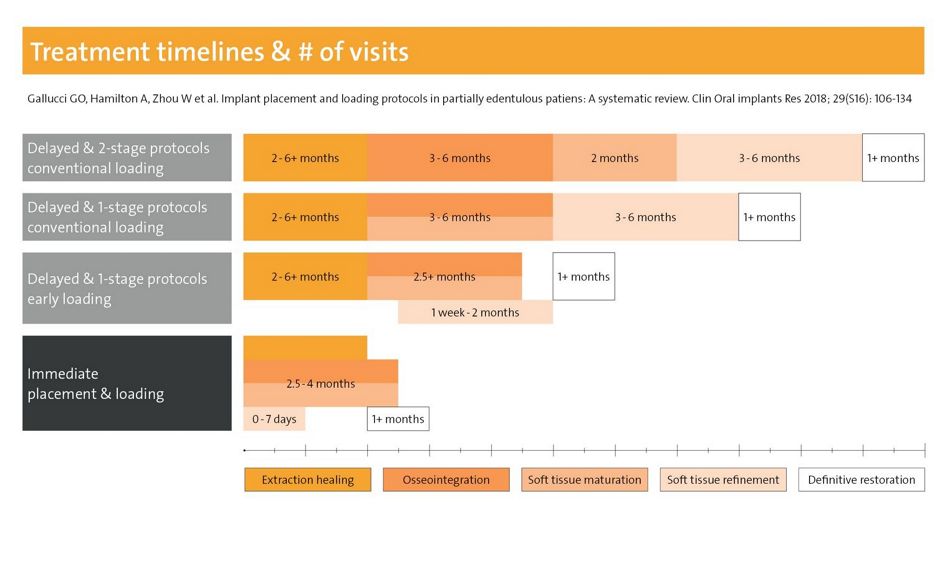
Fig. 1: Treatment duration and number of visits can be significantly reduced with immediate or early placement and restorative protocols
With courtesy of Leziy/Miller, taken from a review article by Dr Jan Koch.
To preserve precious tissues and meet patient expectations implants should be placed within the first four months after tooth extraction. According to the latest ITI consensus paper, this is “due to the risk of alveolar resorption and reduction in bone volume, as well as the extended treatment time” for Type 4 placement (6 months or later)1, 3. Alternatively, a post-extraction (Type 1) or early (Type 2 or 3) implant insertion is preferable. Decisions will depend on diagnostic findings, e.g. as proposed in the SAC classification by the International Team for Implantology (ITI), and on the clinical expertise of the team4-6.
According to recent conference presentations, immediate placement can be indicated in sockets with more than 50% intact walls and thick biotypes. Risk factors include a non-optimal implant diameter or situations where primary stability requires a prosthetically non-optimal implant position (Dr Frank Schwarz, Germany, presentation at the Europerio 2022). According to Dr Ronald Jung (Switzerland) dedicated tissue level implants (Straumann® TLX, details see below) are optimized for immediate protocols in posterior areas.
Moreover, clinicians should be aware that physiological soft tissue thickening after extractions may mask an extended bone defect in patients with thin soft tissue types7. Therefore soft tissue or GBR augmentations are often indicated in connection with immediate or early implant placement4. For these indications different xenogeneic (e.g. Straumann® Xeno Graft) or allogenic grafting materials are available, which can be complemented by, e.g., the flexible Jason® collagen membrane.
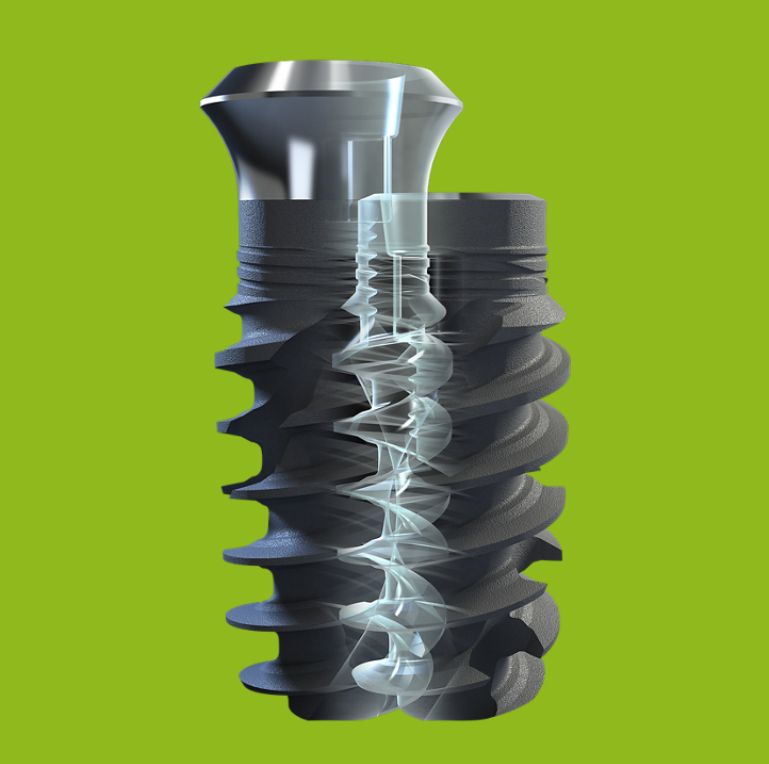
Figure 2: Both the Straumann® BLX (Bone Level) and Straumann® TLX (Tissue Level) Implant Systems have an identical deeply structured endosteal thread macro design. There is only one surgical tray for both systems, which allows to adapt the protocol to the intra-operative situation.
Implant systems designed for stability
Modern implant designs can enhance and simplify time-saving insertion and restorative protocols. For increased primary stability especially in soft bone, specific macro designs have been developed8, 9. For example, the Straumann® BLX implant system (Fig. 2) improves bone management, e.g. by means of a conical shape of the implant body with reduced neck diameter, deeply structured threads, bidirectional cutting and bone condensing properties. The thread design was transferred to the Straumann® TLX implant system (Fig. 2). Other Straumann® implants systems including the Zygomatic™ are equally compatible with digital and immediate placement or restorative options.

Figure 3: The Straumann® TLX implant combines a smooth transgingival collar with an aggressive thread design optimized for high primary stability
Picture courtesy of Dr Mario Rocuzzo, see full case report here.

Figure 4: Straumann® BLT implants are being used for this full arch case with fully guided surgery and immediate temporary loading
Picture courtesy of Dr Nikolay Makarov, see full case report here.
To enhance osseointegration and provide maximum secondary stability during bone remodeling (after 2-4 weeks), a chemically modified surface has been developed (Straumann® SLActive®)10, 11. This is especially relevant in connection with early loading or in patients with compromised systemic health12. The highly stable implant material Straumann® Roxolid® adds maximum fracture resistance. This combination of macro, micro and chemical implant features increase the predictability of immediate and early protocols. Finally, with transgingival healing only one surgery is needed in many cases.
