Straumann at the EuroPerio 8
London, UK - June 3-6, 2015
From "one fits all" to indication based use of biomaterials - a shift of paradigm in regenerative treatment concepts.
Straumann Corporate Forum
Presentation #1 - Contemporary concepts and new developments for improving the outcomes of reconstructive periodontal surgery - Prof. Dr. Anton Sculean

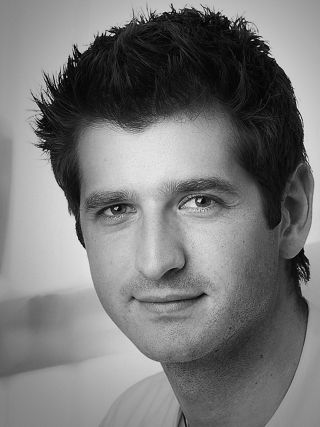
Speaker: Prof. Dr. Anton Sculean, Switzerland
Biography
Anton Sculean is professor and chairman of the Department of Periodontology at the University of Bern in Switzerland. He qualified in 1990 at the Semmelweis University in Budapest, Hungary and has received his postgraduate training at the Universities Münster, Germany and Royal Dental College Aarhus, Denmark. He received his habilitation at the University of Saarland, Homburg, Germany. Professor Sculean has been a recipient of many research awards, among others the Anthony Rizzo Award of the Periodontal Research Group of the International Association for Dental Research (IADR), and the IADR/Straumann Award in Regenerative Periodontal Medicine. He received honorary doctorates (Dr. h.c.) from the Semmelweis University in Budapest, Hungary and from the Victor Babes University in Timisoara, Romania. He has been the author of more than 160 publications in peer reviewed journals and is on the editorial board of more than 10 dental journals. Professor Sculean served from 2009-2010 as president of the Periodontal Research Group of the IADR and is currently president of the Swiss Society of Periodontology. His current research interests include periodontal wound healing, regenerative and plastic-esthetic periodontal therapy, treatment of peri-implantitis, antibiotic and antiseptic therapies, laser treatments and oral biofilms.
Aims
Advances in cell and molecular biology have contributed to increased understanding of wound healing of various tissues, and revealed a great complexity of processes involved. In general, the outcome of wound healing can be characterized either as repair, i.e. scar tissue formation that differs in form and/or function from the original tissues, or regeneration, i.e. form and function of the lost tissues are restored. A large body of evidence has established that polypeptide growth and differentiation factors, enamel matrix proteins, barrier membranes, certain bone grafts or various combinations thereof may support periodontal wound healing/regeneration creating an environment conducive to and/or immediately inducing de novo tissue formation. Moreover, it is now clear that reconstructive periodontal procedures can only be successful if patient related factors and biologically driven surgical approaches, aiming to enhance wound stability are considered.
Objectives
The presentation will provide an overview on the biologic background, surgical considerations and clinical decision tree of using various biomaterials in reconstructive periodontal surgery for intrabony, furcation and recession defects. Finally, future perspectives will be presented on upcoming indications such as the use of enamel matrix derivative for treating horizontal types of defects and the combination of various collagen substrates and enamel matrix derivative to maximize healing outcomes in recession defects.
Presentation #2 - Augmentation procedures of soft and hard tissues using biomaterials – predictable in the daily practice - PD Dr. Dr. Daniel Rothamel
Speaker: PD Dr. Dr. Daniel Rothamel, Germany
Biography
Daniel Rothamel is a graduate of the Heinrich-Heine University of Duesseldorf, Germany, and received his Dr. med. dent. with the thesis “Establishing a new method for quantification of tooth hypersensitivity". He was trained in oral surgery and also obtained the Dr. med with his thesis on “Biocompatibility, biodegradation and angiogenetic aspects of native and cross-linked collagen membranes”. From 2002-2007 he worked as a Research Associate at the Department of Oral Surgery (Prof. Dr. J. Becker) at the Heinrich-Heine University in Duesseldorf, Germany. In 2005, he volunteered at the Clinic of Plastic and Reconstructive Surgery in Sankhu, Kathmandu, Nepal before he went in 2007 to Australia to start a post-doc position at the Department of Oral Pathology and Molecular Research, Westmead Hospital, University of Sydney, Australia (granted by DAAD). In 2008, Daniel Rothamel moved back to Germany to work as a Research Associate in the Department of Oral and Maxillofacial Plastic Surgery (Prof. Dr.Dr. J. Zoeller), University of Cologne, Germany and received his PhD on “Reconstruction of jaw defects using artificial and autogenous bone blocks in combination with growth factors”. Daniel Rothamel is best known for his research interest in guided bone regeneration, implant surfaces, collagen membranes, bone substitute materials, and growth factors.
Aims
One of the most challenging procedures in dental implantology is the predictable and safe regeneration of bone and soft tissue defects. Although autogenous bone is still considered being the golden standard, different biomaterials such as bone substitutes and membranes have shown predictable results in augmentation procedures of the alveolar process. Whereas the regeneration of smaller defects inside the ridge contour may be supported by transmembraneous angioselectivity of the applied membranes, extended defects require volume-stable bone substitute materials and long-lasting barriers. Native porcine pericardium has shown favourable results, based on its multi-layered collagen structure. Moreover, available bone substitutes differ significantly in terms of biochemical aspects, influencing the volume stability, speed of bone formation, graft remodelling and patient´s acceptance. Also the quality of the recipient site, the osteogenicity of the graft and the selected healing time are affecting the predictability of the regeneration outcome.
In addition to bone augmentation biomaterials, specific collagen matrices have been established for soft tissue augmentation procedures, including gingiva thickening, vestibuloplasty and recession coverage. In contrast to the patient´s own soft tissue, the use of biomaterials is not accompanied by donor site morbidity.
Objectives
This presentation will detail selection rules of different collagen matrices and different bone graft materials that fit to the indication, the defect´s shape and to the patient's preconditions in order to achieve the best regeneration outcome. Based on clinical examples new treatment options of prevalent clinical indications like socket preservation that arise from the availability of novel collagen soft tissue grafts will be presented.
Presentation #3 - Straumann®Osteogain – A new chapter in the clinical use of enamel matrix proteins - Prof. Dr. David L. Cochran

Speaker: Prof. Dr. David L. Cochran, USA
Biography
David L. Cochran is a graduate of the University of Virginia and received his D.D.S., M.S. and Ph.D. in Biochemistry from the Medical College of Virginia (MCV). He was trained in Periodontology at the Harvard School of Dental Medicine where he also obtained a second Master‘s degree. He recently received an Honorary Doctorate from the University of Bern in Switzerland. Dr. Cochran is currently Professor and Chairman of the Department of Periodontics at The University of Texas Health Science Center at San Antonio, Dental School. Prior to his appointment at San Antonio, Dr. Cochran was Director of Postgraduate Periodontics at MCV. Dr. Cochran is a member of many professional dental organizations and is a Diplomate of the American Board of Periodontology. He is a fellow of the American College of Dentistry and the International College of Dentistry. Dr. Cochran has published numerous scientific articles and abstracts on various periodontal, biochemistry, and implant topics. He has received awards for his research work at both the national and international levels. Dr. Cochran is an active basic science and clinical researcher who has received funding from both the NIH-NIDCR and private industry.
Aims
Enamel matrix proteins have been clinically used for more than 2 decades and have been documented by vast clinical and preclinical research. Despite the broad biologic potential of enamel matrix proteins to stimulate various cell and tissue types into regenerative and tissue forming patterns, the potential of this component class has been so far only fully explored for the successful treatment of periodontal indications. Recent advances in the research on enamel matrix proteins as a mixture and as partial fractions of the mixture, show that besides inducing periodontal regeneration, enamel matrix proteins stimulate important processes for the formation, maturation and, regeneration of bone, such as the stimulation of osteoblasts and stem cells and the promotion of angiogenesis. With these properties in mind enamel matrix proteins can per se be classified as promising candidates to promote bone growth and bone maturation as part of clinical bone augmentation procedures in periodontology and, importantly in implantology.
Objectives
This presentation introduces Straumann®Osteogain as a new biologic solution that has been developed and optimized for the mixing with bone graft materials and collagen substrates to stimulate bone formation as part of regenerative bone augmentation procedures. It introduces the product concept and rationale, its components and its biological properties to stimulate various physiological activities that are clinically relevant for various bone augmentation procedures.
Innovative and predictable treatment concepts helping to satisfy demanding patient needs.
Straumann Corporate Forum II
Presentation #1 - Successful and predictable single tooth implant therapy: make the right decisions! - Prof. Dr. Ronald Jung

Speaker: Prof. Dr. Ronald Jung, Switzerland
Biography
Ronald Jung is trained in oral surgery, prosthodontics and implant therapy. He is currently Vice Chairman of the Department of Fixed & Removable Prosthodontics and Dental Material Sciences at the University of Zurich in Switzerland (Chairman: Prof. Dr. Ch Hämmerle). In 2006 he worked as Visiting Associate Professor at the Department of Periodontics at the University of Texas Heath Science Center at San Antonio, USA (Chairman: Prof. Dr. D. Cochran). 2008 he finalized his „Habilitation“ (venia legendi) in dental medicine and was appointed associate professor at the University of Zürich. In 2011 he completed his PhD doctorate degree of the University of Amsterdam, ACTA dental school, The Netherlands. In 2013 he worked as Visiting Associate Professor at the Department of Restorative Dentistry and Biomaterials Sciences at Harvard School of Dental Medicine in Boston, USA. He is an accomplished and internationally renowned lecturer and researcher, best known for his work in the field of hard and soft tissue management and his research on new technologies in implant dentistry.
Aims
The aim of this lecture is to provide a comprehensive overview of the important steps needed from initial risk analysis until delivering of the final reconstruction.
Objectives
In order to achieve an optimal solution after replacing a missing tooth with an implant a sequence of decisions and an appropriate timing of the treatment steps are of great importance.
A successful and predictable implant therapy starts with a locally and systemically related risk assessment. Based on risk assessments individual treatment strategies for handling of extraction sockets, implant timing, implant selection, soft and hard tissue regeneration as well as for prosthetic decisions are necessary.
The focus will be on solutions for handling of extraction sockets and implant placement timing, for implant selection in terms of length and diameter and for the selection of abutments and crowns.
Presentation #2 - How to determine the optimal number of implants and the prosthetic treatment strategy for partially and totally edentulous patients - Prof. Dr. Bjarni Pjetursson

Speaker: Prof. Dr. Bjarni Pjetursson, Iceland
Biography
Bjarni E. Pjetursson, received his DDS from University of Iceland in 1990. From 1990 to 2000 he worked as a general dentist in his private clinic in Iceland. In 2000 he started his postgraduate training in Periodontology and Implant Dentistry at the University of Bern, Switzerland. He received his specialist certificate and Masters degree in Periodontology (EFP & SSP) and Doctorate in Dentistry (Dr. med. dent) from the Faculty of Medicine, University of Bern, Switzerland. From 2003 to 2005 he received his postgraduate training in Prosthodontics at the University of Bern, Switzerland. From 2005 he was an Assistant Professor and Senior lecturer at the Department of Periodontology and Fixed Prosthodontics, University of Bern and is presently the Chairman of the Department of Prosthodontics, Faculty of Odontology, University of Iceland. Dr. Pjetursson is an ITI Fellow and member of the editorial board of Clinical Oral Implants Research.
Aims
This lecture will focus on:
- Different treatment approaches to select the optimal number of implants.
- How to choose the best implant length and diameter in a given indication.
- How to decide on certain treatment protocols which help to improve treatment time, costs and the extent of surgical intervention.
Objectives
In daily practice, dentists routinely face the challenge of making fast and difficult decisions. There is an abundance of literature with different protocols of how to design implant-supported fixed dental prostheses in terms of the number, length and diameter of implants required to support such reconstructions. For fully edentulous patients, the number of implants recommended to support full-arch reconstructions in the maxilla ranged from 4 to 22. Meanwhile, in the mandible, this ranged from 3 to 18 implants. So what is the optimal number of implants? And how can the dentist make the right decision?
During this lecture, the pre-requisites for deciding on the number of implants needed to support different types of reconstructions will be discussed. In addition, the question of how to use short and narrow diameter implants to avoid complicated bone augmentation procedures will be addressed. Finally, there will be the opportunity to determine which clinical situations are suitable for using tilted implants.
Common clinical situations of partially and fully edentulous patients will be presented. Evidence-based treatment planning will be done with consideration of the number, size and type of implants required, also with the material and retentive mechanisms of the prosthetic components to be selected.
The single flap approach – a simplified procedure for periodontal regeneration.
Straumann Workshop
Presentation #1 - The single flap approach – a simplified procedure for periodontal regeneration - Prof. Dr. Leonardo Trombelli, DDS, PhD

Speaker: Prof. Dr. Leonardo Trombelli, DDS, PhD, Italy
Biography
Full Professor and Chair, Periodontology and Implantology, School of Dentistry, University of Ferrara, Italy. Director, Research Center for the Study of Periodontal and Periimplant Diseases, University of Ferrara. Director, Dental Clinic, University Hospital, Ferrara. Active member of the Italian Society of Periodontology and the Italian Society of Implantology. Editorial Board member for the Journal of Clinical Periodontology, member of the peer review panel for the Journal of Periodontology.
Abstract
Deep intrabony defects represent a challenge for the clinician since, if not properly treated, they can lead to tooth loss. Over the past years, various approaches aimed at a substantial improvement of the clinical conditions of the tooth affected by the lesion associated with the regeneration of the lot attachment apparatus have been developed.
The single flap approach (SFA) in combination with regenerative devices is a simplified surgical procedure to effectively treat deep intrabony defects while minimizing surgical trauma and post-surgery complications.
In this workshop, the expert, Prof. Leonardo Trombelli, will present the SFA, its indications and surgical protocol. A hands-on session on pig jaws will follow, giving the participants the opportunity to practice the fundamental steps of the single flap approach in combination with Straumann® Emdogain®.
Aim
The aim of the course will be to thoroughly define advantages and limitations of a simplified surgical approach, the Single Flap Approach (SFA), specifically designed for the treatment of deep intrabony defects. In particular, the possibility that SFA may enhance condition for wound stability, leading to eventual periodontal regeneration, will be discussed when used in conjunction with reconstructive technologies.
Objectives
- Define the diagnostic aspects of intrabony lesions suitable for the surgical access by SFA;
- Discuss the advantages of the surgical flap approach to enhance conditions for wound stability and minimize post-surgical pain and discomfort;
- Outline the clinical outcomes, in terms of early and late wound healing, of the SFA when compared to the conventional double-flap surgical procedures;
- Critically appraise which regenerative technologies (membrane, biological agents, combinations) are most indicated when used in conjunction with SFA.
- Hands-on activity to teach the surgical steps of SFA when combined with graft biomaterial and Enamel Matrix Derivative (Straumann® Emdogain®)




