
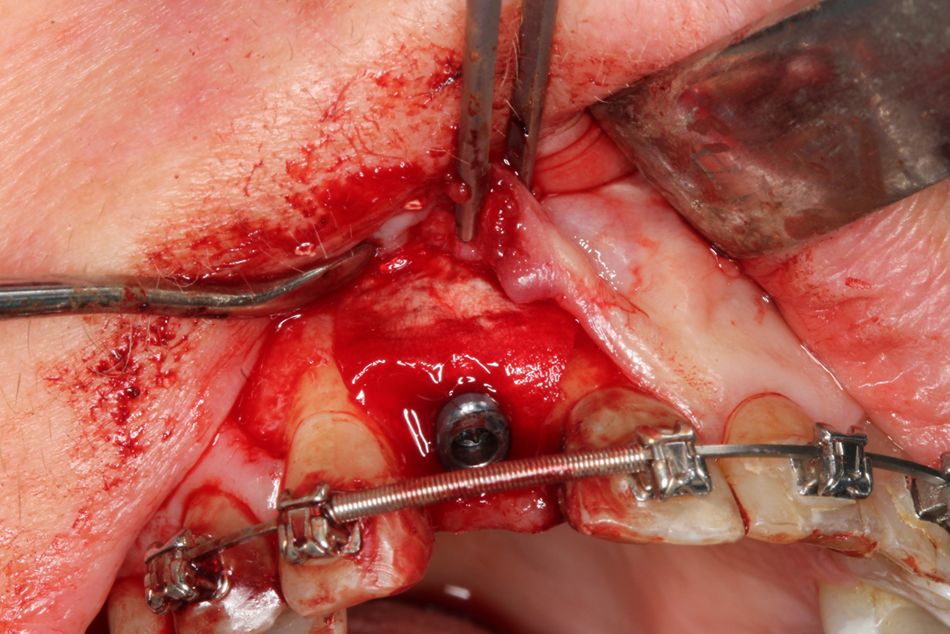
Fig. 7: In these situations, due to the membrane’s excellent adhesion to tissues, pinning may not be necessary. The coronal part of the membrane has been fixed with the implant screw.

Dr. Massimo Frosecchi
(Studio Odontoiatrico, Firenze, Italy)
You like to use the Jason® membrane in practically all clinical situations. For which reasons?
The use of a membrane is normally indicated in connection with bone substitute materials. An extended barrier function is often necessary to maintain volume and promote substantial bone regeneration, especially in large augmented areas. The specific structure of the Jason® membrane ensures the desired barrier effect and presents a favorable handling.
Do you have any favorite indications?
My favorite indications are all GBR cases, especially when the membrane has to be fixed with pins. Another frequent indication in my practice is the final coverage of lateral osteotomies after lateral sinus augmentation (2). Because of its minimal thickness, the Jason® membrane has also proven very helpful in thin phenotypes.
“Because of its minimal thickness, the Jason membrane has also proven very helpful in thin phenotypes.” M. Frosecchi
How should the membrane be used?
My suggestion is to re-hydrate the Jason® membrane after shaping and use it wet in the recipient site. For rehydration saline solution or blood can be used. This can also be performed after placement of the membrane, but this may not be optimal due to its relative rigidity. Fixation with pins is very easy, and it ensures the desirable stability and volume maintenance.
Clinical pictures: GBR large
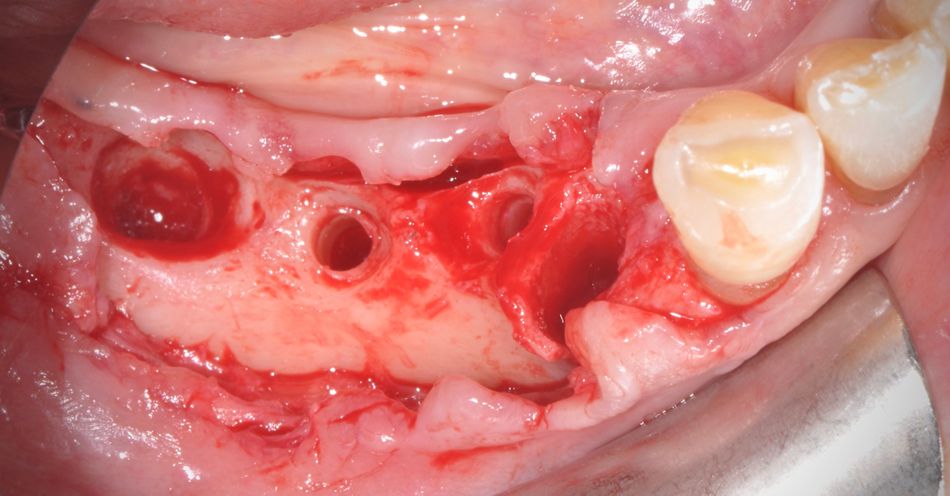
Fig. 8: Due to its elasticity and strength, the Jason® membrane shows special benefits in large augmentation procedures (case by Dr. Massimo Frosecchi).
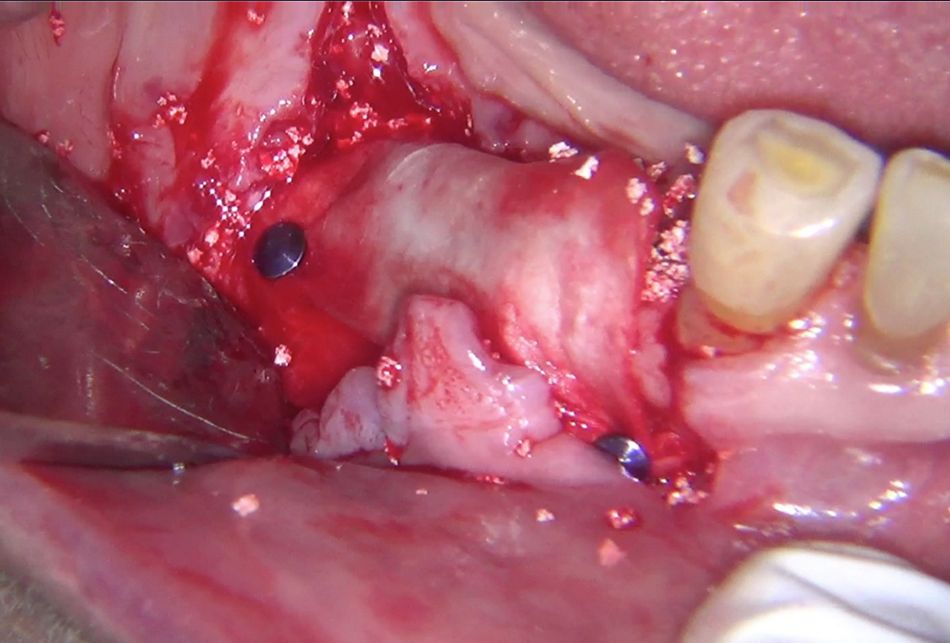
Fig. 9: The membrane was used in combination with botiss maxresorb®, mixed with autogenic bone.
Clinical picture, ridge preservation (Dr. Damir Jelušić)
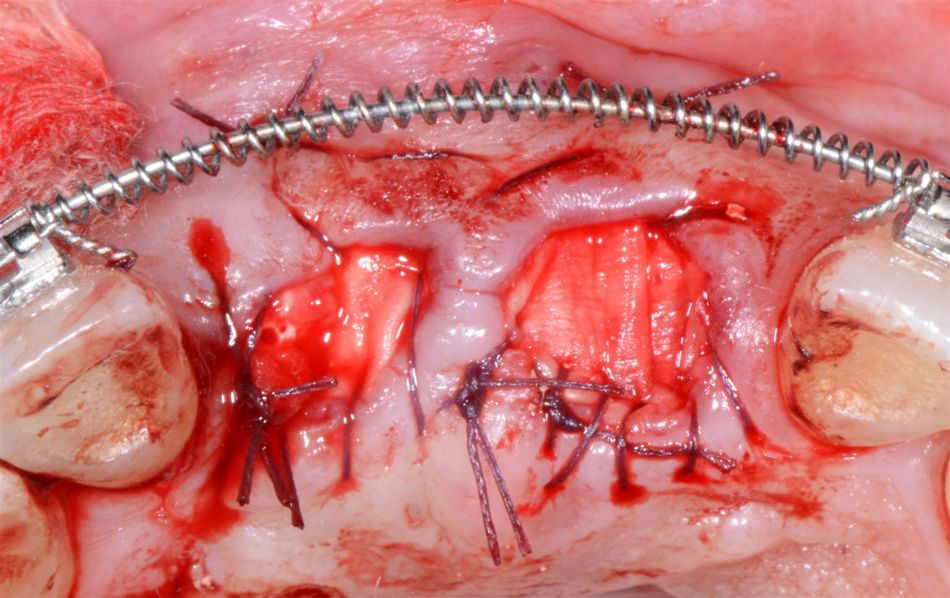
Fig. 10: The Jason® membrane is also indicated for ridge preservation procedures (case by Dr. Damir Jelušić, Opatija, Croatia).
For further information on the botiss Jason® membrane: see here or contact your local sales representative.


