The following article is based on the review of selected, currently available scientific reports. It cannot replace official statements issued by your local health authorities or government guidelines.
What is the novel coronavirus-19 (COVID-19)?
The infectious agent of viral pneumonia originated in Wuhan (China) is recognized as a novel coronavirus (2019-nCoV), which causes COVID-19. The signs and symptoms include respiratory symptoms and fever, cough, and shortness of breath. In more severe cases, the infection can cause pneumonia, severe acute respiratory syndrome, and sometimes death. WHO declared COVID-19 a pandemic on 11/03/2020, pointing to “alarming levels” of spread and severity and confirmed that it is a first pandemic caused by a coronavirus.[1]
Dental professionals are strongly recommended to stick to the guidelines and recommendations communicated by the respective dental associations of the region or follow the recommendation by the American Dental Association (ADA) and Centers for Disease Control and Prevention, USA (CDC). “The use of standard precautions within the dental workplace and acquiring a thorough history of symptoms and potential exposure for patients is critical for dental health care professionals to maintain a healthy working environment, whether the concern is flu, 2019-nCoV or other transmissible illnesses,” said Dr. Maria Geisinger, chair of the ADA Council on Scientific Affairs.[2]
Transmission routes
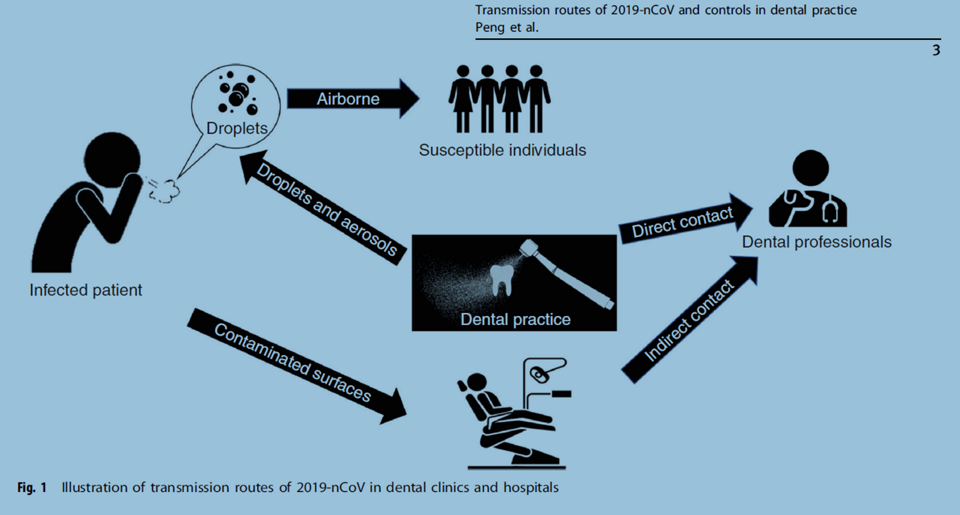
The typical routes of transmission for the 2019 n-CoV are either via a direct transmission (cough, sneeze, and droplet inhalation) or via contact transmission (contact with oral, nasal and eye mucous membranes).[3, 4] Also, studies have shown that the disease could be transmitted directly or indirectly through saliva. It was reported that live viruses were present in the saliva of infected individuals.[5]
Dental patients and professionals can be exposed to viruses and bacteria that infect the oral cavity and respiratory tract. Dental care settings always bear the risk of COVID-19 infection due to the procedures which involve face-to-face communication with patients and frequent exposure to saliva, blood, and handling sharp instruments.[3]
Infection controls for dental practice
Dental professionals should be familiar with;
- How 2019-nCoV is spread,
- How to identify patients with 2019-nCoV infection and
- What extra-protective measures should be adopted during daily practice to prevent the transmission of 2019-nCoV.
The infection control measures should be followed by dental professionals, mainly because aerosols and droplets are the main routes of transmission of 2019-nCoV.
These recommendations are reported in the recently published article[3], which is based on;
- The Guideline for the Diagnosis and Treatment of Novel-Coronavirus Pneumonia (the 5th edition) http://www.nhc.gov.cn/yzygj/s7653p/202002/3b09b894ac9b4204a79db5b8912d4440.shtml
- The Guideline for the Prevention and Control of Novel Coronavirus Pneumonia in Medical Institutes (the 1st edition) http://www.nhc.gov.cn/yzygj/s7659/202001/b91fdab7c304431eb082d67847d27e14.shtml and
- The Guideline for the Use of Medical Protective Equipment in the Prevention and Control of Novel Coronavirus Pneumonia http://www.nhc.gov.cn/yzygj/s7659/202001/e71c5de925a64eafbe1ce790debab5c6.shtml released by the National Health Commission of the People’s Republic of China, and the practice experience in West China Hospital of Stomatology related to the outbreak of COVID-19 transmission.[3]
Patient assessment:
I. Firstly, the dentists ought to be able to recognize a suspected case of COVID-19. Overall, a patient with COVID-19 who is in the acute febrile phase of the disease is not recommended to visit the dental clinic. If this does occur, the dental professional should be able to identify the patient with suspected 2019-nCoV infection and should not treat the patient in the dental clinic. He/she shall immediately made sure to report the patient to the infection control department as soon as possible for quarantine.
II. The body temperature of the patient should be measured. A contact-free forehead thermometer is strongly recommended for the screening.
III. A questionnaire should be used to screen patients with the potential infection before they could be led to the dental chair-side. This questionnaire should belong to the regular patient record and saved. These questions should include the following:
- Do you have a fever or experienced fever within the past 14 days?
- Have you experienced a recent onset of respiratory problems, such as a cough or difficulty in breathing within the past 14 days?
- Have you, within the past 14 days, traveled to a country reported to be infected according to the World Health Organization with documented 2019-nCoV transmission?
- Have you come into contact with a patient with confirmed 2019- nCoV infection within the past 14 days?
- Have you come into contact with people from the neighborhood/region reported to be infected according to the World Health Organization who have recently documented fever or respiratory problems within the past 14 days?
- Are there at least two people with documented experience of fever or respiratory problems within the last 14 days having close contact with you?
- Have you recently participated in any gathering, meetings, or had close contact with many unacquainted people?
» If a patient replies “yes” to any of the screening questions, and his/her body temperature is below 37.3 °C, the dentist can defer the treatment until 14 days after the exposure event. The patient should be instructed to self-quarantine at home and report any fever experience or flu-like syndrome to the local health authorities.
» If a patient replies “yes” to any of the screening questions, and his/her body temperature is no less than 37.3 °C, the patient should be immediately quarantined, and the dental professionals should report to the infection control department of the hospital or the local health department.
» If a patient replies “no” to all the screening questions, and his/her body temperature is below 37.3 °C, the dentist can treat the patient with extra protection measures and avoid spatter or aerosol-generating procedures to the best.
» If a patient replies “no” to all the screening questions, but his/her body temperature is no less than 37.3 °C, the patient should be instructed to the fever clinics or specialized clinics for COVID-19 for further medical care.
Standard precautions include:
Hand hygiene.
Emphasis on proper hand hygiene is extremely important. In particular, the oral care professionals should wash their hands with soap or disinfect the hands with alcohol-based sanitizers;
- before a patient examination,
- before dental procedures,
- after touching the patient,
- after touching the surroundings and equipment without disinfection, and
- after touching the oral mucosa, damaged skin or wound, blood, body fluid, secretion, and excreta.
- More caution should be taken for dental professionals to avoid touching their own eyes, mouth, and nose.
Use of personal protective equipment (gloves, masks, eyewear).
Considering that airborne droplet transmission of infection is the main route of spread, particularly in dental clinics and hospitals, barrier-protection equipment, including protective eyewear, masks, gloves, caps, face shields, and protective outwear, is strongly recommended for all healthcare givers in the clinic/hospital settings.
Based on the possibility of the spread of infection, three-level protective measures of the dental professionals are recommended for specific situations;
a. Primary protection (standard protection for staff in clinical settings).
- A disposable working cap,
- disposable surgical mask,
- working clothes (white coat),
- protective goggles or face shield,
- disposable latex or nitrile gloves.
b. Secondary protection (advanced protection for dental professionals).
- disposable doctor cap,
- disposable surgical mask,
- protective goggles or face shield,
- working clothes (white coat) with disposable isolation clothing or surgical clothes outside,
- disposable latex gloves.
c. Tertiary protection (strengthened protection when contact patient with suspected or confirmed 2019-nCoV infection).
Although a patient with 2019-nCoV infection is not expected to be treated in the dental clinic, in the unlikely event that this does occur, and the dental professional cannot avoid close contact, special protective outwear is needed.
- If protective outwear is not available, working clothes (white coat) with extra disposable protective clothing outside should be worn.
- In addition a disposable cap,
- protective goggles/face shield,
- disposable surgical mask,
- disposable latex gloves,
- and impermeable shoe cover should be worn.
Mouthrinse before dental procedures.
A preoperational antimicrobial mouth rinse is generally believed to reduce the number of oral microbes. Chlorhexidine may not be sufficient to eliminate 2019-nCoV.[3] Preprocedural mouthrinse containing oxidative agents such as 1% hydrogen peroxide or 0.2% povidone is recommended, for reducing the salivary load of oral microbes, including potential 2019-nCoV. [3]
Rubber dam isolation
- The use of rubber dams can significantly minimize the production of saliva- and blood-contaminated aerosol or spatter, particularly in cases when high-speed handpieces and dental ultrasonic devices are used.
- When a rubber dam is applied, extra high-volume suction for aerosol and spatter should be used during the procedures along with regular suction.
- If rubber dam isolation is not possible in some cases, manual devices, chemo-mechanical caries removal, and hand scaler are recommended for caries removal and periodontal scaling to minimize the generation of aerosol as much as possible.[3]
Anti-retraction handpiece
The high-speed dental handpiece without anti-retraction valves may aspirate and expel the debris and fluids during the dental procedures. More importantly, the microbes, including bacteria and viruses, may further contaminate the air and water tubes within the dental unit, and thus can potentially cause cross-infection. The use of dental handpieces without anti-retraction function is prohibited during the epidemic period of COVID-19.
Anti-retraction dental handpiece with specially designed anti-retractive valves or other anti-reflux designs is strongly recommended as an extra preventive measure for cross-infection. [3]
Disinfection of the clinic settings
Medical institutions should take effective and strict disinfection measures in both clinical settings and public areas. The clinic settings should be cleaned and disinfected following the Protocol.[3]
As the coronavirus can stay alive on surfaces for more than 24 hours, it is crucial to keep all surfaces clean and sanitized. While this pertains to the waiting room, the bathroom, and the front desk, it is particularly vital to disinfect the operatory as frequently as is feasible. Common cleaners such as 0.1% sodium hypochlorite, 0.5% hydrogen peroxide, or 62-71% ethanol have all been shown to be effective.[6]
Public areas and appliances should also be frequently cleaned and disinfected, including door handles, chairs, and desks. The elevator should be disinfected regularly. People taking elevators should wear masks correctly and avoid direct contact with buttons and other objects.
Management of medical waste
The medical waste (including disposable protective equipment after use) should be transported to the temporary storage area of the dental clinic/ medical institute timely. The reusable instrument and items should be pretreated, cleaned, sterilized, and appropriately stored following the Protocol.
The medical and domestic waste generated by the treatment of patients with suspected or confirmed 2019-nCoV infection is regarded as infectious medical waste. Double-layer yellow color medical waste package bags and “gooseneck” ligation should be used. The surface of the package bags should be marked and disposed of according to the Protocol.[3]
Front Desk Staff
Front desk staff should also have N95 mask/respirator for their protection. A barrier should be established between the patient and the front desk staff. Front desk staff should stay at least 6 feet away from patients.[6]
Conclusion
The dental profession has numerous challenges and occupational hazards, the COVID-19 being the new one on the block. Be cautious, focused, and follow the recommendations issued by the local health authorities or recommendations of the regional dental councils until we have a better insight and command of this disease.
These recommendations outlined are obviously subject to change as the clinical situation evolves. However, they are undoubtedly practical cornerstones to help dental professionals steer these anxious moments.
As health care professionals and responsible citizens of the world, we all have a role to play in slowing the spread of the coronavirus and “flattening the curve” by following sound scientific, public health advice, which will help limit infections and slow down the spread of the virus. The spread of COVID-19 entirely depends on our collective actions.
We firmly believe by taking these extraordinary precautions a dentist can make a difference in helping to sustain the limited supply of personal protection equipment (PPE) critical for emergency dental care and frontline health care personnel responding to the pandemic
Please keep yourselves and your patients safe!
References
- WHO, WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020.
- Versaci, M.B., CDC Reminds Clinicians to Use Standard Precautions, Recommends Isolating Patients with Coronavirus Symptoms. . American Dental Association, February 7, 2020.
- Peng, X., et al., Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci, 2020. 12(1): p. 9.
- Meng, L., F. Hua, and Z. Bian, Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res, 2020: p. 22034520914246.
- To, K.K., et al., Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis, 2020.
- Fang, L.S.T., Coronavirus and the Dentist, 2020, DOCS Education.