Introduction
Peri-implantitis remains one of the most challenging biological complications in implant dentistry, particularly in patients with a history of periodontitis. Effective decontamination of the implant surface is critical to the successful management of this condition. Traditional mechanical and chemical methods often fall short in completely eliminating the biofilm from the complex microstructure of implant surfaces, especially in advanced cases.
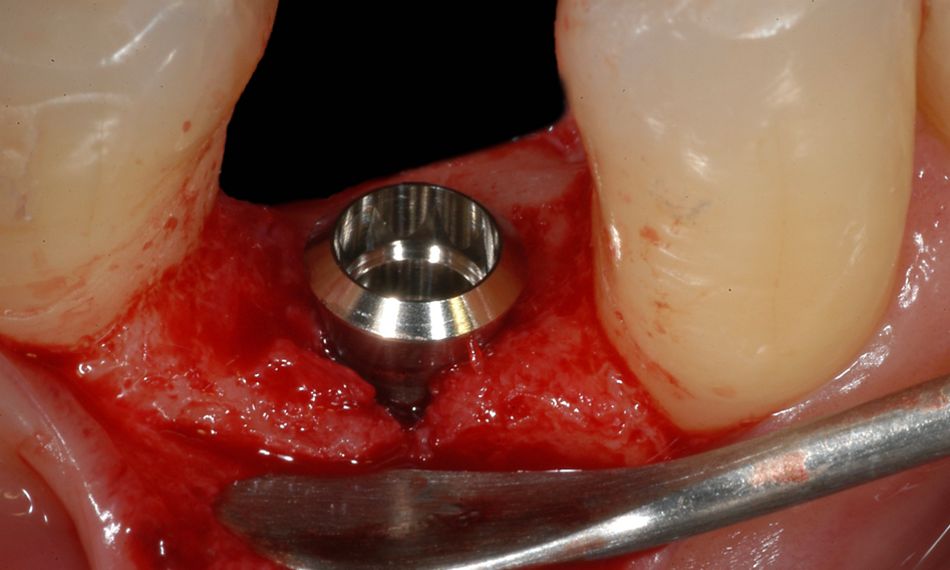
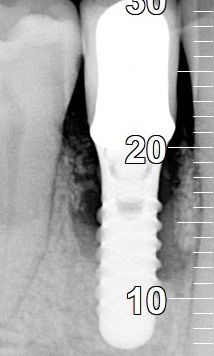
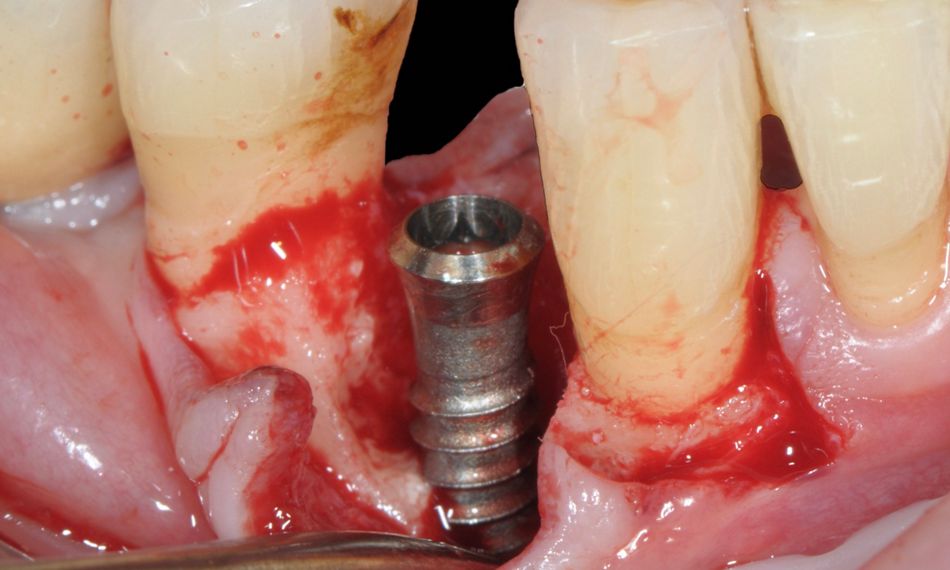
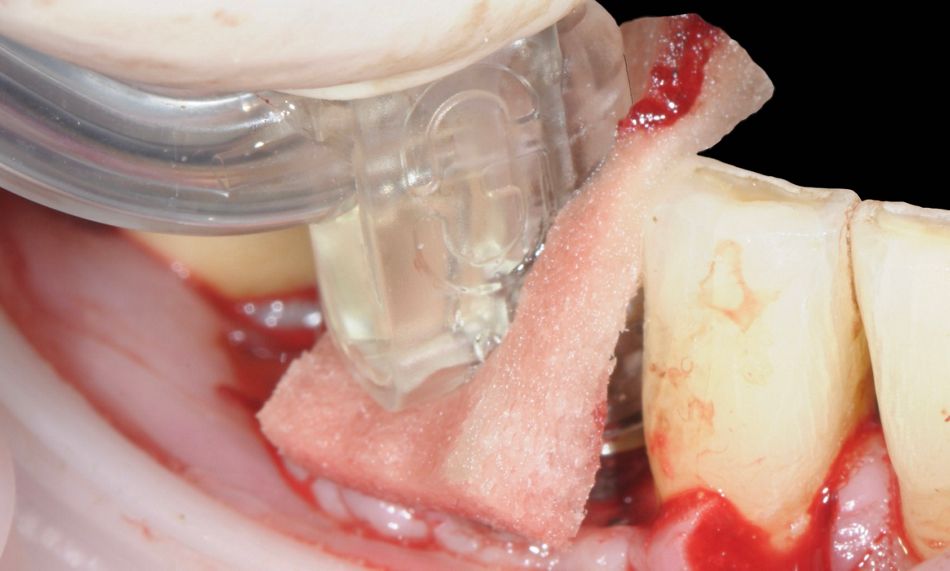
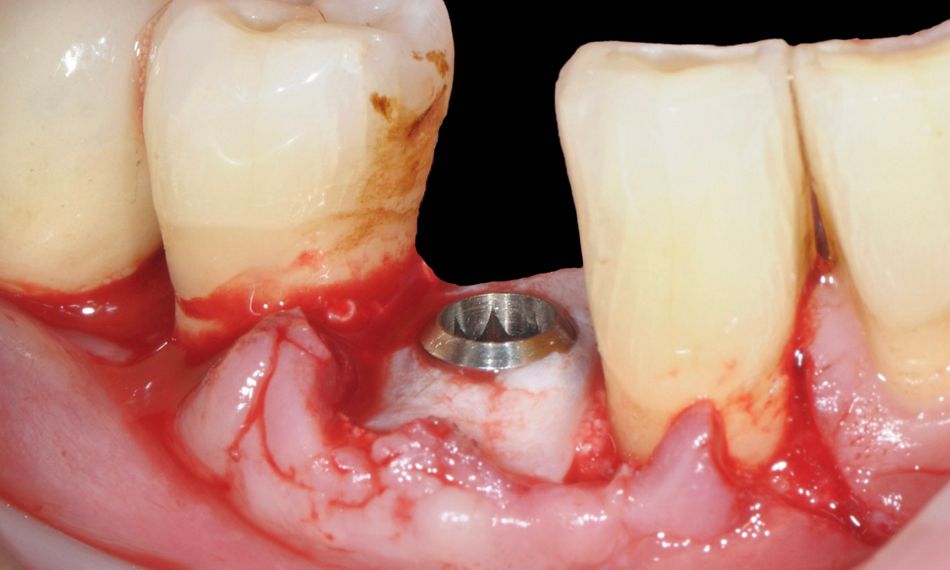
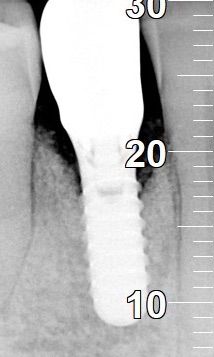
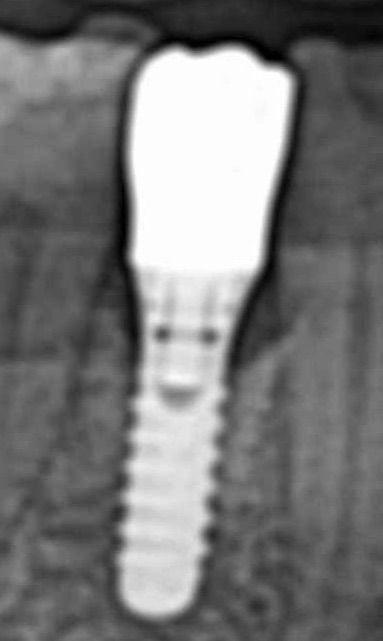
GalvoSurge®, an electrolytic cleaning system, offers a novel and minimally invasive approach by generating hydrogen bubbles that physically lift biofilm and bacterial contaminants from the implant surface without damaging the titanium. This case report describes the successful management of peri-implantitis in a high-risk patient with a documented history of severe generalized periodontitis. Remarkably, the peri-implantitis developed 16 years after implant placement, emphasizing the need for long-term monitoring and effective treatment strategies in vulnerable patients.
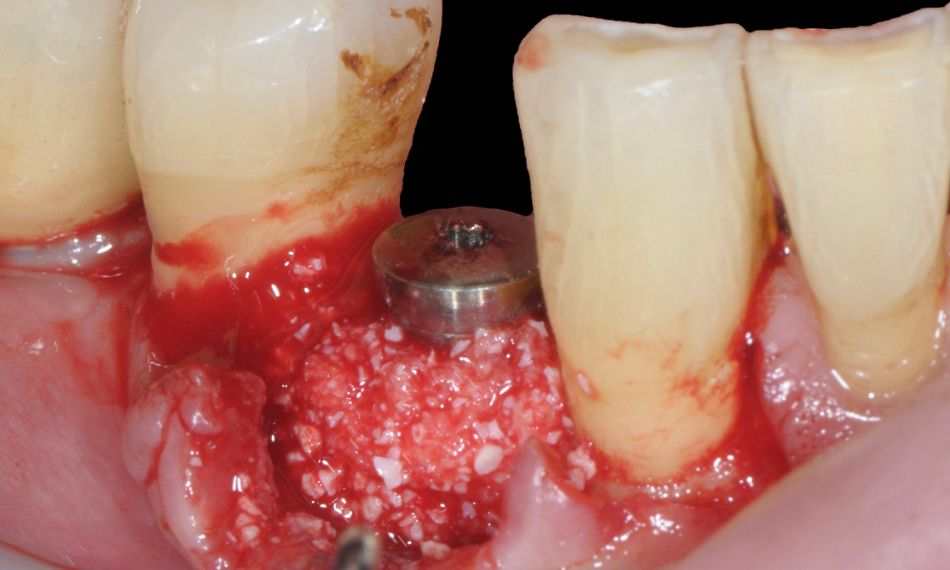
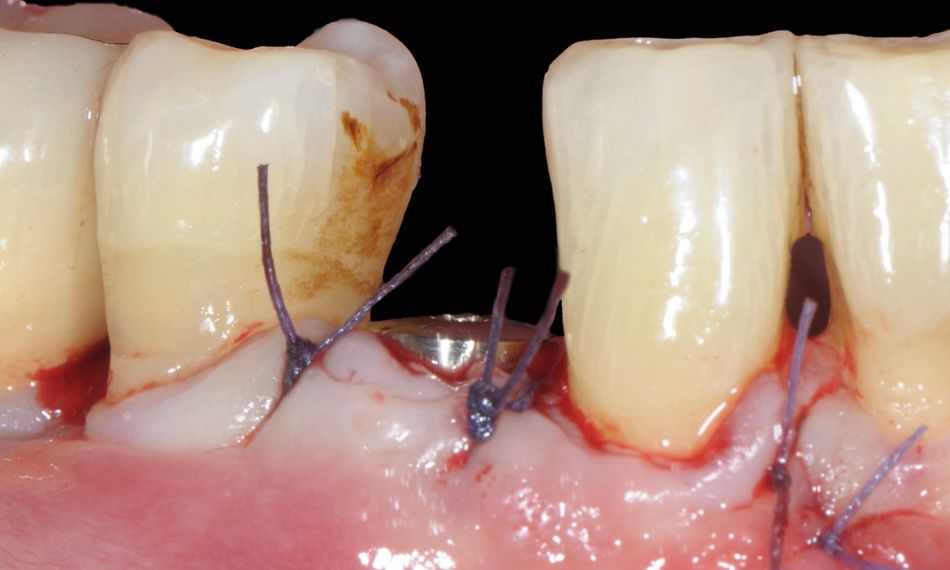
The case highlights the pivotal role of electrolytic decontamination with GalvoSurge®, combined with guided bone regeneration (GBR) and personalized supportive care, in achieving soft and hard tissue stability around an implant affected by advanced peri-implantitis.
Initial situation
A 46-year-old male non-smoking patient with a diagnosis of severe generalized periodontitis was referred to our practice in January 2002 for an integral dental treatment. The patient was initially professionally treated by scaling and root planing in order to obtain infection control. In addition, personalized oral hygiene instructions were given to ensure proper domiciliary plaque control. After the assurance of good motivation and compliance (FMPS < 20%; FMBS < 20%), the patient was prepared for the surgical phase.
The surgical phase included guided tissue regeneration with amelogenin (Straumann® Emdogain®) in locations where deep periodontal infrabony defects were present.
Nine months after the surgical phase, an orthodontic treatment, aiming at correcting malposition, creating contact points, and giving a non-traumatic occlusion, was initiated.
After completion of the active orthodontic therapy, the patient was placed on an individually tailored maintenance care program, including continuous evaluation of the occurrence and the risk of disease progression. In addition, motivation, reinstruction, instrumentation, and treatment of re-infected sites were performed as needed.