Initial situation
A 55-year-old woman was referred to our specialized periodontal office due to severe peri-implantitis combined with a general stage III grade b periodontitis (Fig. 1). The peri-implant disease had led to severe bone loss around two of three implants in the right mandible (Fig. 2). The patient was systemically healthy, but smoked 10 cigarettes per day. The peri-implant mucosa showed pocket probing depths up to 10 mm with bleeding on probing and suppuration.
Treatment Planning
The treatment was supposed to start with a systematic periodontal therapy including full mouth subgingival debridement accompanied by administration of systemic antibiotics. After reevaluation of the initial therapy following the first supportive periodontal therapy, the implants received another subgingival debridement combined with local antibiotics. After a healing period of about 2 weeks, the surgical intervention was planned as a combined regenerative-resective procedure with guided bone regeneration (GBR) and implantoplasty. After 8 months the result of the treatment should be evaluated.
Surgical procedure
After periodontal examination, a full mouth subgingival debridement was performed following the principles described by Quirynen et al.1 and Cosyn et al.2. Amoxicillin 500 mg three times a day for seven days and Metronidazole 400 mg three times a day for seven days were administered as systemic antibiotics. After 8 weeks the reevaluation was performed with another complete periodontal examination and supragingival debridement. During the same treatment session, the area of the implants in the fourth quadrant was anesthetized and, again, a subgingival debridement was performed. During this procedure, a Labrida BioCleanTM chitosan brush was used to thoroughly clean the exposed implant surfaces (Figs. 3a-c).
In the next step, a local antibiotic was administered as a sustained delivery device (Ligosan®, Haereus Kulzer, Germany) (Figs. 4,5). The peri-implant soft tissues were allowed to heal while the local drug acted on the bacteria in the peri-implant pocket for 14 days.
The surgical intervention was performed after intravenous sedation using Midazolam combined with Novaminsulfon as a painkiller. After anesthetization, a mucoperiosteal buccal and lingual flap was raised using a sulcular incision, while avoiding the removal of any keratinized mucosal tissue.
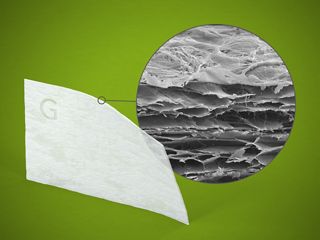
Once all granulation tissue was removed, the implant surfaces were smoothened using hard metal burs up to 1 mm underneath the edge of the bony defect (Fig. 8). The more apical parts of the exposed implant surfaces were thoroughly cleaned using a titanium brush (Figs. 9,10).
Utilizing a Safescraper, autologous bone chips were harvested from the retromolar area (Fig. 11).
The demineralized bovine biomaterial (Straumann® Xenograft®) was mixed with enamel matrix proteins (Straumann® Emdogain®) and was subsequently combined with the autologous particles (Figs. 12-14).

Want to stay up to date?
youTooth.com is THE PLACE TO BE IN DENTISTRY – subscribe now and receive our monthly newsletter on top hot topics from the world of modern dentistry.
The intrabony defects were completely filled with the combined autologous-xenogeneic bone chips up to the crest of the defect. Care was taken not to overfill. The guided bone regeneration was completed by inserting a collagen membrane (Jason® membrane, botiss, distributed by Straumann Biomaterials), fixed by resorbable sutures to the buccal periosteum, and to the apical parts of the flap on the lingual site (Fig. 15). After, periosteal slitting, care was taken to ensure wound closure was tension-free (Fig. 16).
Postsurgical Treatment
Post surgically, ibuprofen 400 mg was administered up to four times per day for pain control. The patient was advised to rinse with 0.2% chlorhexidine solution for 10 weeks. Professional supragingival plaque control was performed every week for the first four weeks. 8 weeks after the augmentation, a complete supportive periodontal therapy was performed, avoiding any subgingival instrumentation in the area of the GBR procedure. The SPT was repeated after 3 months and then again after 6 months, when radiographic pictures and pocket probing depths were taken to assess the radiographic and clinical outcome of the procedure.
Treatment Outcomes
The surgical site recovery was uneventful and signs of inflammation could be successfully reduced. Pocket probing depths which were up to 10 mm in the beginning could be reduced to 5 mm without bleeding on probing. No suppuration occurred after the initial periodontal treatment. Almost complete bone fill of the intrabony defects could be observed radiographically (Fig. 18). The patient is in a three-month regular supportive periodontal therapy program and, so far, no recurrence of inflammation was observed.