Benefits of the Axiom X3® implant for primary stability in the maxillary region.

Dr. Philippe COLIN
QUALIFIED SPECIALIST IN ORAL SURGERY
France
- Private practitioner in Montpellier
- MSc in oral implantology
Case introduction:
This 65-year-old patient was a non-smoker in good health. He presented with good periodontal status and a low (or maintained low) smile line. Many restorations had been carried out over time, without affecting occlusal function. There was a natural diastema between teeth 11 and 21. There were also two bridges, created to offset agenesis of the maxillary lateral incisors.
The initial consultation was in 2018, following an inflammatory episode of endodontic origin affecting 23 (located in position 22), resolved by antibiotic therapy. At that time, the patient had not agreed to the proposed implant therapy, which was eventually started in 2021 after trust was built up following prolonged treatment in the lower right quadrant.
Initial situation
1. The two mesially tipped upper canines and first premolars supported two bridges that had been remade 3 times. Repeated decementation in the upper left quadrant and an infection in 2018 made the patient decide to agree to the proposed implant treatment.
Surgical procedure:
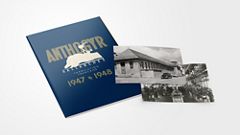
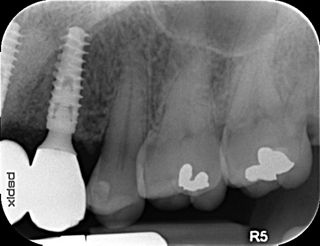
2a-b-c. Initial X-rays. The cause of the endodontic lesions was obvious, and they are underestimated on these retro-alveolar X-rays.
3a-b. Note the strip of keratinized gingiva and its 1 mm attachment. The roots were extracted. The sites were thoroughly debrided of all granulation tissue and filled with Bio-Oss® Collagen. Each site was hermetically resealed using a coronally positioned flap.
4a-b. Healing 5 months later. The patient wore a removable overdenture. Vestibular ridge resorption was moderate and bone volume, estimated using CBCT, was sufficient to allow the placement of Axiom X3® Ø 3.4 mm implants in positions 12 and 22 and Ø 4 mm implants in positions 14 and 24.
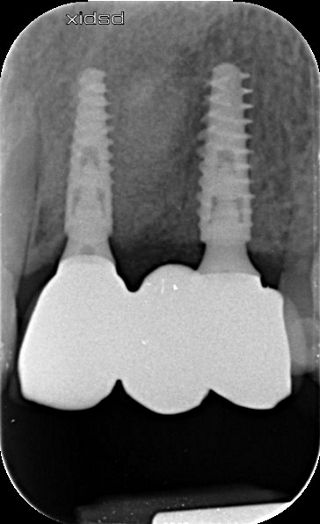
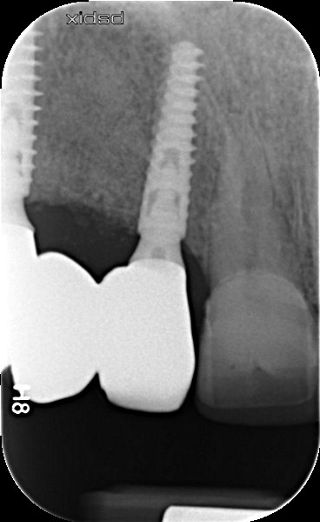
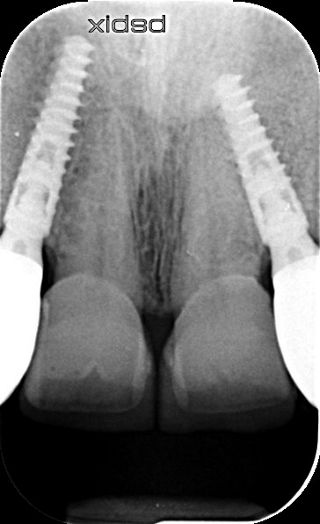
5a-b. Implants were placed away from the edge of the vestibular bone, 0.5 to 1.5 mm subcrestally, so that the implant collar lay 3 mm apical to the collar of the removable overdenture teeth. The design of the Axiom X3® implant limits insertion-related stresses in the bone and thus favors bone preservation. In this clinical situation of average bone density, the Axiom X3® drilling protocol is shortened without the need to use the final drill. Final insertion of each implant was carried out by hand using the ratchet wrench and primary stability was correct.
6a-b. Hand-tightening of Ø 4 mm healing screws for the incisors and Ø 5 mm healing screws for the premolars.
7a-b. Connective tissue grafts were placed vestibularly to offset ridge resorption and maintain the papilla mesial to implants 12 and 22.
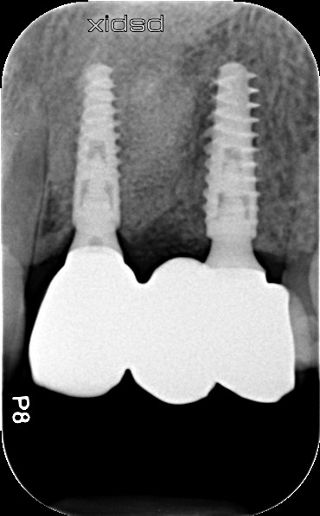
8a-b. 2 months follow-up. The healing screws were removed and replaced with Multi-Unit abutments. The abutments gingival height was 2.5 mm. 4 mm diameter abutments were used for lateral incisors and 4.8 mm platforms for the premolars. They were tightened to 25 N.cm. An initial impression was taken to prepare the temporary bridges.
9a-b. Temporary resin bridges were inserted with and without mock-ups on 11 and 21. Two veneers were envisaged to standardize the proportions of future restorations.
10. Impression taken with pick-up transfers. The transfers were connected in pairs with a rod and burnout resin. The preparations on teeth 11 and 21 were guided by the mock-up.
Prosthetic restoration:
11. Working model. Once the wax-up had been fabricated, the emergence profile was sculpted in the pink silicone to create a transition between the ideal neck of the ceramic crowns and the Multi-Unit abutments. As the soft tissue had been thickened and the implant collars sat away from the vestibular bone margin, compression would have no harmful effects. Note the interpupillary line marked on the model (Ditramax®). We used it as a reference.
12. State of the soft tissues 8 months after insertion of the implants and 6 months after wearing bridges. Soft tissue volume was satisfactory. A crown was fitted to tooth 15.
13.a-b. Although the soft tissue was healthy, the emergence profile was guided by the resin of the temporary crowns. This material is not ideal, even after polishing.
14a-b. Wax-up positioned the anatomical neck of each prosthetic element in the ideal position. The emergence profile was then created by adjusting the pink silicone.
15. Same emergence profile between resin and zirconia bridges. Enameling only on the vestibular surface. The zirconia was carefully polished where it contacted soft tissue.
16a-b. Final situation after inserting bridges to 15 Ncm, cementing the crown to tooth 15, and gluing the veneers to teeth 11 and 21.
16c. 4 years post implant placement.
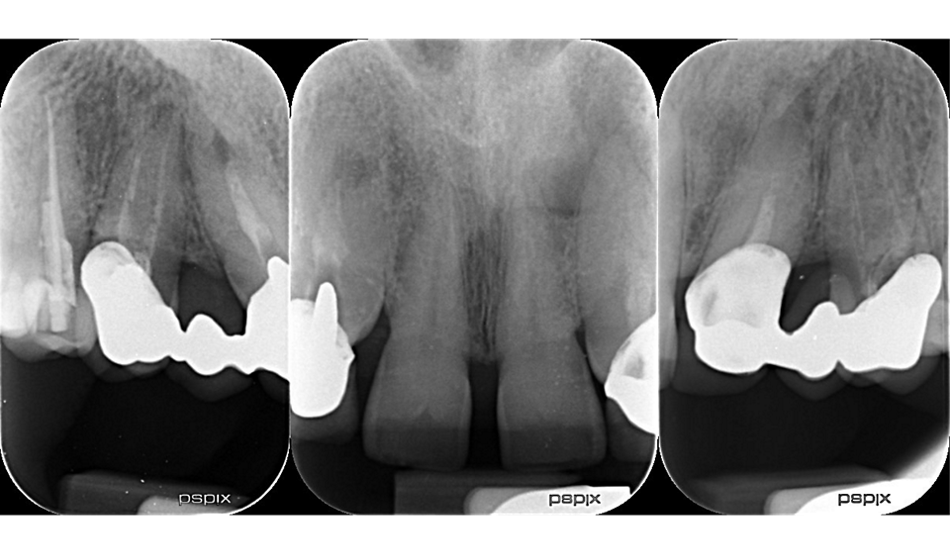
17a-b-c-d. Retro-alveolar X-rays at the end of treatment. Note bone behavior around the 4 implant collars. Soft tissue height above each collar was 3 to 4 mm.
Final situation:
18. Situation 4 years post implant placement.
Conclusion :
In this simple clinical situation, alveolar ridge preservation and alveolar bone filling made it possible to achieve favorable bone results. Post-extraction vestibular bone loss did not require bone volume augmentation and was offset by palatal connective tissue, which matured over the 6 months following the graft. The drilling sequence for Axiom X3® implants must be adapted to bone density, which is determined using an initial Ø 2 mm drill. In our patient the drilling protocol was adapted to D2-D3 bone, with the final drill being unnecessary. Indeed, the implant’s design reduces insertion torque in the bone and favors primary stability. The primary stability that we achieved would have allowed immediate loading of the temporary bridges, thereby shortening the always problematic period of wearing a removable overdenture by 2 months. However, the time required for the ossification of alveolar bone and maturation of soft tissue cannot be shortened.