What is this about?
- A minimally invasive alveolar ridge reconstruction is showcased in region 11 using the permamem® barrier membrane and maxgraft®.
- The treatment workflow combined delayed implant placement, esthetic crown lengthening, and a subepithelial connective tissue graft.
- A predictable esthetic and functional outcome was achieved through peri-implant soft tissue conditioning with a provisional restoration, followed by a definitive crown.
Introduction
This clinical case report presents a successful alveolar ridge reconstruction performed through a minimally invasive approach using a permamem® barrier membrane and maxgraft® in region #11. The procedure was followed by delayed implant placement in combination with esthetic crown lengthening and a subepithelial connective tissue graft. After the peri-implant mucosa was conditioned with a provisional restoration, a definitive crown was placed, meeting both the patient’s esthetic expectations and functional demands.
Initial situation
A 31-year-old female patient presented to our clinic with a history of trauma to tooth #11 during childhood. The tooth had previously undergone root canal treatment and multiple apicoectomies. The patient sought a definitive tooth replacement at site #11 to resolve persistent discomfort and expressed a desire for a long-term solution that would provide esthetic satisfaction, functional stability, and peri-implant health.
The patient reported no systemic diseases and was not taking any medications. Clinical evaluation revealed generalized periodontal parameters consistent with health and adequate oral hygiene. However, site #11 exhibited probing depths of up to 9 mm and an amalgam tattoo on the facial mucosa. Tooth #11 also presented with grade I mobility. Additionally, the patient exhibited altered passive eruption in the anterior maxillary region (Figs. 1-4).
Radiographic examination, including a cross-sectional CBCT image and a periapical radiograph of the region of interest, confirmed the compromised prognosis of tooth #11, showing bone loss around the root apex and previous surgical interventions (Fig. 5).

Fig 5. Cross-sectional cone-beam computed tomography (CBCT) image and periapical radiograph of the region of interest.
Radiographic examination, including a cross-sectional CBCT image and a periapical radiograph of the region of interest, confirmed the compromised prognosis of tooth #11, showing bone loss around the root apex and previous surgical interventions (Fig. 5).
Treatment planning
Brief description of the treatment plan:
- Extraction of tooth #11 followed by minimally invasive alveolar ridge reconstruction using permamem® and maxgraft®.
- After a 4-month healing period, fully guided implant placement was performed in region #11 with a Straumann® Bone-Level Roxolid® SLActive® implant (4.1 mm diameter, 10 mm length). Additionally, esthetic crown lengthening from premolar to premolar and phenotype modification therapy with a connective tissue graft harvested from the posterior palate were carried out.
- At 2.5 months post-implant placement, soft tissue conditioning was initiated using a provisional crown.
- Six months later, the definitive crown was delivered.
Author’s testimonial
As clinicians, we were satisfied with the outcomes achieved. The permamem® membrane was easy to handle, and no excessive plaque accumulation was observed during the healing period. Furthermore, adequate alveolar ridge volume was obtained with the reconstruction procedure with maxgraft®, allowing implant placement without the need for additional bone grafting.
Surgical procedure
Local anesthesia was achieved using Ubistesin (articaine hydrochloride 4% with epinephrine 1:100,000), administered at the buccal and palatal aspects of tooth #11. Tooth #11 was extracted as atraumatically as possible, and all granulomatous tissue was removed by curettage (Fig. 6).

Fig 6. Occlusal view after minimally traumatic tooth extraction, before and after removal of granulomatous tissue.
After the tooth was extracted, the socket at site #11 was found to be damaged, with loss of the buccal bone. A defect in this area was identified, and a tunneling approach was performed using specialized instruments, extending about 3–4 mm beyond the dehiscence defect to allow adequate access for subsequent grafting procedures (Fig. 7).
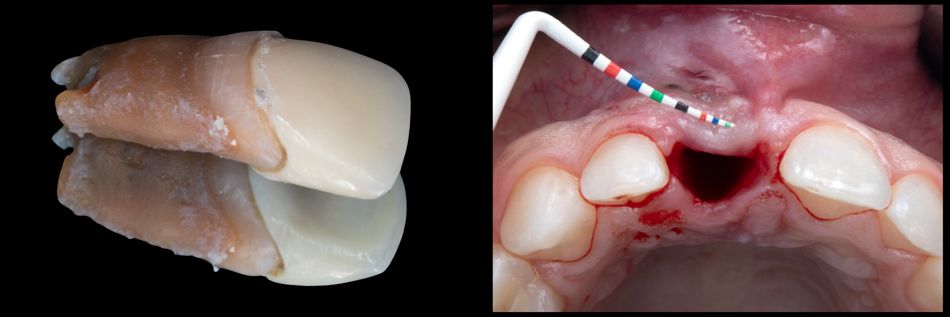
Fig 7. Extracted tooth and clinical view of the damaged socket, showing absence of buccal bone.
A similar small tunnel was created on the palatal side, extending approximately 3 mm. A permamem® membrane was then trimmed into a “guitar-shaped” form to adapt without wrinkling (Fig. 8).

Fig 8. Trimmed permamem® membrane adapted to the buccal dehiscence defect, and occlusal view of implant placement following the tunneling approach.
Allograft particles (maxgraft®) were placed into the socket, filling up to the alveolar crest, with intentional buccal over-augmentation to compensate for expected shrinkage during healing. The membrane was then positioned and stabilized against the palatal mucosa (Fig. 9).
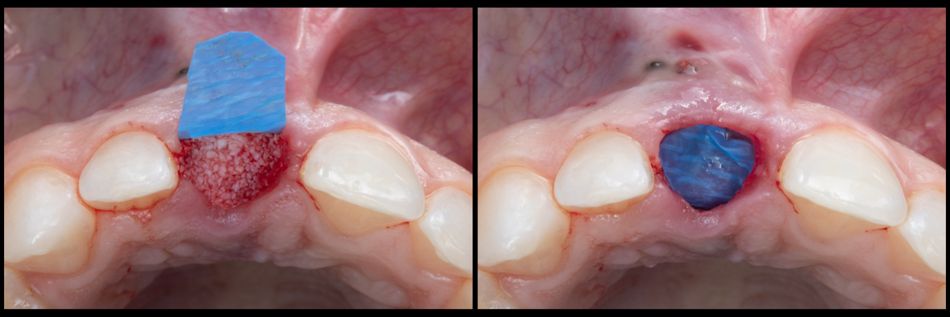
Fig 9. Placement of allograft particles (maxgraft®) filling the socket up to the alveolar crest with buccal over-augmentation. Right: membrane stabilized into the palatal mucosa.
The membrane was stabilized on the palatal aspect, and the mucosa was reapproximated with cross-mattress sutures using non-absorbable material, intentionally leaving part of the membrane exposed (Fig. 10).

Fig 10. Reapproximation of mucosa with cross-mattress sutures using non-absorbable material, leaving the membrane partially exposed.
The patient was instructed to clean the occlusal surface of the membrane daily with chlorhexidine and cotton tips, and to use chlorhexidine mouthrinse for the first two weeks. Postoperative medication included analgesics as needed and antibiotics (co-amoxicillin 1g/625 mg, twice daily for 5 days).
Sutures were removed at 10 days (Fig. 11).

Fig 11. Clinical view 10 days after alveolar ridge reconstruction.
At five weeks, the barrier membrane was removed using forceps without anesthesia, and the site was rinsed with chlorhexidine (Figs. 12-15).
Four months after alveolar ridge reconstruction, local anesthesia was administered at the buccal and palatal aspects of teeth #16–26 (Fig. 16).

Fig 16. Frontal view prior to implant placement, approximately 4 months post healing.
Cross-sectional CBCT imaging and digital implant planning were performed prior to surgery (Fig. 17).
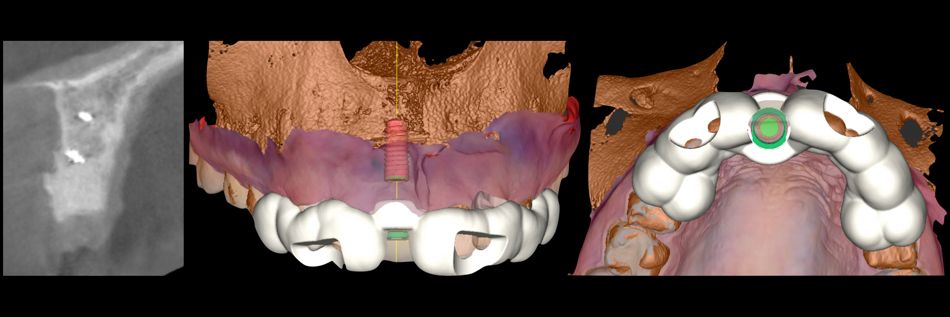
Fig 17. Cross-sectional CBCT image and digital implant planning.
A full-thickness mucoperiosteal flap was then elevated, and esthetic crown lengthening was carried out from premolar to premolar using hand instruments and rotary burs (Figs. 18,19).
Guided implant placement at site #11 was performed according to the manufacturer’s protocol, using a static fully guided approach (Fig. 20), followed by a periapical radiograph to confirm implant position (Fig. 21).
A healing abutment was inserted, and phenotype modification therapy was performed with a connective tissue graft harvested from the posterior palate. The graft was de-epithelialized extraorally with a 15C blade before placement on the buccal aspect (Fig. 22).

Fig 22. Harvesting of a subepithelial connective tissue graft from the posterior palate.
The flap was reapproximated following implant placement and esthetic crown lengthening, demonstrating proper flap closure and tissue adaptation (Fig. 23).
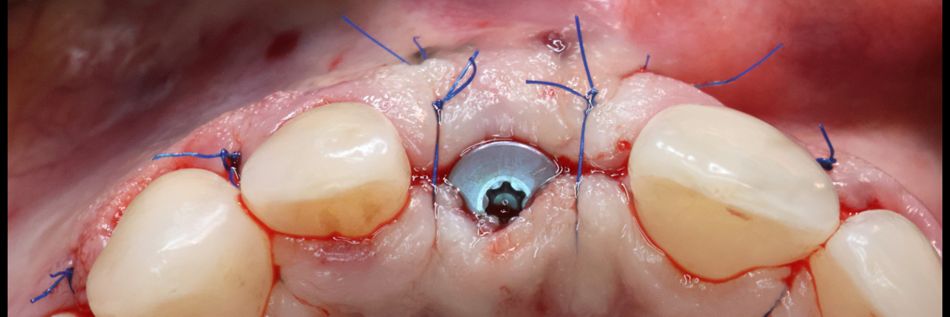
Fig 23. Occlusal view after mucosal reapproximation following implant placement and esthetic crown lengthening.
Two weeks postoperatively showed satisfactory healing and proper tissue adaptation at the surgical site (Figs. 24,25).
Frontal and occlusal views taken 2.5 months postoperatively demonstrated satisfactory healing and stable tissue contours (Fig. 26).

Fig 26. Frontal and occlusal views 2.5 months postoperatively.
Prosthetic procedure
The prosthetic procedure started prior to tooth extraction with an assessment of the available space for the new crown. Clinical examination revealed a small mesio-distal width discrepancy between tooth #11 and its contralateral tooth #21. To address this discrepancy, composite buildup on the mesial aspect of tooth #12 was planned in addition to the implant crown in region #11. This treatment plan was incorporated into the implant positioning for site #11. Furthermore, crown lengthening was planned to optimize the width-to-length ratio of the maxillary anterior teeth.
Following implant placement and the healing period, a conventional loading protocol was implemented with the delivery of a provisional implant crown after digital impression acquisition (Fig. 27).

Fig 27. Provisional crown.
Soft tissue conditioning during this phase was essential to achieve optimal papilla fill and establish the definitive contours for the final implant crown (Figs. 28-30).
After four months of soft tissue stabilization, a definitive impression was obtained for the fabrication of the final screw-retained implant crown. The restoration consisted of a layered zirconia crown cemented to a Variobase® abutment (Figs. 31-33).
Prior to delivery, composite buildup (Ceram.x Spectra®, Dentsply Sirona) on the mesial aspect of tooth #12 was completed using a silicone matrix fabricated from a diagnostic wax-up (Figs. 34,35).
The site was clinically evaluated prior to delivery of the final restoration, showing stable tissue contours and proper healing (Fig. 36).

Fig 36. Clinical view of the region of interest before delivery of the final restoration.
The crown was delivered with 35 Ncm torque, and proper fit was confirmed radiographically with a periapical radiograph (Figs. 37-40).
The patient received comprehensive oral hygiene instructions specific to implant maintenance and was enrolled in the clinic's recall program.
Treatment outcomes
The use of permamem® in combination with maxgraft® for buccal over-augmentation contributed to stable alveolar ridge preservation and predictable soft tissue contours. The membrane remained well-adapted and partially exposed as planned, facilitating guided tissue regeneration while maintaining adequate flap closure.
Following delivery of the final crown, the patient reported high satisfaction with the treatment, noting pleasant esthetics and minimal discomfort. Function was adequate, and no further discomfort was experienced.
A before-and-after comparison and the patient’s final smile and portrait are shown (Figs. 41,42).
Key takeaways
- Use of permamem® and maxgraft® for buccal over-augmentation enables predictable alveolar ridge preservation, stable soft tissue contours, and successful guided tissue regeneration at compromised extraction sites.
- Careful surgical planning and technique, including tunneling, membrane stabilization, and esthetic crown lengthening, contributes to optimal implant placement, flap adaptation, and minimal patient discomfort.
- Clinical and patient-reported outcomes demonstrate high satisfaction, proper function, and esthetic integration of the final restoration, confirming the effectiveness of biologically guided regenerative approaches.


