- Learn how regenerative strategies can preserve dental implants affected by peri-implantitis
- Discover the role of the GalvoSurge® system in biofilm decontamination
- Explore step-by-step treatment decisions that restored esthetics and function
Introduction
Peri-implantitis is a biologically driven inflammatory condition characterized by progressive bone loss around osseointegrated implants. If not treated effectively, it can ultimately lead to implant failure. The management of peri-implantitis presents a clinical challenge, particularly when patients express a strong preference for implant retention and when implant removal would entail significant functional or esthetic compromise.
This report describes the case of a 45-year-old male patient who presented with peri-implantitis at tooth #11, affecting a 1.5-year-old implant. The patient was medically healthy, a non-smoker, and expressed a clear desire to preserve the implant. Given the absence of systemic risk factors and the localized nature of the defect, a regenerative approach was considered appropriate.
Central to the treatment protocol was the use of the GalvoSurge® Dental Implant Cleaning System, which employs electrochemical cleaning to remove biofilm from contaminated implant surfaces. This method allows for in situ decontamination without altering the implant microstructure, making it particularly suitable for regenerative procedures. In this case, GalvoSurge® was used in conjunction with guided bone regeneration and a connective tissue graft to restore peri-implant health and soft tissue volume.
This case report outlines the diagnostic findings, clinical decision-making, and stepwise treatment protocol. It demonstrates how a combination of advanced decontamination and regenerative techniques can facilitate successful implant preservation in cases of peri-implantitis with favorable local and systemic conditions.
Initial situation
A 45-year-old male patient referred for treatment of peri-implantitis presented with recurrent inflammation, bleeding, and discomfort around the implant at tooth #11. His primary concern prioritized health over esthetics, with a strong desire to preserve the 1.5-year-old implant, even though full bone regeneration was not expected due to the implant position. He had no identifiable risk factors such as systemic diseases or smoking. His dental history included generalized stage III, grade C periodontitis, and extraction of tooth #11 due to a root fracture, followed by immediate implant placement and provisionalization (Fig. 1).
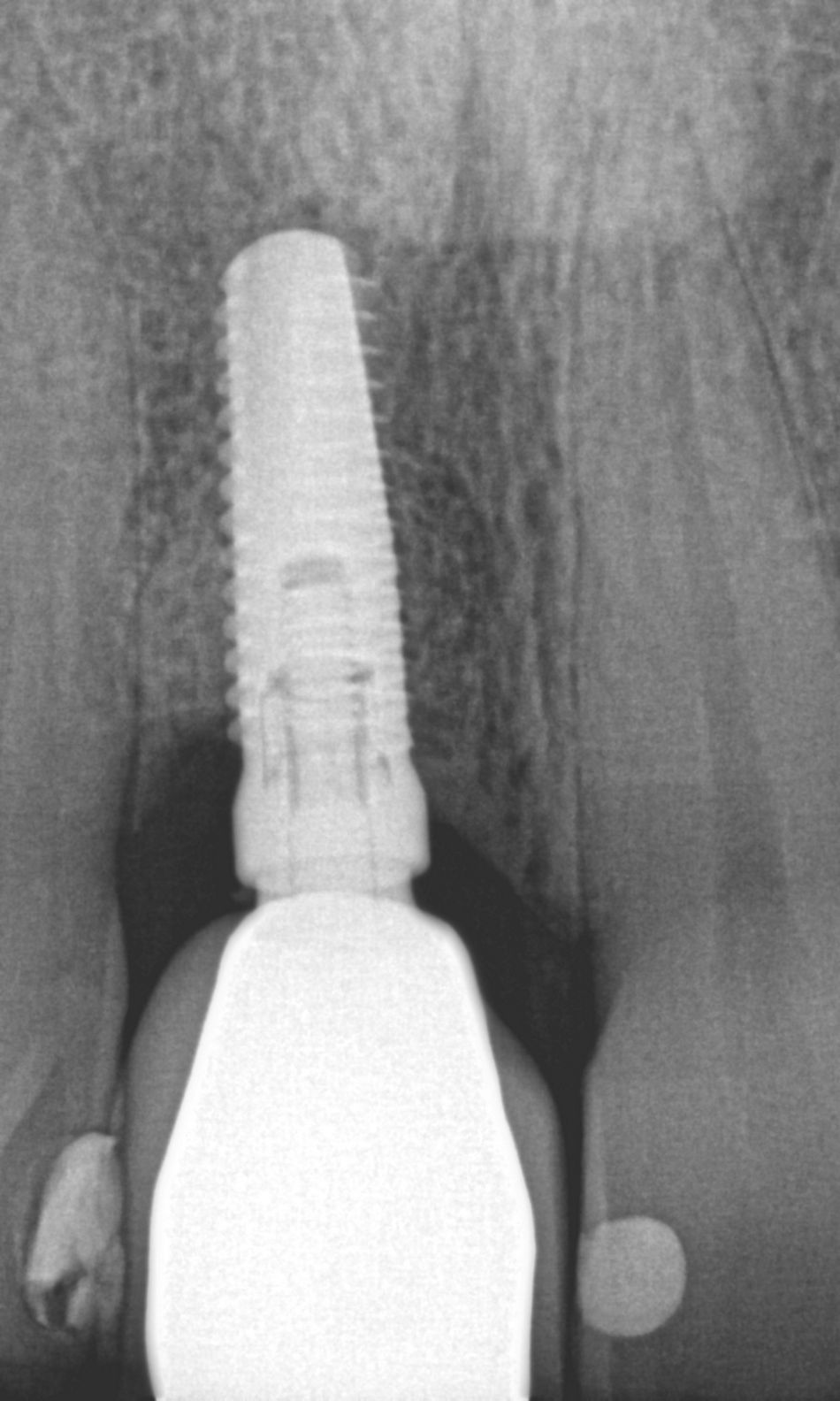
Radiographic analysis showed horizontal bone loss on neighboring teeth, particularly mesially on tooth #12, and a mixed horizontal and crater-like bone defect around the implant, which had been placed too shallowly and buccally (Fig. 2).
The remaining dentition exhibited a favorable overall prognosis. Implant #11 was diagnosed with peri-implantitis but was considered to have a favorable outcome upon successful intervention. Long-term stability would depend on rigorous maintenance protocols, including frequent recall intervals and individualized supportive periodontal therapy.
Treatment planning
Pre-surgical Phase:
- 14 days before: Non-surgical periodontal and peri-implant therapy.
- 3 days before: 0.2% chlorhexidine rinses, 3x/day.
Surgical Phase:
- Local anesthesia.
- The crown was removed, and a digital impression was taken with a scan body for the later provisional.
- Implant decontamination with GalvoSurge®.
- Guided bone regeneration with botiss maxgraft® plus and Jason® membrane.
- Connective tissue graft for soft tissue support.
Provisionalization:
- Immediate: Maryland bridge placement.
- 3 months post-op: Screw-retained zirconia provisional crown.
Prosthetic Phase (Planned):
- Final restoration after further hard and soft tissue maturation by the referring dentist.
Surgical procedure
Fourteen days prior to surgery, the patient underwent non-surgical periodontal therapy, including mechanical debridement and subgingival instrumentation with ultrasonic and hand instruments, aimed at reducing local microbial load and gingival inflammation. This pre-surgical phase was essential to optimize the peri-implant soft tissue environment and support a more predictable surgical outcome.
Three days before the surgical intervention, the patient was instructed to begin using 0.2% chlorhexidine digluconate mouth rinses three times daily. The use of chlorhexidine served as a chemical adjunct to reduce bacterial colonization and ensure a cleaner surgical field. Oral hygiene instructions were reinforced, and the patient demonstrated excellent compliance during the preparatory phase.
On the day of surgery, local anesthesia was achieved using articaine with epinephrine to ensure adequate pain control and hemostasis. The crown was removed, and a digital impression was taken with a scan body for the later provisional. The patient desired a very esthetic temporary prosthesis (Figs. 3-8).
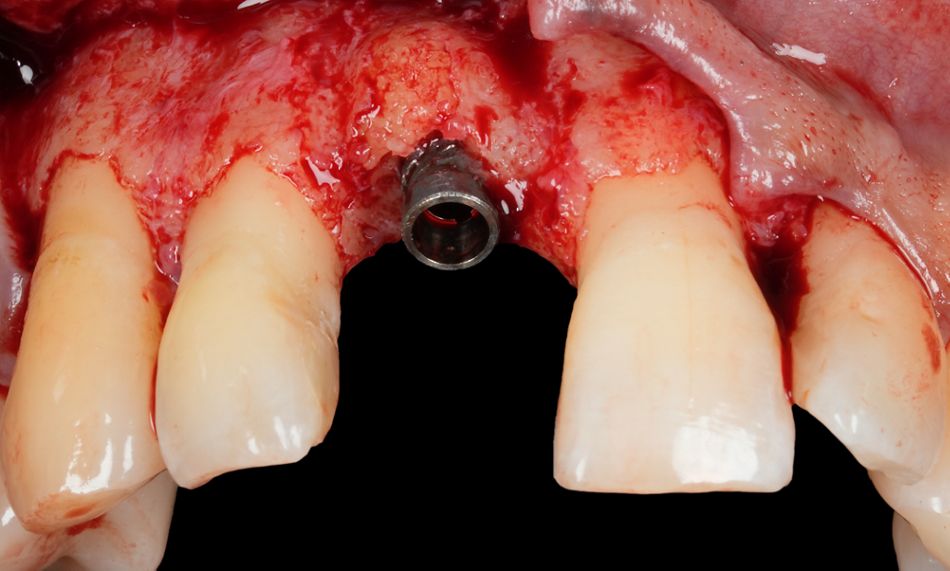
A full-thickness mucoperiosteal flap was elevated to expose the affected implant and the surrounding bone defect. The clinical examination confirmed the presence of a mixed horizontal and crater-like peri-implant bone defect, as previously noted on radiographs (Fig. 9).
The exposed implant surface was thoroughly decontaminated using the GalvoSurge® Dental Implant Cleaning System. This electrochemical cleaning technique operates by generating hydrogen bubbles at the implant surface, which mechanically lift and detach biofilm and other contaminants without damaging the titanium microstructure. The process allows for an effective and atraumatic surface decontamination, creating a favorable environment for potential re-osseointegration and regenerative healing (Figs. 10-12).
Following decontamination, guided bone regeneration (GBR) was performed to correct the bone defect. A particulate allograft material, botiss maxgraft® plus, was used to fill the defect, providing osteoconductive scaffold properties. The grafted area was then covered with a resorbable collagen membrane, Jason® membrane, to stabilize the graft material and promote selective cell repopulation while preventing soft tissue invasion into the graft site (Figs. 13,14).
To further enhance the soft tissue profile and improve long-term peri-implant tissue stability, a connective tissue graft was harvested and placed over the augmented site. This graft contributed to an increase in mucosal thickness and supported wound closure, promoting favorable esthetic and functional outcomes (Figs. 15-17).
The surgical site was carefully sutured to achieve primary closure with tension-free adaptation of the flap. Postoperative care instructions were provided, and a control periapical X-ray was taken. The patient was scheduled for close follow-up to monitor healing progress (Figs. 18-20).
Immediately after surgery, a Maryland bridge was placed as a temporary restoration.
Prosthetic procedure
Two weeks later, the sutures were removed, and wound healing was satisfactory (Fig. 21).
Three months postoperatively, the Maryland bridge was removed. The soft tissue healing was satisfactory (Figs. 22-24).
A screw-retained zirconia provisional crown was delivered. The temporary restorations were milled for optimal fit and esthetics. The provisional was designed in an ideal way based on the digital scan during PI surgery (Figs. 25,26).
The referring dentist placed the definitive crown. The patient was very pleased with the result (Fig. 27)
Treatment outcomes
The treatment protocol led to a marked reduction in periodontal inflammation, attributed to thorough non-surgical therapy and strict oral hygiene measures initiated in the pre-surgical phase. The adjunctive use of 0.2% chlorhexidine rinses prior to surgery effectively reduced the microbial load, contributing to a more favorable surgical environment. Intraoperatively, the implant surface was successfully decontaminated using the GalvoSurge® Dental Implant Cleaning System, enabling thorough removal of biofilm without compromising the implant surface integrity. This was a critical step in minimizing infection risk and facilitating conditions conducive to re-osseointegration.
Guided bone regeneration (GBR) was successfully performed, resulting in stable bone volume around the implant site. The combination of botiss maxgraft® plus and Jason® membrane provided both osteoconductive support and a protective barrier for tissue regeneration. Additionally, the placement of a connective tissue graft enhanced soft tissue thickness, promoting improved mucogingival stability and contributing to a more favorable esthetic outcome in the anterior maxilla.
Functional and esthetic continuity during healing was maintained through immediate provisionalization with a Maryland bridge. Three months postoperatively, a screw-retained zirconia provisional crown was placed, offering both durability and a natural appearance while allowing for continued tissue maturation. The final prosthetic restoration, planned following complete osseointegration and soft tissue stabilization, is anticipated to ensure long-term implant success and high patient satisfaction.
Three main take-aways
- Regenerative treatment of peri-implantitis is viable with advanced decontamination tools like GalvoSurge®
- Combining GBR, soft tissue grafting, and provisionalization supports both function and esthetics
- Patient-centered planning and strict hygiene protocols are essential for successful implant preservation
Author’s testimonial
“In my clinical experience, GalvoSurge® offers a highly effective and predictable method for implant surface decontamination in peri-implantitis cases. Its electrolytic cleaning technology allows thorough biofilm removal without damaging the implant surface, supporting re-osseointegration and improving long-term treatment outcomes.”
Kai Fischer